Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Solution, Intravenous [preservative free]:
Vimpat: 200 mg/20 mL (20 mL)
Solution, Oral:
Vimpat: 10 mg/mL (200 mL, 465 mL) [contains aspartame, methylparaben, polyethylene glycol, propylene glycol; strawberry flavor]
Tablet, Oral:
Vimpat: 50 mg [contains fd&c blue #2 aluminum lake]
Vimpat: 100 mg, 150 mg
Vimpat: 200 mg [contains fd&c blue #2 aluminum lake]
Pharmacology
Mechanism of Action
In vitro studies have shown that lacosamide stabilizes hyperexcitable neuronal membranes and inhibits repetitive neuronal firing by enhancing the slow inactivation of sodium channels (with no effects on fast inactivation of sodium channels).
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Completely
Distribution
Vd: ~0.6 L/kg
Metabolism
Hepatic via CYP3A4, CYP2C9, and CYP2C19; forms metabolite, O-desmethyl-lacosamide (inactive)
Excretion
Urine (95%; 40% as unchanged drug, 30% as inactive metabolite, 20% as uncharacterized metabolite); feces (<0.5%)
Time to Peak
Oral: 1-4 hours
Half-Life Elimination
Children ≥4 years and Adolescents:
Mean weight 11 kg: 7.4 hours
Mean weight 28.9 kg: 10.6 hours
Mean weight 70 kg: 14.8 hours
Adults: ~13 hours
Protein Binding
<15%
Use in Specific Populations
Special Populations: Renal Function Impairment
AUC is increased ~25% in patients with mild or moderate renal impairment (CrCl >30 to 80 mL/minute) and 60% in patients with severe renal impairment (CrCl ≤30 mL/minute). Following a 4-hour hemodialysis treatment, AUC is reduced by ~50%.
Special Populations: Hepatic Function Impairment
AUC is increased by ~50% to 60% in patients with moderate hepatic impairment (Child-Pugh class B).
Special Populations: Elderly
In patients >65 years of age, AUC and Cmax are increased ~20% compared with younger subjects.
Use: Labeled Indications
Focal (partial) onset seizures: Monotherapy or adjunctive therapy in the treatment of focal (partial) onset seizures in children ≥4 years of age and adults.
Use: Off Label
Status epilepticus, refractorycyes
Data from case reports, retrospective studies, prospective observational studies, and a randomized pilot study in patients with refractory status epilepticus suggest that lacosamide may be beneficial for the treatment of patients with refractory status epilepticus, though the results are mixed Albers 2011, Goodwin 2011, Kellinghaus 2011, Misra 2017, Newey 2017, Sutter 2013. Additional data may be necessary to further define the role of lacosamide in the treatment of patients with refractory status epilepticus.
Based on the Neurocritical Care Society Guidelines for the Evaluation and Management of Status Epilepticus, the use of lacosamide is an effective and recommended treatment for refractory status epilepticus in adults although there is limited clinical experience in this setting.
Contraindications
US labeling: There are no contraindications listed in manufacturer's labeling.
Canadian labeling: Hypersensitivity to lacosamide or any component of the formulation; second- or third-degree atrioventricular (AV) block (current or history of).
Dosage and Administration
Dosing: Adult
Focal (partial) onset seizure:
Monotherapy: Oral, IV:
Initial: 100 mg twice daily; may be increased at weekly intervals by 50 mg twice daily based on response and tolerability.
Alternative initial dosage: Loading dose: 200 mg followed approximately 12 hours later by 100 mg twice daily for 1 week; may be increased at weekly intervals by 50 mg twice daily based on response and tolerability. Note: Administer loading doses under medical supervision because of the increased incidence of CNS adverse reactions.
Maintenance: 150 to 200 mg twice daily; a further increase up to 300 mg twice daily may be needed in some patients for optimal response (Baulac 2017). Note: For patients already on a single antiepileptic and converting to lacosamide monotherapy, maintain the maintenance dose for 3 days before beginning withdrawal of the concomitant antiepileptic drug. Gradually taper the concomitant antiepileptic drug over ≥6 weeks.
Adjunctive therapy: Oral, IV:
Initial: 50 mg twice daily; may be increased at weekly intervals by 50 mg twice daily based on response and tolerability.
Alternative initial dosage: Loading dose of 200 mg followed approximately 12 hours later by 100 mg twice daily for 1 week; may be increased at weekly intervals by 50 mg twice daily based on response and tolerability. Note: Administer loading doses under medical supervision because of the increased incidence of CNS adverse reactions.
Maintenance dose: 100 to 200 mg twice daily. Note: Doses up to 600 mg/day may provide additional benefit in some patients (eg, with secondary generalized tonic-clonic seizures) based on clinical trials with oral formulations; however, risk of adverse effects is greater (Ben-Menachem 2007; Chung 2010).
Status epilepticus, refractory (off-label use): IV: 200 to 400 mg followed by a daily maintenance dose of 200 to 400 mg daily in 2 divided doses (Misra 2017; NCS [Brophy 2012]; Newey 2017; Sutter 2013); some patients may require up to 600 mg/day for optimal response (Strzelczyk 2017). Note: The Neurocritical Care Society recommends an administration rate of 200 mg over 15 minutes; however, some experts administer IV push or infusion doses up to 400 mg at a rate of ≤80 mg/minute (Davidson 2018; Kellinghaus 2011; NCS [Brophy 2012]).
Dosing conversion: Between oral and IV dosing: Convert using same total daily dose. Use IV therapy only temporarily; clinical trial experience of IV lacosamide is limited to 5 days of consecutive treatment.
Discontinuation of therapy: In patients receiving lacosamide long term, unless safety concerns require a more rapid withdrawal, lacosamide should be withdrawn gradually over a few weeks to several months to minimize the potential of seizures or other withdrawal symptoms (Schachter 2019).
Dosing: Geriatric
Refer to adult dosing; use caution during dose titration.
Dosing: Pediatric
Seizure, partial onset: Note: For patients already on a single antiepileptic and converting to lacosamide monotherapy, maintain the maintenance dose for 3 days before beginning withdrawal of the concomitant antiepileptic drug. Gradually taper the concomitant antiepileptic drug over ≥6 weeks.
Children ≥4 to 17 years:
Monotherapy and adjunctive therapy:
11 to <30 kg: Oral:
Initial: 1 mg/kg/dose twice daily; may be increased at weekly intervals by 1 mg/kg/dose twice daily based on response and tolerability
Maintenance: 3 to 6 mg/kg/dose twice daily
30 to <50 kg: Oral:
Initial: 1 mg/kg/dose twice daily; may be increased at weekly intervals by 1 mg/kg/dose twice daily based on response and tolerability
Maintenance: 2 to 4 mg/kg/dose twice daily
≥50 kg: Oral:
Initial (monotherapy and adjunctive therapy): 50 mg twice daily; may be increased at weekly intervals of 50 mg twice daily based on response and tolerability
Maintenance:
Monotherapy: 150 to 200 mg twice daily
Adjunctive therapy: 100 to 200 mg twice daily. Note: In adjunctive clinical trials in adults, doses higher than 400 mg/day were not more effective and were associated with more adverse reactions.
Adolescents ≥17 years: Note: When switching from oral to IV formulations, the total daily dose and frequency should be the same; IV therapy should only be used temporarily. Clinical study experience of IV lacosamide is limited to 5 days of consecutive treatment.
Monotherapy: Oral, IV:
Initial: 100 mg twice daily; may be increased at weekly intervals by 50 mg twice daily based on response and tolerability
Alternate initial dosage: Loading dose: 200 mg followed approximately 12 hours later by 100 mg twice daily for 1 week; may be increased at weekly intervals by 50 mg twice daily based on response and tolerability. Note: Administer loading doses under medical supervision because of the increased incidence of CNS adverse reactions.
Maintenance: 150 to 200 mg twice daily. Note: In adjunctive clinical trials in adults, doses higher than 400 mg/day were not more effective and were associated with more adverse reactions.
Adjunctive therapy: Oral, IV:
Initial: 50 mg twice daily; may be increased at weekly intervals by 50 mg twice daily based on response and tolerability
Alternative initial dosage: Loading dose of 200 mg followed approximately 12 hours later by 100 mg twice daily for 1 week; may be increased at weekly intervals by 50 mg twice daily based on response and tolerability. Note: Administer loading doses under medical supervision because of the increased incidence of CNS adverse reactions.
Maintenance dose: 100 to 200 mg twice daily. Note: In adjunctive clinical trials in adults, doses higher than 400 mg/day were not more effective and were associated with more adverse reactions.
Seizure, severe; refractory: Limited data available: Infants ≥6 months, Children, and Adolescents <17 years: Oral: Initial: 1 to 2 mg/kg/day divided twice daily (usual maximum initial dose: 50 mg/dose); may titrate by 1 to 2 mg/kg/day weekly to effect. Range of reported mean maintenance doses: 4.7 to 15.2 mg/kg/day. Dosing based on large prospective, open label trials, small retrospective trials and case series; reported experience is primarily as adjunctive therapy with a few pediatric patients receiving monotherapy (Casas-Fernández 2012; Gavatha 2011; Grosso 2014a; Grosso 2014b; Guilhoto 2011; Heyman 2012; Kim 2014; Kliegman 2015; Rastogi 2012; Verrotti 2013; Yorns 2014). In the largest, multicenter, prospective trial of 130 pediatric patients (mean age: 8.01 ± 4.25 years; range: 6 months to 16 years) with refractory focal seizures, therapy was initiated at 1 to 2 mg/kg/day divided twice daily and titrated by 1 or 2 mg/kg/day increments to effect; mean reported dose was 6.8 ± 2.39 mg/kg (effective dose range: 2.14 to 14.3 mg/kg/day); after 3 months of therapy, 62.3% of patients had a >50% decrease in seizure frequency, including 16.2% who became seizure free; five patients withdrew due to adverse effects. While doses as high as 20 mg/kg/day were reported in this study, this was isolated to the group of subjects that reported no decrease in seizure frequency during therapy (Casas-Fernández 2012). In another large prospective trial of 59 pediatric patients (mean age: 10.8 ± 3.14 years; range: 4 to 15 years) with focal, general, or mixed seizure types, therapy was initiated at 1 mg/kg/day, titrating weekly by 1 mg/kg/day increments to a target dose of 3 to 12 mg/kg/day; after 3 months of therapy (n=59), 47.4% of patients had a ≥50% decrease in seizure frequency, 6.8% were seizure free, 11.9% reported an increase in seizure frequency, and two patients withdrew due to adverse effects; at 6-month follow up (n=50), 52.5% had a ≥50% decrease in seizure frequency and four patients withdrew due to lack of efficacy and at 12-month follow-up (n=46), 47.4% had a ≥50% decrease in seizure frequency (Verrotti 2013).
Reconstitution
Injection: May be mixed with compatible diluents (NS, LR, D5W) in glass or PVC.
Administration
IV:
Infusion: Administer over 15 to 60 minutes; infusions over 30 to 60 minutes are preferred to minimize adverse effects. IV administration has been used for up to 5 days. Can be administered without further dilution or may be mixed with compatible diluents (NS, LR, D5W).
Bolus (off label): Doses up to 400 mg may be administered undiluted at ≤80 mg/minute (Davidson 2018; Kellinghaus 2011).
Oral solution, tablets: May be administered with or without food. Oral solution should be administered with a calibrated measuring device (not a household teaspoon or tablespoon). Oral solution may also be administered via a nasogastric or gastrostomy tube. Swallow tablets whole; do not divide.
Dietary Considerations
Some products may contain phenylalanine.
Storage
Injection: Store at 20°C to 25°C (68°F to 77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Do not freeze. Stable when mixed with compatible diluents (NS, LR, D5W) for up to 4 hours at room temperature; extended storage information for prepared solution at room temperature may be available; contact product manufacturer to obtain current recommendations. Discard any unused portion.
Oral solution, tablets: Store at 20°C to 25°C (68°F to 77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F). Do not freeze oral solution. Discard any unused portion of oral solution after 7 weeks.
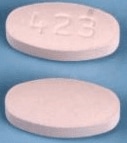
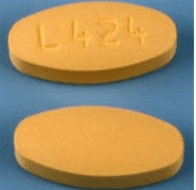
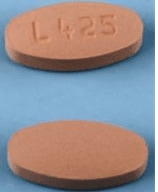
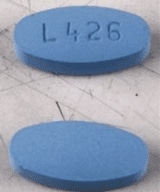
Lacosamide Images
Drug Interactions
Antiarrhythmic Agents (Class III): May enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
Antiepileptic Agents (Sodium Channel Blockers): May enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
Bradycardia-Causing Agents: May enhance the AV-blocking effect of Lacosamide. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Lacosamide. Monitor therapy
Lidocaine (Systemic): May enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Mexiletine: May enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
Mianserin: May diminish the therapeutic effect of Anticonvulsants. Monitor therapy
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
QT-prolonging Class IA Antiarrhythmics (Highest Risk): May enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): May enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
Adverse Reactions
>10%:
Central nervous system: Dizziness (16% to 30%), headache (11% to 14%)
Gastrointestinal: Nausea (7% to 11%)
1% to 10%:
Central nervous system: Drowsiness (8%), fatigue (7%), ataxia (4% to 7%), vertigo (3% to 5%), equilibrium disturbance (1% to 5%), abnormal gait (2%), depression (2%)
Dermatologic: Pruritus (2% to 3%)
Gastrointestinal: Vomiting (6% to 9%), diarrhea (5%)
Hematologic & oncologic: Bruise (4%)
Local: Pain at injection site (IV: 3%), local irritation (IV: 1%)
Neuromuscular & skeletal: Tremor (6%), asthenia (2%)
Ophthalmic: Diplopia (6% to 10%), blurred vision (9%), nystagmus (5%)
Miscellaneous: Laceration (3%)
Frequency not defined:
Cardiovascular: Palpitations, syncope
Central nervous system: Cerebellar syndrome, cognitive dysfunction, confusion, disturbance in attention, dysarthria, falling, hypoesthesia, intoxicated feeling, irritability, mood changes, paresthesia, suicidal ideation, suicidal tendencies
Gastrointestinal: Constipation, dyspepsia, oral hypoesthesia, xerostomia
Hematologic & oncologic: Anemia, neutropenia
Neuromuscular & skeletal: Muscle spasm
Otic: Tinnitus
Miscellaneous: Fever
<1%, postmarketing, and/or case reports: Abnormal hepatic function tests, acute psychosis, aggressive behavior, agitation, agranulocytosis, angioedema, atrial fibrillation, atrial flutter, atrioventricular block, bradycardia, cardiac arrhythmia, DRESS syndrome, erythema at injection site, euphoria, first degree atrioventricular block, hallucination, hepatitis, increased serum alanine aminotransferase, insomnia, nephritis, prolongation P-R interval on ECG, seizure, skin rash, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria, ventricular tachyarrhythmia
Warnings/Precautions
Concerns related to adverse effects:
- Cardiovascular effects: Lacosamide may prolong PR interval; cardiac arrhythmias, including bradycardia, AV block, and ventricular tachyarrhythmias have also been reported, which have rarely resulted in asystole, cardiac arrest, and death. Occurrence was more prevalent in patients with underlying proarrhythmic conditions or with concomitant use of medications that affect cardiac conduction or prolong the PR interval; events occurred with oral and IV administration. Use caution in patients with conduction problems (eg, first/second degree atrioventricular block and sick sinus syndrome without pacemaker), sodium channelopathies (eg, Brugada syndrome), myocardial ischemia, heart failure, structural heart disease, or if concurrent use with other drugs that affect cardiac conduction and prolong the PR interval. In these patients, an ECG is recommended prior to initiating therapy and when at the steady state maintenance dose. Monitor closely with IV administration; bradycardia, AV block, or ventricular tachyarrhythmias may occur during infusions. Instruct patients to contact their healthcare provider if signs or symptoms of conduction problems occur (eg, low or irregular pulse, feeling of lightheadedness and fainting). During short-term trials, atrial fibrillation/flutter or syncope occurred slightly more often in patients with diabetic neuropathy and/or cardiovascular disease. In addition, in open-label studies, syncope has been associated with a history of cardiac disease risk factors and use of drugs that slow AV conduction.
- CNS effects: Dizziness and ataxia may occur during therapy; patients should be cautioned about performing tasks which require alertness (eg, operating machinery or driving).
- Multiorgan hypersensitivity reactions (drug reaction with eosinophilia and systemic symptoms [DRESS]): Potentially serious (sometimes fatal or life-threatening, possibly delayed) multiorgan hypersensitivity reactions have been reported with some antiepileptic drugs (rare), including lacosamide; monitor for signs and symptoms of possible disparate manifestations associated with lymphatic, hepatic, renal, and/or hematologic organ systems; gradual discontinuation and conversion to alternate therapy may be required.
- Ophthalmic effects: Blurred vision and diplopia may occur during therapy. Patients with persistent visual disturbances may need further assessment. Consider increased monitoring in patients with preexisting ocular conditions or vision-related issues.
- Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; notify health care provider immediately if symptoms occur.
Disease-related concerns:
- Hepatic impairment: Not recommended for use in patients with severe hepatic impairment; dosage adjustment required for mild to moderate hepatic impairment. Further dosage adjustment may be necessary in patients with hepatic impairment taking concomitant strong CYP3A4 and/or CYP2C9 inhibitors.
- Renal impairment: Use caution in patients with renal impairment; dosage adjustment required for severe renal impairment (CrCl ≤30 mL/minute) and supplementation may be necessary in hemodialysis. Patients with any degree of renal impairment taking concomitant strong CYP3A4 and/or CYP2C9 inhibitors may require dosage adjustment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Phenylalanine: Some products may contain phenylalanine.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures and respiratory depression; use caution (AAP 1997; Zar 2007).
Other warnings/precautions:
- Withdrawal: Anticonvulsants should not be discontinued abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually (≥1 week) to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal.
Monitoring Parameters
Patients with conduction problems, sodium channelopathies, severe cardiac disease, or concomitant medications that affect cardiac conduction or prolong PR interval should have ECG tracing prior to start of therapy and when at steady-state. Monitor these patients closely during IV infusions (bradycardia, AV block, or ventricular tachyarrhythmias may occur during infusions). Monitor for suicidality (eg, suicidal thoughts, depression, behavioral changes).
Pregnancy
Pregnancy Considerations
Lacosamide crosses the placenta (Ylikotila 2015; Zárubová 2016).
Due to pregnancy-induced physiologic changes, some pharmacokinetic properties of lacosamide may be altered (Zárubová 2016). Information related to pregnancy outcomes following maternal use of lacosamide is limited (Hoeltzenbein 2011; Lattanzi 2017; Zárubová 2016). In general, maternal polytherapy with antiepileptic drugs may increase the risk of congenital malformations; monotherapy with the lowest effective dose is recommended. Newborns of women taking antiepileptic medications may be at an increased risk of adverse events (Harden 2009).
Patients exposed to lacosamide during pregnancy are encouraged to enroll themselves into the North American Antiepileptic Drug (NAAED) Pregnancy Registry by calling 1-888-233-2334. Additional information is available at http://www.aedpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used to treat seizures.
Frequently reported side effects of this drug
- Fatigue
- Loss of strength and energy
- Headache
- Blurred vision
- Nausea
- Vomiting
- Diarrhea
- Dry mouth
- Sweating a lot.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, emotional instability, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Change in balance
- Trouble with memory
- Severe dizziness
- Passing out
- Slow heartbeat
- Fast heartbeat
- Abnormal heartbeat
- Tremors
- Double vision
- Shortness of breath
- Swollen glands
- Chest pain
- Burning or numbness feeling
- Involuntary eye movements
- Unable to pass urine
- Change in amount of urine passed
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.