Boxed Warning
Serious skin rashes:
Lamotrigine can cause serious rashes requiring hospitalization and discontinuation of treatment. The incidence of these rashes, which have included Stevens-Johnson syndrome, is approximately 0.3% to 0.8% in pediatric patients (2 to 17 years of age) and 0.08% to 0.3% in adults receiving lamotrigine. One rash-related death was reported in a prospectively followed cohort of 1,983 pediatric patients (2 to 16 years of age) with epilepsy taking lamotrigine immediate-release as adjunctive therapy. In worldwide postmarketing experience, rare cases of toxic epidermal necrolysis and/or rash-related death have been reported in adults and pediatric patients, but those numbers are too few to permit a precise estimate of the rate.
The risk of serious rash caused by treatment with lamotrigine ER is not expected to differ from that with the immediate-release formulation of lamotrigine. However, the relatively limited treatment experience with lamotrigine ER makes it difficult to characterize the frequency and risk of serious rashes caused by treatment with lamotrigine ER.
Other than age, there are as yet no factors identified that are known to predict the risk of occurrence or the severity of rash caused by lamotrigine. There are suggestions, yet to be proven, that the risk of rash may also be increased by coadministration of lamotrigine with valproate (includes valproic acid and divalproex sodium), exceeding the recommended initial dose of lamotrigine, or exceeding the recommended dose escalation for lamotrigine. However, cases have been reported in the absence of these factors.
Nearly all cases of life-threatening rashes caused by lamotrigine have occurred within 2 to 8 weeks of treatment initiation. However, isolated cases have been reported after prolonged treatment (eg, 6 months). Accordingly, duration of therapy cannot be relied upon as a means to predict the potential risk heralded by the first appearance of a rash.
Although benign rashes are also caused by lamotrigine, it is not possible to predict reliably which rashes will prove to be serious or life-threatening. Accordingly, lamotrigine should ordinarily be discontinued at the first sign of rash unless the rash is clearly not drug-related. Discontinuation of treatment may not prevent a rash from becoming life-threatening or permanently disabling or disfiguring.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Kit, Oral:
LaMICtal ODT: Blue Kit: 25 mg (21s) & 50 mg (7s), Orange Kit: 25 mg (14s) & 50 mg (14s) & 100 mg (7s), Green Kit: 50 mg (42s) & 100 mg (14s)
LaMICtal Starter: Blue Kit: 25 mg (35s)
LaMICtal Starter: Green Kit: 25 mg (84s) & 100 mg (14s), Orange Kit: 25 mg (42s) & 100 mg (7s) [contains fd&c yellow #6 aluminum lake]
LaMICtal XR: Green Kit: 50 mg (14s) & 100 mg (14s) & 200 mg (7s) [contains fd&c blue #2 aluminum lake, polysorbate 80]
LaMICtal XR: Blue Kit: 25 mg (21s) & 50 mg (7s), Orange Kit: 25 mg (14s) & 50 mg (14s) & 100 mg (7s) [contains polysorbate 80]
Subvenite Starter Kit-Blue: Blue Kit: 25 mg (35s)
Subvenite Starter Kit-Green: Green Kit: 25 mg (84s) & 100 mg (14s)
Subvenite Starter Kit-Orange: Orange Kit: 25 mg (42s) & 100 mg (7s)
Generic: Blue Kit: 25 mg (21s) & 50 mg (7s) [DSC], Blue Kit: 25 mg (35s), Green Kit: 25 mg (84s) & 100 mg (14s), Green Kit: 50 mg (42s) & 100 mg (14s) [DSC], Orange Kit: 25 mg (14s) & 50 mg (14s) & 100 mg (7s) [DSC], Orange Kit: 25 mg (42s) & 100 mg (7s)
Tablet, Oral:
LaMICtal: 25 mg [scored]
LaMICtal: 100 mg [scored; contains fd&c yellow #6 aluminum lake]
LaMICtal: 150 mg [scored]
LaMICtal: 200 mg [scored; contains fd&c blue #2 (indigotine)]
Subvenite: 25 mg, 100 mg, 150 mg, 200 mg [scored]
Generic: 25 mg, 100 mg, 150 mg, 200 mg
Tablet Chewable, Oral:
LaMICtal: 5 mg [scored; berry flavor]
LaMICtal: 25 mg [berry flavor]
Generic: 5 mg, 25 mg
Tablet Disintegrating, Oral:
LaMICtal ODT: 25 mg, 50 mg, 100 mg, 200 mg
Generic: 25 mg, 50 mg, 100 mg, 200 mg
Tablet Extended Release 24 Hour, Oral:
LaMICtal XR: 25 mg, 50 mg, 100 mg [contains polysorbate 80]
LaMICtal XR: 200 mg [contains fd&c blue #2 aluminum lake, polysorbate 80]
LaMICtal XR: 250 mg [contains fd&c blue #2 aluminum lake]
LaMICtal XR: 300 mg [contains polysorbate 80]
Generic: 25 mg, 50 mg, 100 mg, 200 mg, 250 mg, 300 mg
Pharmacology
Mechanism of Action
A triazine derivative which inhibits release of glutamate (an excitatory amino acid) and inhibits voltage-sensitive sodium channels, which stabilizes neuronal membranes. Lamotrigine has weak inhibitory effect on the 5-HT3 receptor; in vitro inhibits dihydrofolate reductase.
Pharmacokinetics/Pharmacodynamics
Absorption
Immediate release: Rapid and complete, 97.6% absorbed; Note: Orally disintegrating tablets (either swallowed whole with water or disintegrated in the mouth) are equivalent to regular tablets (swallowed whole with water) in terms of rate and extent of absorption.
Distribution
Vd: 1.1 L/kg; range: 0.9 to 1.3 L/kg
Metabolism
Hepatic and renal; >75% metabolized via glucuronidation; autoinduction may occur
Excretion
Urine (94%, ~90% as glucuronide conjugates and ~10% unchanged); feces (2%)
Time to Peak
Plasma: Immediate release: 1 to 5 hours (dependent on adjunct therapy); Extended release: 4 to 11 hours (dependent on adjunct therapy)
Half-Life Elimination
Pediatric patients:
No concomitant enzyme-inducing AED (ie, phenytoin, phenobarbital, carbamazepine, primidone): Infants and Children 10 months to 5 years: 19 hours (range: 13 to 27 hours)
Concomitant valproate derivative therapy:
Infants and Children 10 months to 5 years: 45 hours (range: 30 to 52 hours)
Children 5 to 11 years: 66 hours (50 to 74 hours)
Concomitant enzyme-inducing AEDs (ie, phenytoin, phenobarbital, carbamazepine, primidone):
Infants and Children 10 months to 5 years: 7.7 hours (range: 6 to 11 hours)
Children 5 to 11 years: 7 hours (range: 4 to 10 hours)
Concomitant enzyme-inducing AEDs plus valproate derivative therapy: Children 5 to 11 years: 19 hours (range: 7 to 31 hours)
Adults:
Immediate release: 25 to 33 hours, Elderly: 25 to 43 hours; Extended release: Similar to immediate release
Concomitant valproic acid therapy: 48 to 70 hours
Concomitant phenytoin, phenobarbital, primidone, or carbamazepine therapy: 13 to 14 hours
Concomitant phenytoin, phenobarbital, primidone, or carbamazepine plus valproate therapy: 27 hours
Chronic renal failure: 43 hours
Hemodialysis: 13 hours during dialysis; 57 hours between dialysis (~20% of a dose is eliminated in a 4-hour dialysis session)
Hepatic impairment:
Mild: 46 ± 20 hours
Moderate: 72 ± 44 hours
Severe without ascites: 67 ± 11 hours
Severe with ascites: 100 ± 48 hours
Protein Binding
~55% (primarily albumin)
Use in Specific Populations
Special Populations: Elderly
Clearance was 0.3 to 0.5 mL/minute/kg.
Special Populations: Gender
Mean trough concentrations were 24% to 45% higher in women than men.
Special Populations: Race
Oral clearance was 25% lower in nonwhite patients than in white patients.
Use: Labeled Indications
Bipolar disorder: Maintenance treatment of bipolar disorder to delay the time to occurrence of mood episodes (depression, mania, hypomania, mixed episodes), as monotherapy or adjunctive therapy.
Focal (partial) onset seizures and generalized onset seizures: Treatment of Lennox-Gastaut syndrome (adjunctive therapy only), primary generalized tonic-clonic seizures (adjunctive therapy only), and focal onset seizures (monotherapy or adjunctive therapy). May be used off-label for other seizure types.
Use: Off Label
Bipolar major depressionbyes
Data from 4 meta-analyses support the use of lamotrigine in the acute treatment of bipolar major depression; however, the effects are modest, especially for severely depressed patients Geddes 2009, Selle 2014, Taylor 2014, Vieta 2010.
Based on the World Federation of Societies of Biological Psychiatry guidelines on the treatment of acute bipolar depression, lamotrigine may be effective and is suggested (particularly in severely depressed patients) as monotherapy or in combination with lithium in patients who are non- or partially responsive to other therapies WFSBP [Grunze 2010]. In contrast, according to the Canadian Network for Mood and Anxiety Treatments and International Society for Bipolar Disorders guidelines for the management of patients with bipolar disorder, lamotrigine is effective for acute bipolar depression, and monotherapy is recommended as a first-line option. Combination therapy with lithium is recommended as a second-line option. In addition, for acute bipolar II depression, monotherapy with lamotrigine is recommended as a second-line option despite conflicting evidence CANMAT/ISBD [Yatham 2018].
Short-lasting unilateral neuralgiform headache attacks, prophylaxiscyes
Data from a limited number of patients studied suggest that prophylactic lamotrigine may decrease severity and frequency of short-lasting unilateral neuralgiform headache attacks Cohen 2007, Williams 2008.
Based on the European Federation of Neurological Societies guidelines on the treatment of cluster headache and other trigeminal-autonomic cephalalgias, prophylactic lamotrigine is possibly effective for short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing EFNS [May 2006].
Contraindications
Hypersensitivity (eg, rash, angioedema, acute urticaria, extensive pruritus, mucosal ulceration) to lamotrigine or any component of the formulation
Dosage and Administration
Dosing: Adult
Note: Severe hypersensitivity reactions: Adhere strictly to recommended initial dose, titration schedules, and adjustments to reduce the risk of severe, including potentially fatal, cutaneous reactions and other hypersensitivity reactions. Adjustments for concomitant medications: Significant dose adjustments are required if used with valproate (which inhibits lamotrigine metabolism) or drugs that induce lamotrigine metabolism. Use drug interactions program for additional information. Formulations: Lamotrigine is available as immediate-release (IR) and extended-release (ER) formulations. Dosing recommendations are expressed as the total daily dose (ie, per 24 hours) unless stated otherwise. The IR tablets and compounded suspension (not commercially available) are dosed once daily when the total daily dose is ≤25 mg, and twice daily if the total daily dose is >25 mg. ER tablets are dosed once daily.
Bipolar disorder, maintenance treatment (labeled use) and acute bipolar major depression (alternative agent; off-label use): Note: Not effective for treating acute bipolar mania or hypomania (Cipriani 2011).
Patients not taking interacting medications: Oral: Initial: Weeks 1 and 2: 25 mg/day; increase based on response and tolerability as follows: Weeks 3 and 4: 50 mg/day; Week 5: 100 mg/day; Week 6: 200 mg/day (recommended maximum dose per manufacturer's labeling); however, further increases up to 400 mg/day may be necessary in some patients for optimal response (Geddes 2009; Shelton 2019). Some experts titrate more gradually (ie, by 25 to 50 mg/day each week) from week 5 until effective maintenance (or maximum) dose is reached (Shelton 2019).
Patients taking valproate (inhibits lamotrigine metabolism): Oral: Initial: Weeks 1 and 2: 25 mg every other day; increase based on response and tolerability as follows: Weeks 3 and 4: 25 mg/day; Week 5: 50 mg/day; Week 6 and maintenance: 100 mg/day.
Patients taking drug(s) that induce lamotrigine metabolism (eg, carbamazepine, phenytoin, others) but not taking valproate: Note: Estrogen derivatives (including hormonal contraceptives) induce lamotrigine metabolism but separate recommendations apply. See manufacturer's labeling for specific dosing recommendations with estrogen derivatives.
Oral: Initial: Weeks 1 and 2: 50 mg/day; increase based on response and tolerability as follows: Weeks 3 and 4: 100 mg/day; Week 5: 200 mg/day; Week 6: 300 mg/day; Maintenance: ≤400 mg/day.
Discontinuation of concomitant interacting therapy (eg, discontinuing valproate or carbamazepine): Note: Gradual adjustments may decrease risk of serious cutaneous hypersensitivity reactions, loss of control of bipolar disorder, and withdrawal symptoms. The following recommendations are based on manufacturer labeling; alterations may be needed based on clinical response and other factors.
Valproate and other inhibitors of lamotrigine metabolism: Discontinue valproate (or other inhibitor) and begin to increase the dose of lamotrigine, with the goal of doubling the dose of lamotrigine over a 2-week interval (using equal weekly increments) based upon response, to a recommended maximum dose of 200 mg/day.
Inducers of lamotrigine metabolism (eg, carbamazepine, phenytoin, others): Note: Estrogen derivatives (including hormonal contraceptives) induce lamotrigine metabolism, but separate recommendations apply. See manufacturer's labeling for recommendations for discontinuation of estrogen derivatives.
Discontinue the inducer drug and keep lamotrigine dose unchanged for 1 week, then decrease lamotrigine dose by one-half over a 2-week interval (using equal weekly increments). After 2 weeks, may adjust lamotrigine dose as needed based on response and tolerability to a recommended maximum dose of 200 mg/day.
Focal (partial) onset seizures and generalized onset seizures: Note: FDA-approved for Lennox-Gastaut syndrome (adjunctive therapy only), primary generalized tonic-clonic seizures (adjunctive therapy only), and focal onset seizures (monotherapy or adjunctive therapy); may be used off-label for other seizure types.
Patients not taking interacting medications: Oral: Initial: Weeks 1 and 2: 25 mg/day; increase based on response and tolerability as follows: Weeks 3 and 4: 50 mg/day; Week 5 and beyond: increase by 50 mg/day every 1 to 2 weeks. Usual maintenance dose: 225 to 375 mg/day (immediate release) or 300 to 400 mg/day (extended release).
Patients taking valproate (inhibits lamotrigine metabolism): Oral: Initial: Weeks 1 and 2: 12.5 to 25 mg every other day; increase based on response and tolerability as follows: Weeks 3 and 4: 25 mg/day; Week 5 and beyond: increase by 25 to 50 mg/day every 1 to 2 weeks. Usual maintenance dose: 100 to 200 mg/day (immediate release) or 200 to 250 mg/day (extended release). In patients taking both valproate and a drug that induces lamotrigine metabolism, the usual maintenance dose range is 100 to 400 mg/day (immediate release) (Schachter 2019; manufacturer's labeling).
Patients taking drug(s) that induce lamotrigine metabolism (eg, carbamazepine, phenytoin, others) but not taking valproate: Note: Estrogen derivatives (including hormonal contraceptives) induce lamotrigine metabolism, but separate recommendations apply. See manufacturer's labeling for dosing recommendations with estrogen derivatives.
Oral: Initial: Weeks 1 and 2: 50 mg/day; increase based on response and tolerability as follows: Weeks 3 and 4: 100 mg/day; Week 5 and beyond: increase by 100 mg/day every 1 to 2 weeks. Usual maintenance dose: 300 to 500 mg/day (immediate release) or 400 to 600 mg/day (extended release).
Discontinuation of concomitant interacting therapy: Note: Gradual adjustments may decrease the risk of serious cutaneous hypersensitivity reactions, loss of seizure control, and withdrawal symptoms. The following recommendations are based on manufacturer labeling; alterations may be needed based on clinical response and other factors.
For discontinuation of valproate and other inhibitors of lamotrigine metabolism:
Immediate release:
- Step 1: Gradually increase lamotrigine dose to 200 mg/day following standard escalation schedule for cotherapy with valproate. Maintain current valproate dose.
- Step 2: While maintaining lamotrigine 200 mg/day, decrease valproate dose in decrements of ≤500 mg/day once every week to a dose of 500 mg/day; maintain this valproate dosage for 1 week.
- Step 3: If needed based on response and tolerability, increase lamotrigine to 300 mg/day while simultaneously decreasing valproate to 250 mg/day; maintain both dosing regimens for 1 week.
- Step 4: Discontinue valproate. Increase lamotrigine as needed based on response and tolerability in increments of 100 mg/day every week to maintenance dose range for no interacting medications (manufacturer's labeling suggests ≤500 mg/day).
Extended release:
- Step 1: Gradually increase lamotrigine dose to 150 mg/day following standard escalation schedule for cotherapy with valproate. Maintain current valproate dose.
- Step 2: While maintaining lamotrigine dose of 150 mg/day, decrease valproate dose in decrements of ≤500 mg/day once every week to a dose of 500 mg/day; maintain this valproate dosage for 1 week.
- Step 3: If needed based on response and tolerability, increase lamotrigine to 200 mg/day while simultaneously decreasing valproate to 250 mg/day; maintain both dosing regimens for 1 week.
- Step 4: Discontinue valproate. Increase lamotrigine as needed based on response and tolerability to maintenance dose range for no interacting medications (manufacturer's labeling suggests 250 to 300 mg/day).
For discontinuation of inducers of lamotrigine metabolism (eg, carbamazepine, phenytoin, others): Note: Estrogen derivatives (including hormonal contraceptives) induce lamotrigine metabolism, but separate recommendations apply. See manufacturer's labeling for dosing recommendations with estrogen derivatives.
Immediate or extended release:
- Step 1: Maintain lamotrigine dose unchanged while withdrawing the concomitant enzyme-inducing drug in 5 equal steps (20% decrease per step) over a 4-week period.
- Step 2: The lamotrigine dose should then be decreased beginning 2 weeks after completion of withdrawal of the enzyme-inducing drug; decrease lamotrigine dose no faster than 100 mg/day each week to the maintenance dose range for no interacting medications (manufacturer's labeling suggests 250 to 300 mg/day for extended release).
For discontinuation of antiepileptic drugs that do not affect lamotrigine metabolism:
Immediate release: There are no specific dosing guidelines in the manufacturer's labeling.
Extended release:
- Step 1: Gradually increase lamotrigine dose based on response and tolerability following standard escalation schedule without interacting drugs to the maintenance dose range for no interacting concomitant medications (manufacturer's labeling suggests 250 to 300 mg/day).
- Step 2: Concomitant antiseizure drug should then be withdrawn in 5 equal steps (20% decrease per step) over a 4-week period. Once concomitant antiseizure drug has been discontinued, no adjustment to the lamotrigine dose is needed, unless clinically warranted.
Short-lasting unilateral neuralgiform headache attacks, prophylaxis (off-label use): Oral: Initial: Weeks 1 and 2: 25 mg/day; Weeks 3 and 4: 50 mg/day; beginning with week 5, may increase based on response and tolerability in increments of 50 mg/day every 1 to 2 weeks. Usual maintenance dose: 200 mg/day; doses up to 400 mg/day may be needed for optimal response in some patients (Cohen 2007; Matharu 2019).
Adjustments for interacting medications: Dosing of lamotrigine with concomitant valproate (inhibits lamotrigine metabolism) or inducers (eg, carbamazepine, others) has not been well studied for conditions other than bipolar disorder and seizures; may consider gradual adjustment schedules described for bipolar disorder or seizure indications to avoid increased risk of serious cutaneous hypersensitivity reactions.
Discontinuation of lamotrigine therapy: In chronic therapy, withdraw gradually to minimize the potential of increased seizure frequency (in patients with epilepsy) and withdrawal symptoms (eg, dysphoria, hallucinations, headache, insomnia, tremor) unless safety concerns require more rapid withdrawal. In clinical trials of bipolar disorder, doses were withdrawn by decreasing in weekly intervals by 50% over at least 2 weeks. If discontinuing all pharmacotherapy for bipolar disorder, patients are monitored for several weeks to months for re-emergence of mania/hypomania (Post 2019). For seizure disorders, some experts suggest withdrawing lamotrigine over a few to several (eg, 2 to 6) months (Schachter 2019).
Restarting therapy after treatment interruption or discontinuation: If lamotrigine has been withheld for ≥5 half-lives (ie, >6 days in most patients), restart according to initial dose and dose escalation schedule. If lamotrigine has been withheld for <5 half-lives (ie, ≤6 days), consider restarting at a low dose and increasing to the previous dose gradually. When restarting therapy after treatment interruption, consider the previous daily dose and any concomitant medications that are known to prolong (eg, valproate) or decrease (eg, carbamazepine) half-life of lamotrigine. If treatment was discontinued due to rash, do not resume lamotrigine.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Tablets should not be split to achieve dose; whole tablets should be used for dosing; round calculated dose down to the nearest whole tablet. Alternatively, a suspension may be prepared using immediate release tablets (see Extemporaneous Preparations). Dosage depends on patient's concomitant medications [ie, valproic acid; enzyme-inducing AEDs (specifically phenytoin, phenobarbital, carbamazepine, and primidone); or other AEDs not previously mentioned. Patients receiving concomitant rifampin or other drugs that induce lamotrigine glucuronidation and increase clearance should follow the same dosing regimen as that used with anticonvulsants that have similar effects (eg, phenytoin, phenobarbital, carbamazepine, and primidone).
Anticonvulsant: Lennox-Gastaut syndrome, primary generalized tonic-clonic seizures, or partial seizures; adjunctive (add-on) therapy: Oral:
Immediate-release formulations:
Infants and Children <24 months: Adjunctive therapy; partial seizures: Limited data available (Piña-Garza 2008; Piña-Garza 2008a): Note: As reported in the trials, initial doses were administered every other day if necessary due to limited strengths of commercially available products; use of an extemporaneously compounded suspension may allow for more frequent dosing; usually, daily doses are divided into 1 to 2 doses per day; daily doses in these trials were divided 3 times daily once sufficiently large enough to utilize commercially available products; this was done due to the possible increased clearance of lamotrigine in this age group.
Patients receiving AED regimens containing valproic acid or nonenzyme-inducing AEDs: Note: Studies excluded patients <6.7 kg:
Weeks 1 and 2: 0.15 mg/kg/day
Weeks 3 and 4: 0.3 mg/kg/day
Maintenance dose: Titrate dose to effect; after week 4, increase dose every week by no more than 0.3 mg/kg/day; maximum maintenance dose: 5.1 mg/kg/day in 3 divided doses not to exceed 200 mg/day; mean final dose required in open-label phase of trial was 3.1 mg/kg/day; n=51 (Piña-Garza 2008a)
Patients receiving enzyme-inducing AED regimens (eg, carbamazepine, phenytoin, phenobarbital, or primidone) without valproic acid:
Weeks 1 and 2: 0.6 mg/kg/day
Weeks 3 and 4: 1.2 mg/kg/day
Maintenance dose: Titrate dose to effect; after week 4, increase dose every week by no more than 1.2 mg/kg/day; maximum maintenance dose: 15.6 mg/kg/day in 3 divided doses not to exceed 400 mg/day; mean final dose required in open-label phase of trial was 8.9 mg/kg/day; n=126 (Piña-Garza 2008a)
Children 2 to 12 years: Note: Only whole tablets should be used for dosing; children 2 to 6 years will likely require maintenance doses at the higher end of recommended range; patients weighing <30 kg may need as much as a 50% increase in maintenance dose compared with patients weighing >30 kg; titrate dose to clinical effect
Patients receiving AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproic acid:
Weeks 1 and 2: 0.3 mg/kg/day in 1 to 2 divided doses; round dose down to the nearest whole tablet
Weeks 3 and 4: 0.6 mg/kg/day in 2 divided doses; round dose down to the nearest whole tablet
Maintenance dose: Titrate dose to effect; after week 4, increase dose every 1 to 2 weeks by a calculated increment; calculate increment as 0.6 mg/kg/day rounded down to the nearest whole tablet; add this amount to the previously administered daily dose; usual maintenance: 4.5 to 7.5 mg/kg/day in 2 divided doses; maximum daily dose: 300 mg/day
Patients receiving AED regimens containing valproic acid:
Weeks 1 and 2: 0.15 mg/kg/day in 1 to 2 divided doses; round dose down to the nearest whole tablet; use 2 mg every other day for patients weighing >6.7 kg and <14 kg
Weeks 3 and 4: 0.3 mg/kg/day in 1 to 2 divided doses; round dose down to the nearest whole tablet
Maintenance dose: Titrate dose to effect; after week 4, increase dose every 1 to 2 weeks by a calculated increment; calculate increment as 0.3 mg/kg/day rounded down to the nearest whole tablet; add this amount to the previously administered daily dose; usual maintenance: 1 to 5 mg/kg/day in 1 to 2 divided doses; maximum daily dose: 200 mg/day. Note: Usual maintenance dose in children adding lamotrigine to valproic acid alone: 1 to 3 mg/kg/day
Patients receiving enzyme-inducing AED regimens (eg, carbamazepine, phenytoin, phenobarbital, or primidone) without valproic acid:
Weeks 1 and 2: 0.6 mg/kg/day in 2 divided doses; round dose down to the nearest whole tablet
Weeks 3 and 4: 1.2 mg/kg/day in 2 divided doses; round dose down to the nearest whole tablet
Maintenance dose: Titrate dose to effect; after week 4, increase dose every 1 to 2 weeks by a calculated increment; calculate increment as 1.2 mg/kg/day rounded down to the nearest whole tablet; add this amount to the previously administered daily dose; usual maintenance: 5 to 15 mg/kg/day in 2 divided doses; maximum daily dose: 400 mg/day
Adolescents:
Patients receiving AEDs other than carbamazepine, phenytoin, phenobarbital, primidone, or valproic acid:
Weeks 1 and 2: 25 mg every day
Weeks 3 and 4: 50 mg every day
Maintenance dose: Titrate dose to effect; after week 4, increase dose every 1 to 2 weeks by 50 mg/day; usual maintenance: 225 to 375 mg/day in 2 divided doses
Patients receiving AED regimens containing valproic acid:
Weeks 1 and 2: 25 mg every other day
Weeks 3 and 4: 25 mg every day
Maintenance dose: Titrate dose to effect; after week 4, increase dose every 1 to 2 weeks by 25 to 50 mg/day; usual maintenance in patients receiving valproic acid and other drugs that induce glucuronidation: 100 to 400 mg/day in 1 to 2 divided doses; usual maintenance in patients adding lamotrigine to valproic acid alone: 100 to 200 mg/day
Patients receiving enzyme-inducing AED regimens (eg, carbamazepine, phenytoin, phenobarbital, or primidone) without valproic acid:
Weeks 1 and 2: 50 mg/day
Weeks 3 and 4: 100 mg/day in 2 divided doses
Maintenance dose: Titrate dose to effect; after week 4, increase dose every 1 to 2 weeks by 100 mg/day; usual maintenance: 300 to 500 mg/day in 2 divided doses; doses as high as 700 mg/day in 2 divided doses have been used
Extended-release formulation: Adolescents: Note: Dose increases after week 8 should not exceed 100 mg/day at weekly intervals
Regimens not containing carbamazepine, phenytoin, phenobarbital, primidone, or valproic acid: Initial: Weeks 1 and 2: 25 mg once daily; Weeks 3 and 4: 50 mg once daily; Week 5: 100 mg once daily; Week 6: 150 mg once daily; Week 7: 200 mg once daily; Maintenance: 300 to 400 mg once daily
Regimens containing valproic acid: Initial: Weeks 1 and 2: 25 mg every other day; Weeks 3 and 4: 25 mg once daily; Week 5: 50 mg once daily; Week 6: 100 mg once daily; Week 7: 150 mg once daily; Maintenance: 200 to 250 mg once daily
Regimens containing carbamazepine, phenytoin, phenobarbital, or primidone and without valproic acid: Initial: Weeks 1 and 2: 50 mg once daily; Weeks 3 and 4: 100 mg once daily; Week 5: 200 mg once daily; Week 6: 300 mg once daily; Week 7: 400 mg once daily; Maintenance: 400 to 600 mg once daily
Conversion from immediate release to extended release (Lamictal XR): Initial dose of the extended release tablet (given once daily) should match the total daily dose of the immediate release formulation; monitor for seizure control, especially in patients on AED agents. Adjust dose as needed within the recommended dosing guidelines.
Anticonvulsant: Partial seizures; monotherapy: Oral:
Immediate-release formulations: Adolescents ≥16 years:
Conversion from adjunctive therapy with a single enzyme-inducing AED (eg, carbamazepine, phenytoin, phenobarbital, or primidone and not valproate) to lamotrigine immediate release monotherapy: Note: First add lamotrigine and titrate it (as outlined below) to the recommended maintenance monotherapy dose (500 mg/day in 2 divided doses), while maintaining the enzyme-inducing AED at a fixed level; then gradually taper the enzyme-inducing AED by 20% decrements each week to fully withdraw over a 4-week period.
Weeks 1 and 2: 50 mg/day
Weeks 3 and 4: 100 mg/day in 2 divided doses
Maintenance dose: After week 4, increase dose every 1 to 2 weeks by 100 mg/day; recommended maintenance monotherapy dose: 500 mg/day in 2 divided doses
Conversion from adjunctive therapy with valproate to lamotrigine immediate release monotherapy: Note: This is a 4-step conversion process to achieve the lamotrigine recommended monotherapy dose (500 mg/day in 2 divided doses).
First: Add lamotrigine and titrate it to a dose of 200 mg/day as follows (if not already receiving 200 mg/day), while maintaining the valproate dose at a fixed level:
Weeks 1 and 2: 25 mg every other day
Weeks 3 and 4: 25 mg every day
Then increase dose every 1 to 2 weeks by 25 to 50 mg/day
Second: Keep lamotrigine dose at 200 mg/day; slowly taper valproate dose in decrements of ≤500 mg/day per week, to a dose of 500 mg/day; maintain this dose for one week
Third: Increase lamotrigine to 300 mg/day and decrease valproate to 250 mg/day; maintain this dose for one week
Fourth: Discontinue valproate and increase lamotrigine by 100 mg/day at weekly intervals to achieve recommended maintenance monotherapy dose of 500 mg/day in 2 divided doses
Conversion from adjunctive therapy with AEDs other than enzyme-inducing AEDs or valproate to lamotrigine immediate release monotherapy: No specific guidelines available
Extended-release formulation: Adolescents:
Conversion from adjunctive therapy with AEDs other than enzyme-inducing AEDs or valproate to lamotrigine extended release monotherapy: First add lamotrigine and titrate it (as outlined below) to a recommended lamotrigine dose of 250 to 300 mg once daily, while maintaining the concomitant AED at a fixed level; then gradually taper the concomitant AED by 20% decrements each week to fully withdraw over a 4-week period.
Weeks 1 and 2: 25 mg once daily
Weeks 3 and 4: 50 mg once daily
Week 5: 100 mg once daily
Week 6: 150 mg once daily
Week 7: 200 mg once daily
Maintenance: 250 to 300 mg once daily
Conversion from adjunctive therapy with valproate to lamotrigine extended release monotherapy: Note: This is a 4-step conversion process to achieve the lamotrigine recommended extended release monotherapy dose (250 to 300 mg once daily).
First: Add lamotrigine and titrate it to a dose of 150 mg/day as follows (if not already receiving 150 mg/day), while maintaining the valproate dose at a fixed level:
Weeks 1 and 2: 25 mg every other day
Weeks 3 and 4: 25 mg once daily
Week 5: 50 mg once daily
Week 6: 100 mg once daily
Week 7: 150 mg once daily
Second: Keep lamotrigine dose at 150 mg/day; slowly taper valproate dose in decrements of ≤500 mg/day per week, to a dose of 500 mg/day; maintain this dose for 1 week
Third: Increase lamotrigine to 200 mg/day and decrease valproate to 250 mg/day; maintain this dose for 1 week
Fourth: Discontinue valproate and increase lamotrigine to a maintenance dose of 250 to 300 mg/day
Conversion from adjunctive therapy with a single enzyme-inducing AED (eg, carbamazepine, phenytoin, phenobarbital, or primidone and not valproate) to lamotrigine extended release monotherapy in patients with partial seizures: Note: First add lamotrigine and titrate it (as outlined below) to a recommended lamotrigine dose of 500 mg/day, while maintaining the enzyme-inducing AED at a fixed level; then gradually taper the enzyme-inducing AED by 20% decrements each week to fully withdraw over a 4-week period. Two weeks following withdrawal of the enzyme-inducing AED, the dosage of lamotrigine extended release may be tapered in decrements of ≤100 mg/day at intervals of 1 week to achieve a maintenance dosage range of 250 to 300 mg/day
Weeks 1 and 2: 50 mg once daily
Weeks 3 and 4: 100 mg once daily
Maintenance: After week 4, increase dose every 1 week by 100 mg/day to a lamotrigine dose of 500 mg once daily
Anticonvulsant: Absence seizures; monotherapy: Oral: Limited data available; efficacy results variable, optimal dose and titration not defined:
Immediate-release formulations: Children and Adolescents 2.5 to 13 years: Initial: 0.3 mg/kg/day in 2 divided doses for 2 weeks; then 0.6 mg/kg/day for 2 weeks; titrate weekly to effect/tolerability to a maximum daily dose of 12 mg/kg/day or 600 mg/day (whichever is less) (Glauser 2010; Glauser 2013). Multiple titration strategies have been reported. In the largest trial (n=453), the efficacy of lamotrigine (n=149) was compared with valproic acid (n=148) and ethosuximide (n=156); the initial lamotrigine dose was 0.3 mg/kg/day for 2 weeks, followed by 0.6 mg/kg/day for 2 weeks, then the dose was increased at weekly intervals until efficacy or intolerability in 0.6 mg/kg/day increments up to 3 mg/kg/day for 1 week (week 8), then increased to 4.5 mg/kg/day for 2 weeks, then 7 mg/kg/day for 2 weeks, then 9 mg/kg/day for 2 weeks, and then finally 12 mg/kg/day (week 15); mean final dose reported was 9.7 ± 6.3 mg/kg/day. Results showed the lamotrigine treatment arm had a treatment failure rate of 71%, compared to 47% failure with ethosuximide and 42% failure with valproic acid; the superior efficacy of valproic acid and ethosuximide persisted at 12 months (Glauser 2010; Glauser 2013). Another titration strategy based on two smaller studies used a higher initial dose of 0.5 mg/kg/day in 2 divided doses for 2 weeks, increased to 1 mg/kg/day for 2 weeks, then increased by 1 mg/kg/day increments every 5 days (or as clinically indicated) to a maximum of 12 mg/kg/day (Coppola 2004; Frank 1999). In one dose-escalation trial of 45 patients (2 to 15 years old), the median effective dose required was 5 mg/kg/day (range: 2 to 15 mg/kg/day) (Frank 1999). The other study was an open-label trial comparing lamotrigine (n=19) to valproic acid (n=19) in 3 to 13 year olds; the mean lamotrigine dose required at 3 months was 6.5 mg/kg/day (range: 2 to 11.5 mg/kg/day) (Coppola 2004).
Bipolar disorder: Oral: Immediate-release formulation: Adolescents ≥18 years:
Patients not receiving enzyme-inducing drugs (eg, carbamazepine, phenytoin, phenobarbital, primidone, rifampin) or valproate:
Weeks 1 and 2: 25 mg/day
Weeks 3 and 4: 50 mg/day
Week 5: 100 mg/day
Week 6 and thereafter: 200 mg/day
Patients receiving valproate:
Weeks 1 and 2: 25 mg every other day
Weeks 3 and 4: 25 mg/day
Week 5: 50 mg/day
Week 6 and thereafter: 100 mg/day
Note: If valproate is discontinued, increase daily lamotrigine dose in 50 mg increments at weekly intervals until dosage of 200 mg/day is attained.
Patients receiving enzyme-inducing drugs (eg, carbamazepine, phenytoin, phenobarbital, primidone, rifampin) without valproate:
Weeks 1 and 2: 50 mg/day
Weeks 3 and 4: 100 mg/day in divided doses
Week 5: 200 mg/day in divided doses
Week 6: 300 mg/day in divided doses
Week 7 and thereafter: May increase to 400 mg/day in divided doses
Note: If carbamazepine (or other enzyme-inducing drug) is discontinued, maintain current lamotrigine dose for 1 week, then decrease daily lamotrigine dose in 100 mg increments at weekly intervals until dosage of 200 mg/day is attained.
Dosing adjustment with concomitant atazanavir/ritonavir: Adolescents: Follow initial lamotrigine dosing guidelines, maintenance dose should be adjusted as follows:
Patients not taking concomitant carbamazepine, phenytoin, phenobarbital, primidone, rifampin, estrogen-containing contraceptives, or lopinavir/ritonavir: Lamotrigine maintenance dose may need to be increased if atazanavir/ritonavir is added or decreased if atazanavir/ritonavir is discontinued.
Dosing adjustment with concomitant estrogen-containing oral contraceptives: Adolescents: Follow initial lamotrigine dosing guidelines, maintenance dose should be adjusted as follows:
Patients taking concomitant carbamazepine, phenytoin, phenobarbital, primidone, or other drugs, such as rifampin, that induce lamotrigine glucuronidation: No dosing adjustment required
Patients not taking concomitant carbamazepine, phenytoin, phenobarbital, primidone, or other drugs, such as rifampin, that induce lamotrigine glucuronidation: If already taking estrogen-containing oral contraceptives, the maintenance dose of lamotrigine may need to be increased by as much as twofold over the target maintenance dose listed above. If already taking a stable dose of lamotrigine and starting an oral contraceptive agent, the lamotrigine maintenance dose may need to be increased by as much as twofold. Dose increases should start when contraceptive agent is started and titrated to clinical response increasing no more rapidly than 50 to 100 mg/day every week. Gradual increases of lamotrigine plasma levels may occur during the inactive “pill-free” week and will be greater when dose increases are made the week before. If increased adverse events consistently occur during “pill-free” week, overall dose adjustments may be required. Dose adjustments during “pill-free” week are not recommended. When discontinuing combination hormonal contraceptive, dose of lamotrigine may need decreased by as much as 50%; do not decrease by more than 25% of total daily dose over a 2-week period unless clinical response or plasma levels indicate otherwise.
Additional considerations:
Discontinuing therapy: Children ≥2 years and Adolescents: Do not abruptly discontinue; when discontinuing lamotrigine therapy, gradually decrease the dose by ~50% per week and taper over at least 2 weeks unless safety concerns require a more rapid withdrawal. Note: If discontinuing other anticonvulsants and maintaining lamotrigine therapy, keep in mind that discontinuing carbamazepine, phenytoin, phenobarbital, primidone, or other drugs, such as rifampin, that induce lamotrigine glucuronidation should prolong the half-life of lamotrigine; discontinuing valproic acid should shorten the half-life of lamotrigine; monitor patient closely; dosage change may be needed.
Restarting therapy after discontinuation: Children ≥2 years and Adolescents: If lamotrigine has been withheld for >5 half-lives, restart according to initial dosing recommendations. If lamotrigine has been withheld for <5 half-lives, consider restarting at a low dose and increasing to the previous dose gradually, based on the duration of treatment interruption, half-life of lamotrigine, and previous daily dose. Note: Concomitant medications may affect the half-life of lamotrigine; consider pharmacokinetic interactions when restarting therapy.
Extemporaneously Prepared
A 1 mg/mL oral suspension may be made with tablets and one of two different vehicles (a 1:1 mixture of Ora-Sweet and Ora-Plus or a 1:1 mixture of Ora-Sweet SF and Ora-Plus). Crush one 100 mg tablet in a mortar and reduce to a fine powder. Add small portions of the chosen vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 100 mL; transfer to a graduated cylinder, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 100 mL. Label "shake well" and "protect from light". Stable for 91 days when stored in amber plastic prescription bottles in the dark at room temperature or refrigerated.
Nahata M, Morosco R, Hipple T. “Stability of Lamotrigine in Two Extemporaneously Prepared Oral Suspensions at 4 and 25 Degrees C,” Am J Health Syst Pharm, 1999, 56(3):240-2.10030509
Administration
Oral: Doses should be rounded down to the nearest whole tablet.
Lamictal chewable/dispersible tablets: May be chewed, dispersed in water or diluted fruit juice, or swallowed whole. To disperse tablets, add to a small amount of liquid (just enough to cover tablet); let sit ~1 minute until dispersed; swirl solution and consume immediately. Do not administer partial amounts of liquid. If tablets are chewed, a small amount of water or diluted fruit juice should be used to aid in swallowing.
Lamictal ODT: Place tablets on tongue and move around in the mouth. Tablets will dissolve rapidly and can be swallowed with or without food or water.
Lamictal XR: Administer without regard to meals. Swallow whole; do not chew, crush, or cut.
Storage
Store at 15°C to 30°C (59°F to 86°F). Protect from light.
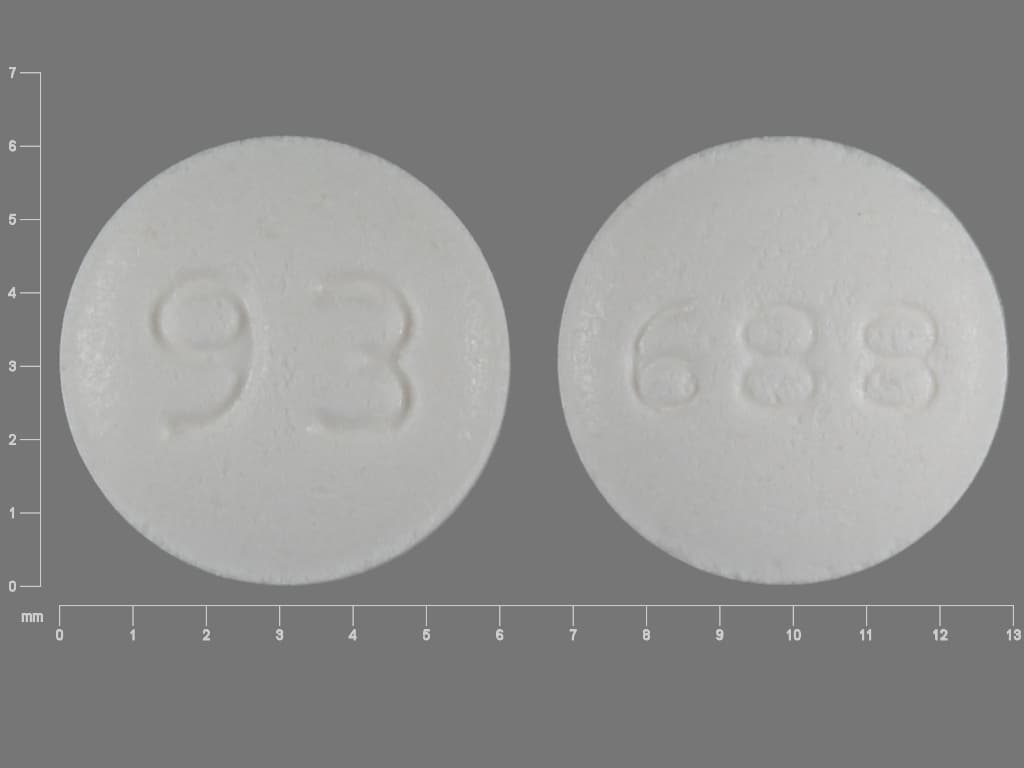
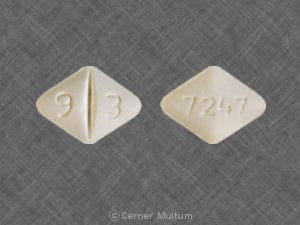
LamoTRIgine Images
Drug Interactions
Acetaminophen: May decrease the serum concentration of LamoTRIgine. Monitor therapy
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Atazanavir: May decrease the serum concentration of LamoTRIgine. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Barbiturates: May decrease the serum concentration of LamoTRIgine. Management: See lamotrigine prescribing information for specific age-dependent dosing guidelines regarding concurrent use with a barbiturate, as well as for adjusting lamotrigine dosing if concurrent barbiturate therapy is discontinued. Consider therapy modification
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
CarBAMazepine: LamoTRIgine may enhance the adverse/toxic effect of CarBAMazepine. CarBAMazepine may increase the metabolism of LamoTRIgine. Consider therapy modification
Cenobamate: May decrease the serum concentration of LamoTRIgine. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Desmopressin: LamoTRIgine may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Dofetilide: LamoTRIgine may increase the serum concentration of Dofetilide. Avoid combination
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Estrogen Derivatives: May decrease the serum concentration of LamoTRIgine. Monitor therapy
Estrogen Derivatives (Contraceptive): May decrease the serum concentration of LamoTRIgine. Management: Most patients taking estrogen-containing contraceptives will require lamotrigine dose increases up to 2-fold over the recommended target lamotrigine dose. Increase lamotrigine doses by 50 to 100 mg/day every week based on clinical response. Consider therapy modification
Ezogabine: May decrease the serum concentration of LamoTRIgine. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosphenytoin: May decrease the serum concentration of LamoTRIgine. Consider therapy modification
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lacosamide: Antiepileptic Agents (Sodium Channel Blockers) may enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
MetFORMIN: LamoTRIgine may increase the serum concentration of MetFORMIN. Management: The lamotrigine Canadian product monograph states that coadministration of these drugs is not recommended. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May diminish the therapeutic effect of Anticonvulsants. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
OLANZapine: LamoTRIgine may enhance the sedative effect of OLANZapine. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Phenytoin: May decrease the serum concentration of LamoTRIgine. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Primidone: May decrease the serum concentration of LamoTRIgine. Management: Adjust dose per lamotrigine prescribing information guidelines during primidone treatment. Monitor for decreased concentration/effect if primidone is initiated/dose increased or increased concentration/effect if primidone is discontinued/dose decreased. Consider therapy modification
Procainamide: LamoTRIgine may increase the serum concentration of Procainamide. Management: Consider monitoring for increased procainamide concentrations and/or systemic effects in patients receiving procainamide with lamotrigine. The lamotrigine Canadian product monograph states that coadministration of these agents is not recommended. Monitor therapy
Progestins (Contraceptive): LamoTRIgine may decrease the serum concentration of Progestins (Contraceptive). Monitor therapy
RifAMPin: May increase the metabolism of LamoTRIgine. Monitor therapy
Ritonavir: May decrease the serum concentration of LamoTRIgine. Consider therapy modification
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Sulthiame: May increase the serum concentration of LamoTRIgine. Monitor therapy
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Valproate Products: May enhance the adverse/toxic effect of LamoTRIgine. Valproate Products may increase the serum concentration of LamoTRIgine. Management: Lamotrigine labeling recommends an approximate 50% decrease in lamotrigine dose when used with valproic acid or other valproate products. See full monograph or lamotrigine labeling for more specific recommendations. Monitor lamotrigine response closely. Consider therapy modification
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
May interfere with some rapid urine drug screens, particularly phencyclidine (false-positives).
Adverse Reactions
Percentages reported in adults on monotherapy for epilepsy or bipolar disorder.
>10%: Gastrointestinal: Nausea (7% to 14%)
1% to 10%:
Cardiovascular: Chest pain (2% to 5%), peripheral edema (2% to 5%), edema (1% to 5%)
Central nervous system: Insomnia (5% to 10%), drowsiness (9%), fatigue (8%), dizziness (7%), ataxia (2% to 7%), anxiety (5%), pain (5%), irritability (2% to 5%), suicidal ideation (2% to 5%), abnormal dreams (1% to 5%), abnormality in thinking (1% to 5%), agitation (1% to 5%), amnesia (1% to 5%), depression (1% to 5%), emotional lability (1% to 5%), hypoesthesia (1% to 5%), migraine (1% to 5%), neurologic abnormality (dyspraxia) (1% to 5%), hyperreflexia (>2% to <5%), hyporeflexia (>2% to <5%), confusion (≥1%), paresthesia (≥1%)
Dermatologic: Skin rash (nonserious: 7%; requiring hospitalization: ≤1%), contact dermatitis (2% to 5%), diaphoresis (2% to 5%), xeroderma (2% to 5%)
Endocrine & metabolic: Increased libido (2% to 5%), weight loss (2% to 5%), weight gain (1% to 5%)
Gastrointestinal: Vomiting (5% to 9%), dyspepsia (7%), abdominal pain (6%), xerostomia (2% to 6%), constipation (5%), anorexia (2% to 5%), peptic ulcer (2% to 5%), flatulence (1% to 5%)
Genitourinary: Dysmenorrhea (2% to 5%), urinary frequency (1% to 5%)
Hematologic & oncologic: Rectal hemorrhage (2% to 5%)
Infection: Infection (5%)
Neuromuscular & skeletal: Back pain (8%), asthenia (2% to 5%), arthralgia (1% to 5%), myalgia (1% to 5%), neck pain (1% to 5%)
Ophthalmic: Nystagmus disorder (2% to 5%), visual disturbance (2% to 5%), amblyopia (≥1%)
Respiratory: Rhinitis (7%), cough (5%), pharyngitis (5%), bronchitis (2% to 5%), dyspnea (2% to 5%), epistaxis (2% to 5%), sinusitis (1% to 5%), nasopharyngitis (≥3%), upper respiratory tract infection (≥3%)
Miscellaneous: Fever (1% to 5%)
Frequency not defined:
Dermatologic: Severe dermatological reaction
Hematologic & oncologic: Natural killer cell count increased (hemophagocytic lymphohistiocytosis)
<1%, postmarketing and/or case reports (any indication): Abnormal hepatic function tests, abnormal lacrimation, accommodation disturbance, acne vulgaris, acute renal failure, ageusia, aggressive behavior, agranulocytosis, akathisia, alcohol intolerance, alopecia, altered sense of smell, amyotrophy, anemia, angioedema, anorgasmia, apathy, aphasia, aplastic anemia, apnea, arthritis, aseptic meningitis, blepharoptosis, breast abscess, breast neoplasm, bursitis, central nervous system depression, chills, choreoathetosis, conjunctivitis, cystitis, deafness, decreased fibrin, decreased libido, decreased serum fibrinogen, delirium, delusion, depersonalization, dermatitis (exfoliative, fungal), drug reaction with eosinophilia and systemic symptoms syndrome, dry eye syndrome, dysarthria, dysgeusia, dyskinesia, dysphagia, dysphoria, dystonia, dysuria, ecchymosis, ejaculatory disorder, eosinophilia, epididymitis, eructation, erythema multiforme, erythema of skin, esophagitis, euphoria, exacerbation of Parkinson disease, extrapyramidal reaction, flushing, gastric ulcer, gastritis, gastrointestinal hemorrhage, gingival hemorrhage, gingival hyperplasia, gingivitis, glossitis, goiter, hallucination, heavy menstrual bleeding, hematemesis, hematuria, hemiplegia, hemolytic anemia, hemorrhagic colitis, hepatitis, hepatotoxicity (idiosyncratic) (Chalasani 2014), herpes zoster infection, hiccups, hirsutism, hostility, hot flash, hyperalgesia, hyperbilirubinemia, hyperesthesia, hyperglycemia, hyperkinetic muscle activity, hypersensitivity reaction, hypertension, hypertonia, hyperventilation, hypogammaglobulinemia, hypokinesia, hypothyroidism, hypotonia, immunosuppression (progressive), impotence, increased appetite, increased gamma-glutamyl transferase, increased serum alkaline phosphatase, increased serum alanine aminotransferase, increased serum aspartate aminotransferase, increased serum creatinine, iron deficiency anemia, lactation, leukocytosis, leukoderma, leukopenia, lower limb cramp, lupus-like syndrome, lymphadenopathy, lymphocytosis, macrocytic anemia, maculopapular rash, malaise, manic depressive reaction, melena, memory impairment, movement disorder, multiorgan failure, muscle spasm, myasthenia, myoclonus, neuralgia, neutropenia, nocturia, oral mucosa ulcer, orthostatic hypotension, oscillopsia, otalgia, palpitations, pancreatitis, pancytopenia, panic attack, paralysis, paranoid ideation, pathological fracture, peripheral neuritis, personality disorder, petechia, petechial rash, photophobia, polyuria, pruritus, psychoneurosis, psychosis, pure red cell aplasia, pustular rash, racing mind, renal pain, rhabdomyolysis, sialorrhea, skin discoloration, sleep disorder, status epilepticus, Stevens-Johnson syndrome, stomatitis, strabismus, stupor, suicidal tendencies, syncope, tachycardia, tendinous contracture, thrombocytopenia, tic disorder, tinnitus, tongue edema, tonic clonic epilepsy (exacerbation), toxic epidermal necrolysis, twitching, urinary incontinence, urinary retention, urinary urgency, urticaria, uveitis, vasculitis, vasodilation, vesiculobullous dermatitis, visual field defect, withdrawal syndrome (seizures with abrupt withdrawal), yawning
Warnings/Precautions
Concerns related to adverse effects:
- Aseptic meningitis: Increased risk of developing aseptic meningitis has been reported; symptoms (eg, headache, nuchal rigidity, fever, nausea/vomiting, rash, photophobia) have generally occurred within 1 to 45 days following therapy initiation. In some cases, new onset hepatic, renal and/or other organ involvement has also occurred with symptoms, possibly suggesting aseptic meningitis is associated with a hypersensitivity reaction (eg, anticonvulsant hypersensitivity syndrome). Symptoms of aseptic meningitis generally resolve following discontinuation. In some cases, re-exposure has resulted in a rapid return of symptoms (often more severe).
- Blood dyscrasias: A spectrum of hematologic effects have been reported with use (eg, neutropenia, leukopenia, thrombocytopenia, pancytopenia, anemias, and rarely, aplastic anemia and pure red cell aplasia); patients with a previous history of adverse hematologic reaction to any drug may be at increased risk. Early detection of hematologic change is important; advise patients of early signs and symptoms including fever, sore throat, mouth ulcers, infections, easy bruising, petechial or purpuric hemorrhage. May be associated with hypersensitivity syndrome.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Hemophagocytic lymphohistiocytosis: Hemophagocytic lymphohistiocytosis (HLH), a rare but life-threatening immune system reaction, has been reported with lamotrigine use. Symptoms may include fever, rash, hepatosplenomegaly, organ system dysfunction, and blood dyscrasias. Onset usually occurs within the first several weeks after starting therapy. Patients with HLH symptoms should be evaluated promptly; discontinuation and conversion to alternate therapy may be required.
- Multiorgan hypersensitivity reactions (drug reaction with eosinophilia and systemic symptoms [DRESS]): Potentially serious, sometimes fatal, multiorgan hypersensitivity reactions (DRESS) have been reported with some antiepileptic drugs (rare). Symptoms may include fever, rash, and/or lymphadenopathy; monitor for signs and symptoms of possible disparate manifestations associated with lymphatic, hepatic, renal, and/or hematologic organ systems. Early symptoms of hypersensitivity reaction (eg, lymphadenopathy, fever) may occur without rash; discontinuation and conversion to alternate therapy may be required.
- Skin reactions: [US Boxed Warning]: Serious skin rashes requiring hospitalization and discontinuation of treatment have been reported; incidence of serious rash is higher in pediatric patients than adults; risk may be increased by coadministration with valproic acid, higher than recommended initial doses, exceeding recommended initial dose titration, or exceeding the recommended dose escalation for lamotrigine. One rash-related death was reported in a pediatric patient taking lamotrigine immediate-release as adjunctive therapy. Nearly all cases of life-threatening rashes caused by lamotrigine have occurred within 2 to 8 weeks of treatment initiation; however, isolated cases may occur after prolonged treatment (eg, 6 months) or in patients without these risk factors; discontinue at first sign of rash and do not reinitiate therapy unless rash is clearly not drug related. Rare cases of toxic epidermal necrolysis and/or rash-related death have been reported. Discontinuation of treatment may not prevent a rash from becoming life-threatening or permanently disabling or disfiguring.
- Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; notify healthcare provider immediately if symptoms occur.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with hepatic impairment; dosage adjustment may be required.
- Renal impairment: Use with caution in patients with renal impairment; dosage adjustment may be required.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Pediatric: Children are at increased risk for developing serious skin rashes during therapy; lower starting doses and slower dose escalations may decrease the risk of rash.
Dosage form specific issues:
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Other warnings/precautions:
- Appropriate use: Bipolar disorder use: Patients treated for bipolar disorder should be monitored closely for clinical worsening or suicidality; reassess patients to determine the need for maintenance treatment if on therapy >16 weeks. Prescriptions should be written for the smallest quantity consistent with good patient care. Treatment of acute manic or mixed episodes is not recommended; efficacy has not been established and slow titration limits use.
- Medication error potential: Medication errors have occurred; potential for medication errors with similar-sounding medications and between different lamotrigine formulations.
- Melanin binding: Binds to melanin and may accumulate in the eye and other melanin-rich tissues; the clinical significance of this is not known.
- Monotherapy: Epilepsy: Safety and efficacy have not been established for use as initial monotherapy, conversion to monotherapy from antiepileptic drugs (AED) other than carbamazepine, phenytoin, phenobarbital, primidone or valproic acid or conversion to monotherapy from two or more AEDs.
- Withdrawal: Anticonvulsants should not be discontinued abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal. Taper over at least 2 weeks if possible.
Monitoring Parameters
Serum levels of concurrent anticonvulsants, LFTs, renal function, hypersensitivity reactions (especially rash); seizure, frequency and duration; suicidality (eg, suicidal thoughts, depression, behavioral changes); signs/symptoms of aseptic meningitis
Pregnancy
Pregnancy Considerations
Lamotrigine crosses the human placenta and can be measured in the plasma of exposed newborns (Harden and Pennell 2009; Ohman 2000). An overall increase in the risk for major congenital malformations has not been observed in available studies; however, an increased risk for cleft lip or cleft palate has not been ruled out (Cunnington 2011; Hernández-Díaz 2012; Holmes 2012). An increased risk of malformations following maternal lamotrigine use may be associated with larger doses (Cunnington 2007; Tomson 2011). Polytherapy may increase the risk of congenital malformations; monotherapy with the lowest effective dose is recommended (Harden and Meader 2009).
Due to pregnancy-induced physiologic changes, women who are pregnant may require dose adjustments of lamotrigine in order to maintain clinical response; monitoring during pregnancy should be considered (Harden and Pennell 2009). For women with epilepsy who are planning a pregnancy in advance, baseline serum concentrations should be measured once or twice prior to pregnancy during a period when seizure control is optimal. Monitoring can then be continued up to once a month during pregnancy and every second day during the first week postpartum (Patsalos 2008; Patsalos 2018). Potentially significant interactions may exist with hormone-containing contraceptives.
Pregnancy registries are available for women who have been exposed to lamotrigine. Patients may enroll themselves in the North American Antiepileptic Drug (NAAED) Pregnancy Registry by calling (888) 233-2334. Additional information is available at www.aedpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used to help control certain kinds of seizures.
- It is used to treat bipolar problems.
Frequently reported side effects of this drug
- Fatigue
- Nausea
- Abdominal pain
- Lack of appetite
- Vomiting
- Tremors
- Trouble sleeping
- Stuffy nose
- Sore throat
- Constipation
- Weight loss
- Dry mouth
- Back pain
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion.
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Infection
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Swollen glands
- Seizures
- Severe muscle weakness
- Severe muscle pain
- Severe joint pain
- Severe joint swelling
- Bruising
- Bleeding
- Severe loss of strength and energy
- Vision changes
- Severe dizziness
- Passing out
- Change in balance
- Involuntary eye movements
- Chest pain
- Flu-like symptoms
- Menstrual changes
- Painful periods
- Aseptic meningitis like headache, fever, chills, severe nausea or vomiting, stiff neck, rash, sensitivity to lights, fatigue, or confusion.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.