Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Kit, Combination:
Lupaneta Pack: 1-month kit: leuprolide acetate 3.75 mg depot suspension for injection (1) and norethindrone acetate 5 mg oral tablets (30), 3-month kit: leuprolide acetate 11.25 mg depot suspension for injection (1) and norethindrone acetate 5 mg oral tablets (90) [contains polysorbate 80]
Pharmacology
Mechanism of Action
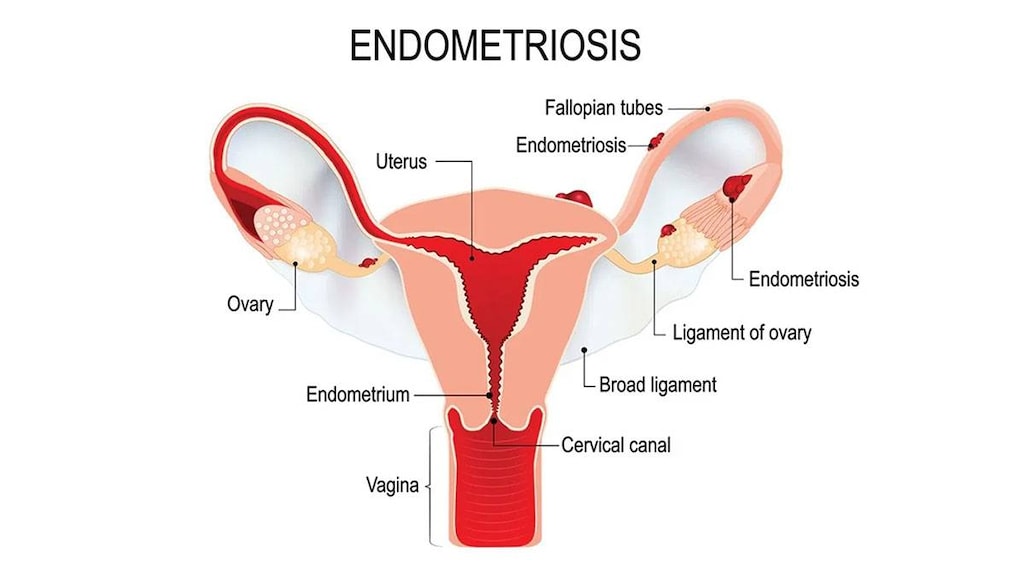
Leuprolide administration inhibits the production of estrogen through negative feedback of pituitary gonadotropins. This in turn decreases endometrial implants and symptoms of endometriosis such as pain. Norethindrone is used to decrease adverse events observed with the hypoestrogenic state caused by leuprolide and possibly mitigate bone mineral density loss (Surrey, 2010).
Use: Labeled Indications
Endometriosis: Management of initial and recurrent painful symptoms of endometriosis
Contraindications
Hypersensitivity to leuprolide, gonadotropin-releasing hormone (GnRH), GnRH-agonist analogs, norethindrone acetate, or any component of the formulation; undiagnosed abnormal uterine bleeding; breast cancer or other hormone-dependent neoplasms (current or a history of); hepatic tumors or disease; thrombotic or thromboembolic disorder (current or history of); pregnancy (or planned pregnancy during therapy); breastfeeding
Dosage and Administration
Dosing: Adult
Endometriosis: Females: Note: Treatment consists of an oral norethindrone tablet used in conjunction with an IM leuprolide injection. The initial therapy should be limited to 6 months duration; a single re-treatment of not more than 6 additional months may be administered if symptoms recur. Maximum total duration of therapy is 12 months.
1 month:
Injection: IM: Leuprolide 3.75 mg as a single dose administered by healthcare provider once every month for up to 6 doses (maximum initial therapy: 6 months; maximum cumulative therapy: 12 months)
Tablet: Oral: Norethindrone 5 mg once daily for up to 6 months (maximum initial therapy: 6 months; maximum cumulative therapy: 12 months)
3 month:
Injection: IM: Leuprolide 11.25 mg as a single dose administered by healthcare provider once every 3 months for up to 2 doses (maximum initial therapy: 6 months; maximum cumulative therapy: 12 months)
Tablet: Oral: Norethindrone 5 mg once daily for up to 6 months (maximum initial therapy: 6 months; maximum cumulative therapy: 12 months)
Dosing: Geriatric
Not for use in postmenopausal women
Reconstitution
Syringe: Prior to use, contents of prefilled syringe must be mixed. Do not use if the powder is clumping or caking, or if the diluent is not clear prior to mixing. Screw components of the syringe together and hold upright. Slowly push plunger to mix contents; while holding upright, shake gently until a uniform suspension forms. Do not use if the powder does not go into suspension.
Administration
IM: Leuprolide: Administer IM in the gluteal area, anterior thigh, or deltoid. Do not use if a blood vessel is accidently penetrated (will be able to see aspirated blood below the transparent luer lock).
Tablet: Norethindrone: Administer orally.
Dietary Considerations
In clinical trials, women were given supplemental elemental calcium 1000 mg/day.
Storage
Syringe: Prior to reconstitution, store at room temperature at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Following reconstitution, administer within 2 hours.
Tablets: Store at room temperature at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
Drug Interactions
Acitretin: May diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Given the potential for progestin-only preparations to fail to prevent pregnancy during acitretin therapy, such products should not be relied upon. Alternative, nonhormonal forms of contraception must be employed during acitretin therapy. Consider therapy modification
Anticoagulants: Progestins may diminish the therapeutic effect of Anticoagulants. More specifically, the potential prothrombotic effects of some progestins and progestin-estrogen combinations may counteract anticoagulant effects. Management: Carefully weigh the prospective benefits of progestins against the potential increased risk of procoagulant effects and thromboembolism. Use is considered contraindicated under some circumstances. Refer to related guidelines for specific recommendations. Consider therapy modification
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Aprepitant: May decrease the serum concentration of Progestins (Contraceptive). Management: Alternative or additional methods of contraception should be used both during treatment with aprepitant or fosaprepitant and for at least one month following the last aprepitant/fosaprepitant dose. Consider therapy modification
Artemether: May decrease the serum concentration of Progestins (Contraceptive). Management: Consider the use of an alternative (i.e., non-hormonal) means of contraception in all women of childbearing potential who are using artemether. Consider therapy modification
Atazanavir: May increase the serum concentration of Progestins (Contraceptive). However, atazanavir may lead to decreased ethinyl estradiol concentrations and decreased effectiveness of oral contraceptive products. Management: Consider an alternative or additional method of contraception, particularly with combined estrogen/progestin products. Depot medroxyprogesterone acetate may be used without a need for additional contraception. Consider therapy modification
Barbiturates: May diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Use of alternative, nonhormonal contraceptives is recommended. Consider therapy modification
Bexarotene (Systemic): May decrease the serum concentration of Progestins (Contraceptive). Management: Women of childbearing potential receiving bexarotene should use two reliable forms of contraception (including at least one nonhormonal form). Consider therapy modification
Bile Acid Sequestrants: May decrease the serum concentration of Progestins (Contraceptive). Management: Administer oral progestin-containing contraceptives at least 1 to 4 hours prior to or 4 to 6 hours after administration of a bile acid sequestrant. Consider therapy modification
Bosentan: May decrease the serum concentration of Progestins (Contraceptive). Management: Use an alternative (i.e., non-hormonal) means of contraception for all women of childbearing potential who are using bosentan, and do not rely on hormonal contraceptives alone. Consider therapy modification
Brigatinib: May decrease the serum concentration of Progestins (Contraceptive). Management: Females of childbearing potential should use an alternative, non-hormonal contraceptive during brigatinib therapy and for at least 4 months after the final brigatinib dose. Consider therapy modification
C1 inhibitors: Progestins may enhance the thrombogenic effect of C1 inhibitors. Monitor therapy
CarBAMazepine: May diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Use of alternative, nonhormonal contraceptives is recommended. Consider therapy modification
Carfilzomib: May enhance the thrombogenic effect of Progestins (Contraceptive). Management: Consider alternative, non-hormonal methods of contraception in patients requiring therapy with carfilzomib. Consider therapy modification
Cenobamate: May decrease the serum concentration of Hormonal Contraceptives. Management: Women should use additional or alternative non-hormonal birth control while taking cenobamate. Consider therapy modification
Choline C 11: Luteinizing Hormone-Releasing Hormone Analogs may diminish the therapeutic effect of Choline C 11. Monitor therapy
Cladribine: May diminish the therapeutic effect of Hormonal Contraceptives. Management: Women using systemically acting hormonal contraceptives should add a barrier method during cladribine dosing and for at least 4 weeks after the last dose in each treatment course. Consider therapy modification
CloBAZam: May decrease the serum concentration of Progestins (Contraceptive). Consider therapy modification
Cobicistat: May increase the serum concentration of Progestins (Contraceptive). Management: Consider an alternative, nonhormone-based contraceptive in patients receiving cobicistat-containing products. Drospirenone is specifically contraindicated with atazanavir and cobicistat. Consider therapy modification
Colesevelam: May decrease the serum concentration of Norethindrone. Management: Oral contraceptives containing ethinyl estradiol and norethindrone should be administered at least 4 hours before colesevelam. Consider therapy modification
Corifollitropin Alfa: Luteinizing Hormone-Releasing Hormone Analogs may enhance the therapeutic effect of Corifollitropin Alfa. Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dabrafenib: May decrease the serum concentration of Progestins (Contraceptive). Management: Females of reproductive potential should use an alternative, highly effective, non-hormonal means of contraception during and at least 2 weeks (dabrafenib alone) or 4 months (dabrafenib + trametinib) after discontinuation of dabrafenib treatment. Consider therapy modification
Darunavir: May decrease the serum concentration of Norethindrone. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Efavirenz: May decrease the serum concentration of Progestins (Contraceptive). Management: Use an alternative or additional method of contraception due to possibly decreased contraceptive effectiveness. Injected depot medroxyprogesterone acetate does not appear to participate in this interaction. Consider therapy modification
Elexacaftor, Tezacaftor, and Ivacaftor: Hormonal Contraceptives may enhance the adverse/toxic effect of Elexacaftor, Tezacaftor, and Ivacaftor. Specifically, the risk for rash may be increased. Monitor therapy
Encorafenib: May decrease the serum concentration of Progestins (Contraceptive). Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Eslicarbazepine: May decrease the serum concentration of Progestins (Contraceptive). Management: Alternative, non-hormonal means of birth control should be considered for women of child-bearing potential. Consider therapy modification
Exenatide: May decrease the serum concentration of Progestins (Oral Contraceptive). Management: Administer oral contraceptives at least one hour prior to exenatide. Consider therapy modification
Felbamate: May decrease the serum concentration of Progestins (Contraceptive). Management: Contraceptive failure is possible. Use of an alternative, nonhormonal method of contraception is recommended. Consider therapy modification
Flibanserin: Progestins (Contraceptive) may increase the serum concentration of Flibanserin. Monitor therapy
Fosamprenavir: Progestins (Contraceptive) may decrease serum concentrations of the active metabolite(s) of Fosamprenavir. Fosamprenavir may decrease the serum concentration of Progestins (Contraceptive). Management: Consider using an alternative or additional means of contraception. Injected depot medroxyprogesterone acetate may be used without a need for additional contraception. Consider therapy modification
Fosaprepitant: May decrease the serum concentration of Progestins (Contraceptive). The active metabolite aprepitant is likely responsible for this effect. Management: Alternative or additional methods of contraception should be used both during treatment with aprepitant or fosaprepitant and for at least one month following the last aprepitant/fosaprepitant dose. Consider therapy modification
Fosphenytoin: May diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Contraceptive failure is possible. Use of an alternative, nonhormonal contraceptive is recommended. Consider therapy modification
Griseofulvin: May diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Avoid combination
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Herbs (Progestogenic Properties) (eg, Bloodroot, Yucca): May enhance the adverse/toxic effect of Progestins. Monitor therapy
Indium 111 Capromab Pendetide: Luteinizing Hormone-Releasing Hormone Analogs may diminish the diagnostic effect of Indium 111 Capromab Pendetide. Avoid combination
Ivosidenib: May decrease the serum concentration of Progestins (Contraceptive). Management: Consider alternative methods of contraception (ie, non-hormonal) in patients receiving ivosidenib. Consider therapy modification
Ixazomib: May decrease the serum concentration of Progestins (Contraceptive). More specifically, use of ixazomib with dexamethasone may decrease the serum concentrations of contraceptive progestins. Management: Patients of childbearing potential should use a nonhormonal barrier contraceptive during and 90 days following ixazomib treatment. Avoid combination
LamoTRIgine: May decrease the serum concentration of Progestins (Contraceptive). Monitor therapy
Lesinurad: May decrease the serum concentration of Progestins (Contraceptive). Management: Use of an additional, nonhormonal contraceptive is recommended in patients being treated with lesinurad who desire effective contraception. Consider therapy modification
Lixisenatide: May decrease the serum concentration of Progestins (Contraceptive). Management: Administer oral contraceptives 1 hour before or at least 11 hours after administration of lixisenatide. Consider therapy modification
Lopinavir: May decrease the serum concentration of Progestins (Contraceptive). Lopinavir may increase the serum concentration of Progestins (Contraceptive). Management: Consider using an alternative or additional means of contraception. Injected depot medroxyprogesterone acetate and etonogestrel implants may be used without a need for additional contraception. Consider therapy modification
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Lumacaftor and Ivacaftor: May decrease the serum concentration of Hormonal Contraceptives. Management: Do not rely on hormone-based contraceptives with concurrent use of lumacaftor/ivacaftor; an alternative, non-hormonal, method of contraception should be used if this combination is required. Consider therapy modification
Metreleptin: May decrease the serum concentration of Progestins (Contraceptive). Metreleptin may increase the serum concentration of Progestins (Contraceptive). Monitor therapy
MiFEPRIStone: May diminish the therapeutic effect of Progestins (Contraceptive). MiFEPRIStone may increase the serum concentration of Progestins (Contraceptive). Management: Women of childbearing potential should use an effective, nonhormonal means of contraception during and 4 weeks following mifepristone treatment. Consider therapy modification
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Mycophenolate: May decrease the serum concentration of Progestins (Contraceptive). Management: Use of an additional or alternative (nonhormonal) method of contraception should be considered. Consider therapy modification
Nelfinavir: May decrease the serum concentration of Progestins (Contraceptive). Management: Use an alternative or additional method of contraception due to possibly decreased contraceptive effectiveness. Injected depot medroxyprogesterone acetate does not appear to participate in this interaction. Consider therapy modification
OXcarbazepine: May decrease the serum concentration of Progestins (Contraceptive). Management: Contraceptive failure is possible. Use of an additional or alternative, nonhormonal method of contraception is recommended. Consider therapy modification
Perampanel: May decrease the serum concentration of Progestins (Contraceptive). Management: Patients should use an alternative, nonhormonal-based form of contraception both during the concurrent use of perampanel and for 1 month after discontinuing perampanel. Consider therapy modification
Phenytoin: May diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Contraceptive failure is possible. Use of an alternative, nonhormonal contraceptive is recommended. Consider therapy modification
Pitolisant: May decrease the serum concentration of Hormonal Contraceptives. Management: Patients using hormonal contraception should be advised to use an alternative non-hormonal contraceptive method during treatment with pitolisant and for at least 21 days after discontinuation of pitolisant treatment. Consider therapy modification
Pomalidomide: Progestins may enhance the thrombogenic effect of Pomalidomide. Management: Canadian pomalidomide labeling recommends caution with use of hormone replacement therapy and states that hormonal contraceptives are not recommended. US pomalidomide labeling does not contain these specific recommendations. Consider therapy modification
Primidone: May diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Use of alternative, nonhormonal contraceptives is recommended. Consider therapy modification
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Retinoic Acid Derivatives: May diminish the therapeutic effect of Progestins (Contraceptive). Retinoic Acid Derivatives may decrease the serum concentration of Progestins (Contraceptive). Management: Two forms of effective contraception should be used in patients receiving retinoic acid derivatives. Microdosed progesterone-only preparations (ie, minipills that do not contain estrogen) are considered an inadequate method of contraception. Exceptions: Adapalene; Alitretinoin (Topical); Bexarotene (Topical); Tretinoin (Topical). Consider therapy modification
Rifamycin Derivatives: May decrease the serum concentration of Progestins (Contraceptive). Contraceptive failure is possible. Management: Contraceptive failure is possible. Use of an alternative, nonhormonal contraceptive is recommended. Consider therapy modification
Rufinamide: May decrease the serum concentration of Norethindrone. Consider therapy modification
Saquinavir: May decrease the serum concentration of Progestins (Contraceptive). Management: Use an alternative or additional method of contraception due to possibly decreased contraceptive effectiveness. Injected depot medroxyprogesterone acetate does not appear to participate in this interaction. Consider therapy modification
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selegiline: Progestins (Contraceptive) may increase the serum concentration of Selegiline. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
St John's Wort: May diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Consider using a product other than St John's wort. Contraceptive failure is possible. Use of an alternative, nonhormonal contraceptive is recommended. Consider therapy modification
Sugammadex: May decrease the serum concentration of Progestins (Contraceptive). Management: Patients receiving any hormonal contraceptive (oral or non-oral) should use an additional, nonhormonal contraceptive method during and for 7 days following sugammadex treatment. Consider therapy modification
Tazemetostat: May decrease the serum concentration of Hormonal Contraceptives. Management: Women of reproductive potential should use a non-hormonal contraceptive method during treatment with tazemetostat and for 6 months after. Men with female partners should use contraception during treatment and for 3 months after. Consider therapy modification
Tetrahydrocannabinol and Cannabidiol: May decrease the serum concentration of Hormonal Contraceptives. Management: Women using hormonal contraceptives should consider adding a barrier contraceptive due to the potential for tetrahydrocannabinol and cannabidiol to decrease concentrations and effectiveness of hormonal contraceptives. Consider therapy modification
Thalidomide: Progestins (Contraceptive) may enhance the thrombogenic effect of Thalidomide. Monitor therapy
Tipranavir: May increase the serum concentration of Progestins (Contraceptive). Management: Use an alternative or additional method of contraception due to possibly decreased contraceptive effectiveness. Injected depot medroxyprogesterone acetate does not appear to participate in this interaction. Consider therapy modification
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Topiramate: May decrease the serum concentration of Progestins (Contraceptive). Management: Caution patients that this combination may be associated with reduced contraceptive effectiveness. Consider adding an additional (non-hormonal) contraceptive method. Consider therapy modification
Tranexamic Acid: Progestins (Contraceptive) may enhance the thrombogenic effect of Tranexamic Acid. Avoid combination
Triazolam: Hormonal Contraceptives may increase the serum concentration of Triazolam. Monitor therapy
Ulipristal: Progestins may diminish the therapeutic effect of Ulipristal. Ulipristal may diminish the therapeutic effect of Progestins. Management: Ulipristal for uterine fibroids (Canadian indication): avoid progestins within 12 days of stopping ulipristal; as emergency contraceptive (U.S. indication): avoid progestins within 5 days of stopping ulipristal. Avoid combination
Vitamin K Antagonists (eg, warfarin): Progestins (Contraceptive) may diminish the anticoagulant effect of Vitamin K Antagonists. In contrast, enhanced anticoagulant effects have also been noted with some products. Management: When possible, concomitant hormonal contraceptives and coumarin derivatives should be avoided in order to eliminate the risk of thromboembolic disorders. Consider using an alternative, nonhormonal contraceptive. Consider therapy modification
Voriconazole: May increase the serum concentration of Progestins (Contraceptive). Progestins (Contraceptive) may increase the serum concentration of Voriconazole. Monitor therapy
Test Interactions
See individual monographs.
Adverse Reactions
Percentages as reported with combination product. Also see individual agents.
>10%:
Central nervous system: Headache (46% to 51%), depression (27% to 34%), pain (21% to 29%), insomnia (13% to 15%), dizziness (7% to 11%), nervousness (4% to 11%)
Dermatologic: Dermatological reaction (9% to 11%)
Endocrine & metabolic: Hot flash (57% to 87%), decreased HDL cholesterol (41% to 44%), increased serum cholesterol (7% to 20%), androgen-like effect (5% to 18%), breast changes (8% to 13%), increased LDL cholesterol (7% to 11%)
Gastrointestinal: Nausea and vomiting (13% to 29%), change in bowel habits (constipation/diarrhea, 10% to 15%), weight gain (4% to 13%)
Genitourinary: Vaginitis (8% to 15%)
Neuromuscular & skeletal: Weakness (11% to 18%)
1% to 10%:
Cardiovascular: Edema (7% to 9%)
Central nervous system: Memory impairment (2% to 4%)
Endocrine & metabolic: Increased serum triglycerides (9% to 10%), decreased libido (4% to 7%), increased gamma-glutamyl transferase (1%)
Gastrointestinal: Dyspepsia (4% to 7%), change in appetite (6%)
Genitourinary: Irregular menses (≤5%)
Hepatic: Increased serum ALT (2%; ≥2 x ULN)
Local: Injection site reaction (3% to 9%)
Neuromuscular & skeletal: Leg cramps (3% to 9%)
<1%, postmarketing, and/or case reports: Anaphylactoid reaction, asthma, nephrolithiasis, urinary tract infection
Warnings/Precautions
Concerns related to adverse effects:
- Allergic reactions: Anaphylactoid reactions and asthma exacerbations have been reported with therapy in patients with histories of asthma, sinusitis, or environmental or drug allergies.
- Decreased bone density: Leuprolide depot suspension may cause an irreversible loss in bone mineral density (BMD). Norethindrone reduces this loss; however, use of this combination should be limited in duration. The initial therapy should be limited to 6 months duration; a single re-treatment of not more than 6 additional months may be administered if symptoms recur. BMD should be measured prior to re-treatment. Maximum total duration of therapy is 12 months. Use caution in patients with additional risk factors for bone loss (eg, chronic alcohol or tobacco use, strong family history of osteoporosis, chronic use of medications that may decrease BMD such as corticosteroid therapy).
- Endometriosis: Due to the physiologic effects of the drug, exacerbation of endometriosis symptoms may occur after the first dose of leuprolide.
- Seizures: Convulsions have been observed with leuprolide in postmarketing reports; patients affected included both those with and without a history of cerebrovascular disorders, central nervous system anomalies or tumors, epilepsy, seizures, and those on concomitant medications which may lower the seizure threshold. If seizures occur, manage accordingly.
- Visual disturbances: Discontinue norethindrone pending examination if migraine, loss of vision, proptosis, diplopia, or other visual disturbances occur; discontinue this combination permanently if papilledema or retinal vascular lesions are observed on examination.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with risk factors for arterial disease or venous thromboembolism (VTE) (eg, hypertension, hypercholesterolemia, obesity, diabetes, family history of VTE, or women who smoke). Manage risk factors prior to therapy; monitor closely.
- Depression: Use with caution in patients with depression. Depression may occur or worsen during therapy; discontinue if serious depression recurs.
- Diseases exacerbated by fluid retention: Use with caution in patients with diseases which may be exacerbated by fluid retention, including asthma, epilepsy, migraine, diabetes, or cardiac or renal dysfunction.
Special populations:
- Elderly: Not for use in postmenopausal women.
- Pediatric patients: Not for use prior to menarche.
- Pregnancy: Pregnancy must be excluded prior to the start of treatment. Although leuprolide usually inhibits ovulation and stops menstruation, contraception is not ensured and a nonhormonal contraceptive should be used. Advise patients to notify their provider if they suspect or become pregnant.
Dosage form specific issues:
- Injection: Due to differing release characteristics, the 1-month and 3-month depot formulations of leuprolide are not equivalent and cannot be substituted for one another.
Monitoring Parameters
Pregnancy test (prior to therapy); bone mineral density (prior to re-treatment); endometrial-related pain; serum lipids
Pregnancy
Pregnancy Risk Factor
X
Pregnancy Considerations
Use is contraindicated in females who are pregnant or who may become pregnant during therapy.
Pregnancy must be excluded prior to the start of treatment. Although leuprolide usually inhibits ovulation and stops menstruation, contraception is not ensured and a nonhormonal contraceptive should be used during therapy.
Fertility suppression observed with other leuprolide formulations is reversible following discontinuation of therapy. This formulation is indicated to treat pain associated with endometriosis; in infertile women with endometriosis, it does not necessarily improve the ability to conceive (ACOG 2010; Practice Committee ASRM 2012).
Also refer to individual monographs for additional information.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience acne, hot flashes, loss of strength and energy, passing gas, nausea, vomiting, trouble sleeping, breast soreness, leg cramps, hair loss, injection site irritation, constipation, diarrhea, or decreased sex drive. Have patient report immediately to prescriber signs of liver problems (dark urine, feeling tired, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes), signs of severe cerebrovascular disease (change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or change in eyesight), signs of DVT (edema, warmth, numbness, change in color, or pain in the extremities), chest pain, fast heartbeat, severe behavioral changes, severe headache, coughing up blood, dizziness, passing out, vision changes, blindness, bulging eyes, vaginal pain, itching, and discharge, abnormal vaginal bleeding, unable to pass urine, painful urination, seizures, shortness of breath, excessive weight gain, swelling of arms or legs, breast pain, abnormal heartbeat, sweating a lot, depression, mood changes, anxiety, trouble with memory, burning or numbness feeling, or bone pain (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling or face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.