Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule Extended Release, Oral:
Dilatrate-SR: 40 mg [contains fd&c yellow #10 (quinoline yellow)]
Tablet, Oral:
Isordil Titradose: 5 mg [scored; contains fd&c red #40]
Isordil Titradose: 40 mg [scored; contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Generic: 5 mg, 10 mg, 20 mg, 30 mg, 40 mg
Tablet Extended Release, Oral:
Generic: 40 mg [DSC]
Pharmacology
Mechanism of Action
Isosorbide dinitrate and other nitrates form free radical nitric oxide. In smooth muscle, nitric oxide activates guanylate cyclase which increases guanosine 3’5’ monophosphate (cGMP) leading to dephosphorylation of myosin light chains and smooth muscle relaxation. Produces a vasodilator effect on the peripheral veins and arteries with more prominent effects on the veins. Primarily reduces cardiac oxygen demand by decreasing preload (left ventricular end-diastolic pressure); may modestly reduce afterload. Additionally, coronary artery dilation improves collateral flow to ischemic regions.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: 2 to 4 L/kg
Metabolism
Extensively hepatic to conjugated active metabolites isosorbide 5-mononitrate and 2-mononitrate
Onset of Action
Sublingual tablet: ~2 to 5 minutes; Oral tablet and capsule (includes extended-release formulations): ~1 hour
Duration of Action
Sublingual tablet: 1 to 2 hours; Oral tablet and capsule (includes extended-release formulations): Up to 8 hours
Half-Life Elimination
Parent drug: ~1 hour; Metabolites (5-mononitrate: 5 hours; 2-mononitrate: 2 hours)
Use: Labeled Indications
Angina pectoris, prevention: Prevention of angina pectoris due to coronary artery disease.
Note: Due to slower onset of action, isosorbide dinitrate is not the drug of choice to abort an acute anginal episode.
Use: Off Label
Achalasiayes
Based on the American College of Gastroenterology (ACG) guidelines on the diagnosis and management of achalasia, isosorbide dinitrate may be considered for patients with achalasia who cannot use or refuse more definitive therapies (pneumatic dilation or surgical myotomy) and patients who have failed botulinum toxin injections.
Heart failure with reduced ejection fractionayes
Data from a randomized, double-blind trial comparing enalapril and hydralazine plus isosorbide dinitrate in patients with chronic heart failure support the use of isosorbide dinitrate (in combination with hydralazine) in patients with intolerance to ACE inhibitor therapy Cohn 1991. Data from a randomized, double-blind, placebo-controlled trial in black patients with NYHA class III or IV heart failure on optimal guideline-directed medical therapy support the use of isosorbide dinitrate (in combination with hydralazine) for the management of this condition Taylor 2004.
Based on the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines for the management of heart failure, isosorbide dinitrate (in combination with hydralazine) is effective and recommended as additional therapy to optimal guideline-directed medical therapy for self-identified African-American patients with persistent NYHA class III or IV heart failure with reduced ejection fraction (HFrEF) or for patients who do not tolerate an ACE inhibitor or an angiotensin II receptor blocker (ARB) ACC/AHA [Yancy 2013]. Some experts recommend isosorbide dinitrate (in combination with hydralazine) in addition to optimal guideline-directed medical therapy for black and nonblack patients with persistent NYHA class III or IV HFrEF, particularly for those with low output states or hypertension, or for patients who do not tolerate an ACE inhibitor, ARB, or angiotensin II-neprilysin inhibitor (ARNI) Colucci 2019.
Contraindications
Hypersensitivity to isosorbide dinitrate or any component of the formulation; concurrent use with phosphodiesterase inhibitors (sildenafil, tadalafil, vardenafil, or avanafil); concurrent use with riociguat
Canadian labeling: Additional contraindications (not in US labeling): Cardiogenic shock or risk of cardiogenic shock developing
Dosage and Administration
Dosing: Adult
Achalasia (off-label use): Sublingual: Immediate release: 5 mg administered 10 to 15 minutes before meals. Note: Clinical response is short acting and use does not provide complete relief of symptoms; consider risks before use (ACG [Vaezi 2013]).
Angina pectoris (prevention): Note: Due to slower onset of action, isosorbide dinitrate is not the drug of choice to abort an acute anginal episode. Tolerance to nitrate effects develops with chronic exposure; dose escalation does not overcome this effect. Tolerance can only be overcome by short periods of nitrate absence from the body. Nitrate-free intervals of ≥14 hours (immediate release products) or >18 hours (sustained release products) may help minimize tolerance.
Oral:
Immediate release: Initial: 5 to 20 mg 2 to 3 times daily; Maintenance: 10 to 40 mg 2 to 3 times daily or 5 to 80 mg 2 to 3 times daily (Anderson 2011)
Sustained release: 40 to 160 mg/day has been used in clinical trials (a nitrate free interval of >18 hours is recommended; however, a clinically efficacious dosage interval has not been clearly established) or 40 mg 1 to 2 times daily (Anderson 2011). Maximum dose: 160 mg/day (Dilatrate-SR only).
Sublingual [Canadian product]: 5 to 10 mg every 2 to 4 hours for prophylaxis of acute angina; may supplement with 5 to 10 mg prior to activities which may provoke an anginal episode.
Heart failure with reduced ejection fraction (off-label use): Note: As additional therapy for persistent NYHA class III or IV heart failure with reduced ejection fraction (HFrEF) despite optimal guideline directed medical therapies or for patients who cannot tolerate an ACE inhibitor, angiotensin II receptor blocker (ARB), or angiotensin II-neprilysin inhibitor (ARNI) (ACCF/AHA [Yancy 2013]; Colucci 2019).
Oral: Immediate release: Initial: 20 to 30 mg 3 or 4 times daily in combination with hydralazine 3 or 4 times daily; titrate dose every 2 to 4 weeks; maximum dose: 120 mg/day in divided doses (ACCF/AHA [Yancy 2013]). Some experts initiate 20 mg 3 times daily in combination with hydralazine 3 times daily; evaluate every 2 to 4 weeks and gradually titrate as tolerated to a target dose of 40 mg 3 times daily in combination with hydralazine 3 times daily (Colucci 2019; Meyer 2019). Note: May also consider use of the fixed-dose combination of isosorbide dinitrate/hydralazine instead of separate components (ACC/AHA/HFSA [Yancy 2017]; ACCF/AHA [Yancy 2013]).
Dosing: Geriatric
Elderly patients should be given lowest recommended adult daily doses initially and titrate upward. Refer to adult dosing.
Administration
Do not administer around the clock; allow nitrate-free interval ≥14 hours (immediate release products) and >18 hours (sustained release products). Do not chew or crush sublingual tablets or sustained release formulations.
Immediate release products: For twice daily dosing, consider administering at 8 AM and 1 PM. For 3 times daily dosing, consider 8 AM, 1 PM, and 6 PM.
Sustained release products: Consider once daily in morning or twice-daily dosing at 8 AM and between 1 PM and 2 PM.
Storage
Extended-release tablets: Store at 20°C to 25°C (68°F to 77°F).
Sustained-release capsules and immediate-release tablets: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light.
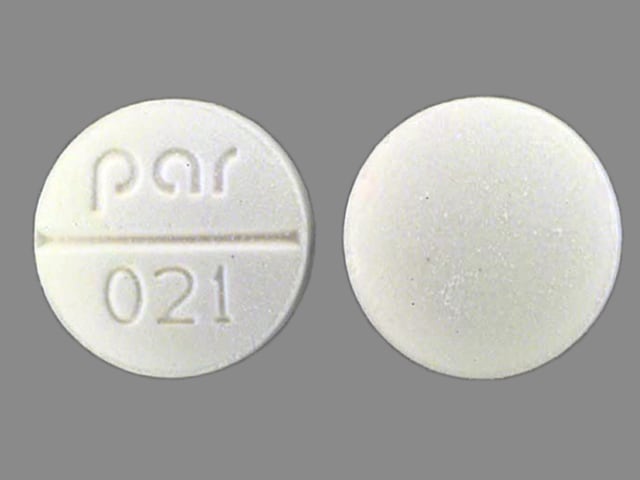
Isosorbide Dinitrate Images
Drug Interactions
Alcohol (Ethyl): May enhance the vasodilatory effect of Vasodilators (Organic Nitrates). Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapoxetine: May enhance the orthostatic hypotensive effect of Vasodilators (Organic Nitrates). Monitor therapy
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Molsidomine: May enhance the hypotensive effect of Vasodilators (Organic Nitrates). Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the vasodilatory effect of Vasodilators (Organic Nitrates). Avoid combination
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Rilmenidine: Vasodilators (Organic Nitrates) may enhance the hypotensive effect of Rilmenidine. Monitor therapy
Riociguat: Vasodilators (Organic Nitrates) may enhance the hypotensive effect of Riociguat. Avoid combination
Rosiglitazone: Vasodilators (Organic Nitrates) may enhance the adverse/toxic effect of Rosiglitazone. Specifically, a greater risk of ischemia and other adverse effects has been associated with this combination in some pooled analyses. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Adverse Reactions
Frequency not defined.
Cardiovascular: Hypotension, rebound hypertension, syncope, unstable angina pectoris
Central nervous system: Headache
Warnings/Precautions
Concerns related to adverse effects:
- Hypotension/bradycardia: Severe hypotension can occur; paradoxical bradycardia and increased angina pectoris can accompany hypotension. Orthostatic hypotension can also occur; ethanol can accentuate this. Use with caution in volume depletion and hypotension, and use with extreme caution with inferior wall MI and suspected right ventricular infarctions. Severe hypotension, particularly with upright posture, may occur with even small doses.
- Intracranial pressure increased: Nitrates may precipitate or aggravate increased intracranial pressure and subsequently may worsen clinical outcomes in patients with neurologic injury (eg, intracranial hemorrhage, traumatic brain injury) (Rangel-Castilla 2008).
Disease-related concerns:
- Cardiovascular disease: Not recommended in patients with acute MI or HF (cannot easily reverse effects if adverse events develop).
- Hypertrophic cardiomyopathy (HCM): Avoid use in patients with HCM with outflow tract obstruction; nitrates may reduce preload, exacerbating obstruction and cause hypotension or syncope and/or worsening of heart failure (ACCF/AHA [Gersh 2011]).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Tolerance: Appropriate dosing intervals are needed to minimize tolerance development. Tolerance can only be overcome by short periods of nitrate absence from the body. Dose escalation does not overcome this effect. When used for HF in combination with hydralazine, tolerance is less of a concern (Gogia 1995).
Monitoring Parameters
Blood pressure, heart rate
Pregnancy
Pregnancy Considerations
Adverse events have been observed in some animal reproduction studies. Nitric oxide donors, such as isosorbide, have been evaluated for pre-eclampsia and cervical ripening; isosorbide dinitrate use in these conditions is not currently recommended (Kalidindi 2012; Ramirez 2011).
Patient Education
What is this drug used for?
- It is used to prevent chest pain.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe dizziness
- Passing out
- Slow heartbeat
- Fast heartbeat
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.