Boxed Warning
Risks from concomitant use with opioids:
Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Concentrate, Oral:
LORazepam Intensol: 2 mg/mL (30 mL) [alcohol free, dye free, sugar free; unflavored flavor]
Generic: 2 mg/mL (30 mL)
Solution, Injection:
Ativan: 2 mg/mL (1 mL, 10 mL); 4 mg/mL (1 mL, 10 mL) [contains benzyl alcohol, polyethylene glycol, propylene glycol]
Generic: 2 mg/mL (1 mL, 10 mL); 4 mg/mL (1 mL, 10 mL)
Tablet, Oral:
Ativan: 0.5 mg
Ativan: 1 mg, 2 mg [scored]
Generic: 0.5 mg, 1 mg, 2 mg
Pharmacology
Mechanism of Action
Binds to stereospecific benzodiazepine receptors on the postsynaptic GABA neuron at several sites within the central nervous system, including the limbic system, reticular formation. Enhancement of the inhibitory effect of GABA on neuronal excitability results by increased neuronal membrane permeability to chloride ions. This shift in chloride ions results in hyperpolarization (a less excitable state) and stabilization. Benzodiazepine receptors and effects appear to be linked to the GABA-A receptors. Benzodiazepines do not bind to GABA-B receptors.
Pharmacokinetics/Pharmacodynamics
Absorption
IM: Rapid and complete absorption; Oral: Readily absorbed
Distribution
IV: Vd: Crosses the blood brain barrier
Neonates: 0.76 ± 0.37 L/kg (range: 0.14 to 1.3 L/kg) (McDermott 1992)
Pediatric patients (Chamberlain 2012):
5 months to < 3 years: 1.62 L/kg (range: 0.67 to 3.4 L/kg)
3 to <13 years: 1.5 L/kg (range: 0.49 to 3 L/kg)
13 to <18 years: 1.27 L/kg (range: 1 to 1.54 L/kg)
Adults: 1.3 L/kg
Metabolism
Hepatic; rapidly conjugated to inactive compounds
Excretion
Urine (~88%; predominantly as inactive metabolites); feces (~7%)
Onset of Action
Anticonvulsant: IV: Within 10 minutes
Hypnosis: IM: 20 to 30 minutes
Sedation: IV: Within 2 to 3 minutes (Greenblatt 1983)
Time to Peak
IM: ≤3 hours; Oral: ~2 hours; Sublingual tablet [Canadian product]: 1 hour
Duration of Action
Anesthesia premedication: Adults: IM, IV: ~6 to 8 hours
Half-Life Elimination
Full-term neonates: IV: 40.2 ± 16.5 hours; range: 18 to 73 hours (McDermott 1992)
Pediatric patients (Chamberlain 2012): IV:
5 months to <3 years: 15.8 hours (range: 5.9 to 28.4 hours)
3 to <13 years: 16.9 hours (range: 7.5 to 40.6 hours)
13 to <18 years: 17.8 hours (range: 8.2 to 42 hours)
Adults: Oral: ~12 hours; IV: ~14 hours; IM: ~13 to 18 hours (Greenblatt 1983); End-stage renal disease (ESRD): ~18 hours
Protein Binding
~91
Use: Labeled Indications
Anxiety (oral): Management of anxiety disorders or short-term (≤4 months) relief of anxiety.
Procedural anxiety, premedication (injection): Anesthesia premedication in adults to relieve anxiety or to produce amnesia (diminish recall) or sedation.
Status epilepticus (injection): Treatment of status epilepticus. May be used off label for acute seizures that have not yet progressed to status epilepticus.
Use: Off Label
Akathisia, antipsychotic-inducedcyes
Data from a limited number of open-label clinical trials suggest that lorazepam may be beneficial for the treatment of patients with antipsychotic-induced akathisia Adler 1985, Bartels 1987.
Based on the World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of schizophrenia, oral benzodiazepines are suggested in the treatment of antipsychotic-induced akathisia; however, the risk of drug tolerance and dependence and the potential for increased mortality when combining benzodiazepines and antipsychotics should be considered WFSBP [Hasan 2013].
Alcohol withdrawal syndromebyes
Data from a limited number of randomized, double-blind, active-comparator trials and a comparative trial of lorazepam dosing regimens support fixed-dose and symptom-triggered regimens of lorazepam for decreasing withdrawal symptoms for patients with alcohol withdrawal syndrome Malcolm 2002, Myrick 2009, Sachdeva 2014.
Based on the WFSBP guidelines for biological treatment of substance use and related disorders and American Society of Addiction Medicine guidelines for the pharmacological management of alcohol withdrawal, lorazepam is effective and recommended in the management of this condition ASAM [Mayo-Smith 1997], WFSBP [Soyka 2017].
Catatoniac
Data from a limited number of patients studied suggest that lorazepam may be beneficial for the treatment of catatonia Bush 1996, England 2011. Additionally, data from a limited number of patients in a single, open-label study suggest that a test dose of parenteral lorazepam may predict response to lorazepam for the treatment of catatonia Bush 1996.
Based on the WFSBP guidelines for biological treatment of schizophrenia, benzodiazepines, such as lorazepam, are first-line treatment for catatonia WFSBP [Hasan 2012].
Chemotherapy-induced nausea and vomitingyes
Based on the American Society of Clinical Oncology antiemetic guidelines for chemotherapy-induced nausea and vomiting, lorazepam may be given as an adjunct to other antiemetic medications for the management of chemotherapy-induced nausea and vomiting and for the management of breakthrough episodes that occur despite optimal prophylaxis in patients who have already received olanzapine.
Insomnia, sleep-onset or sleep-maintenancecyes
Data from a limited number of patients studied in double-blind, randomized trials suggest that lorazepam may be beneficial for the treatment of sleep-onset or sleep-maintenance insomnia Lorizio 1986, McClure 1988, Wang 1976.
Based on the European Sleep Research Society guideline for the diagnosis and treatment of insomnia, benzodiazepines are effective in the short-term treatment of insomnia; however, long-term treatment is not recommended based on lack of evidence and possible adverse effects and risks ESRS [Riemann 2017].
Intoxication: Cocaine, methamphetamine, and other sympathomimeticsyes
Based on German consensus- and evidence-based guidelines for the treatment of methamphetamine-related toxicity, benzodiazepines such as lorazepam are first-line agents for methamphetamine intoxication, particularly in cases of acute agitation or aggression Wodarz 2017. Other experts also recommend benzodiazepines for agitation, seizures, hypertension, and tachycardia associated with intoxication from cocaine and other sympathomimetics Akerele 2017.
Neuroleptic malignant syndromec
Data from a limited number of patients studied in case reports suggest that lorazepam may be beneficial for the treatment of muscle rigidity and agitation caused by neuroleptic malignant syndrome Khaldarov 2000, Tsai 2010. Some experts suggest use of benzodiazepines in patients with severe symptoms (eg, muscle rigidity, agitation, hyperthermia) not responsive to supportive therapies Ware 2018, Wijdicks 2019.
Opioid withdrawalc
Data from a limited number of patients studied in case reports suggest that lorazepam may be beneficial for the treatment of opioid withdrawal; some experts recommend benzodiazepines for management of agitation and autonomic instability associated with opioid withdrawal Hanna 2018, Stolbach 2019, Wightman 2018.
Sedation/agitation, critical illnessbyes
Data from randomized, comparator trials and a propensity-matched study suggest that lorazepam may be beneficial for the management of sedation and agitation in critical illness; however, lorazepam is associated with longer duration of mechanical ventilation or ICU stay, increased delirium, and higher mortality when compared to nonbenzodiazepine regimens Carson 2006, Lonardo 2014, Pandharipande 2007.
Based on the Society of Critical Care Medicine clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU, propofol or dexmedetomidine are preferred over benzodiazepines (ie, lorazepam) for sedation in critically ill, mechanically ventilated adults SCCM [Devlin 2018].
Serotonin syndrome (serotonin toxicity)c
Data from a limited number of patients studied in case reports suggest that lorazepam may be beneficial for the treatment of altered mental state, autonomic instability, and muscle rigidity caused by serotonin syndrome Frank 2008, Levin 2008. Additionally, experts recommend use of benzodiazepines for symptomatic management (eg, muscle rigidity, agitation, hyperthermia, autonomic instability, tremor) of serotonin syndrome Boyer 2019a, Tormoehlen 2018, Wang 2016.
Vertigo, acute episodes, treatmentc
Data from a limited number of randomized, double-blind clinical trials suggest that lorazepam may be beneficial for the treatment of vertigo Amini 2014, Marill 2000.
Based on the American Academy of Otolaryngology—Head and Neck Surgery Foundation clinical practice guideline for benign paroxysmal positional vertigo (BPPV), benzodiazepines, including lorazepam, are not routinely recommended for the treatment of BPPV based on limited evidence and the risk-benefit profile. Use may be considered for short-term management of severe symptoms (eg, nausea and vomiting), for patients refusing other treatment options, and for patients requiring prophylaxis for canalith repositioning procedures Bhattacharyya 2017.
Contraindications
Hypersensitivity to lorazepam, any component of the formulation, or other benzodiazepines (cross-sensitivity with other benzodiazepines may exist); acute narrow-angle glaucoma; severe respiratory insufficiency (except during mechanical ventilation)
Parenteral: Additional contraindications: Hypersensitivity to polyethylene glycol, propylene glycol, or benzyl alcohol; sleep apnea; intra-arterial injection; use in premature infants
Canadian labeling: Additional contraindications (not in the US labeling): Myasthenia gravis
Dosage and Administration
Dosing: Adult
Note: Avoid use in patients with, or at risk for, substance abuse disorders, except for acute or emergency situations (eg, acute agitation, status epilepticus).
Akathisia, antipsychotic-induced (alternative agent) (off-label use): IV, Oral: Initial: 0.5 to 1 mg twice daily; may increase dose based on response and tolerability up to 10 mg/day (Adler 1985; Bartels 1987; Marder 2019).
Anxiety:
Anxiety and agitation, acute/severe (monotherapy or adjunctive therapy): IM, IV, Oral: 0.5 to 2 mg every 4 to 6 hours as needed up to 10 mg/day; adjust dose based on response and tolerability. In severely agitated inpatients, some experts recommend doses up to 4 mg and repeat IM or IV doses as frequently as 10 to 30 minutes; may give alone or in combination with an antipsychotic (Moore 2019).
Anxiety disorder (monotherapy or adjunctive therapy) (alternative agent): Note: Most commonly used short-term for immediate symptom relief until concurrent therapy is effective (eg, ≤12 weeks). Long-term therapy may be considered for select patients only when other treatments are ineffective or poorly tolerated (Katzman 2014; WFSBP [Bandelow 2008]).
Oral: Initial: 0.5 to 1 mg 2 to 3 times daily; increase gradually based on response and tolerability up to 6 mg/day in 2 to 4 divided doses; some patients may require doses up to 10 mg/day for optimal response (Bystritsky 2019; manufacturer's labeling).
Advanced cancer and/or palliative care: IM, IV, Oral: 0.25 to 2 mg every 3 to 6 hours as needed (Irwin 2019; Roy-Byrne 2019). Note: The injectable solution may be administered rectally or subcutaneously, and the tablet and oral solution may be administered sublingually at the same doses when other routes are unavailable (Caillé 1983; Graves 1987; Greenblatt 1982; Harman 2019; Howard 2014; von Gunten 2019).
Performance- or phobia-related anxiety (monotherapy or adjunctive therapy): Note: Provide a test dose, at the same dose to be used for treatment, in advance of the stimulus to ensure tolerability (Stein 2019).
Oral: 0.5 to 2 mg once 30 to 60 minutes before the stimulus (Stein 2019; Swinson 2019).
Procedural anxiety (premedication) (off-label use):
Oral, Sublingual: 0.5 to 2 mg once 30 to 90 minutes before procedure; if needed due to incomplete response, may repeat the dose (usually at 50% of the initial dose) after 30 to 60 minutes (Chang 2015; Choy 2019; Male 1984; Shih 2019).
IV: 1 to 4 mg or 0.02 to 0.04 mg/kg (maximum single dose: 4 mg) once 5 to 20 minutes before procedure; if needed based on incomplete response and/or duration of procedure, may repeat the dose (usually at 50% of the initial dose) after ≥5 minutes (Choy 2019; manufacturer's labeling). Note: In obese patients, non–weight-based dosing is preferred (Choy 2019).
Catatonia (off-label use):
Diagnosis: Note: Partial, temporary relief of signs following administration is consistent with the diagnosis; a negative response does not rule out catatonia (Coffey 2019a).
IV (preferred): 1 to 2 mg once; if no response in 5 to 10 minutes, repeat dose once (Coffey 2019a; Fink 2009; Rosebush 2010).
IM, Oral, Sublingual: 2 mg once; may administer up to 2 additional doses at 3-hour intervals if needed (Coffey 2019a; Rosebush 2010).
Treatment: Note: For patients with malignant catatonia, electroconvulsive therapy should begin immediately (WFSBP [Hasan 2012]).
IM, IV, Oral: Initial: 1 to 2 mg 3 times daily; IV preferred for initial dosing with switch to oral as patient improves. May increase dose based on response and tolerability in increments of 3 mg every 1 to 2 days to a usual dose of 6 to 21 mg/day. Doses up to 30 mg/day have been reported (Coffey 2019b; Daniels 2009; Fink 2009). For patients at risk of cardiorespiratory compromise or oversedation, some experts recommend initiating with 0.5 mg 3 times daily (Coffey 2019b; WFSBP [Hasan 2012]).
Duration of treatment: Remission is usually achieved in 4 to 10 days; maintenance therapy at the effective dose is usually continued for 3 to 6 months to maintain recovery, although longer courses may be needed (Coffey 2019b).
Chemotherapy-induced nausea and vomiting, prevention and treatment (adjunctive therapy) (off-label use):
Anticipatory or breakthrough nausea/vomiting, as an adjunct to conventional antiemetics: Oral, IV, Sublingual: 0.5 to 2 mg every 6 hours as needed (Lohr 2008).
Insomnia, sleep-onset or sleep-maintenance (alternative treatment) (off-label use): Note: Intended for short-term use (≤4 to 8 weeks), preferably in conjunction with nonpharmacologic therapies (ACP [Qaseem 2016]; Bonnet 2019; ESRS [Riemann 2017]). Chronic use should be limited to cases where nonpharmacologic treatments are not available or not effective and benefits are felt to outweigh risks (AASM [Sateia 2017]). Some experts advise against extended use of pharmacologic therapy for insomnia (ACP [Qaseem 2016]).
Oral: 0.5 to 2 mg at bedtime (Bonnet 2019; Winkelman 2015).
Intoxication: Cocaine, methamphetamine, and other sympathomimetics (off-label use): Based on limited data: IV: 2 to 4 mg every 3 to 10 minutes as needed for agitation, sedation, seizures, hypertension, and tachycardia until desired symptom control achieved. Large cumulative doses may be required for some patients; monitor for respiratory depression and hypotension (Arnold 2019; Boyer 2019b; Nelson 2019; Wodarz 2017). Note: Initiating treatment at 1 mg may be adequate in patients who are only mildly or moderately intoxicated, but doses should be repeated or increased as needed. Consider IM administration if IV access is not possible; however, effects will be delayed (Arnold 2019).
Neuroleptic malignant syndrome (adjunctive therapy) (off-label use): Note: For management of muscle rigidity or anxiety in patients with severe symptoms at presentation (hyperthermia, evidence of rhabdomyolysis) and for those not responding to initial withdrawal of medication and supportive care:
IM, IV: 0.5 to 2 mg every 4 to 6 hours until symptom resolution. Use higher doses (eg, 1 to 2 mg) for management of muscle rigidity (Wijdicks 2019).
Sedation/agitation, critical illness (alternative agent) (off-label use): Note: Titrate to light level of sedation (eg, Richmond Agitation-Sedation Scale 0 to −2). Intermittent as-needed therapy is preferred to avoid oversedation (SCCM [Devlin 2018]). For obese patients, fixed dosing is preferred; alternatively, some use IBW for weight-based dosing (Tietze 2019). Continuous infusions are not recommended for use in most ICU patients due to propylene glycol (PG) accumulation and subsequent complications (osmol gap metabolic acidosis, kidney failure); monitor PG accumulation with osmol gap; nonbenzodiazepine or midazolam continuous infusions are generally preferred (Arroliga 2004; Barnes 2006; Yahwak 2008).
Intermittent (preferred):
Fixed dose: IV: Initial dose: 1 to 4 mg; Maintenance: 1 to 4 mg every 2 to 6 hours as needed (Carson 2006; Tietze 2019).
Weight based: IV: Initial dose: 0.02 to 0.04 mg/kg (maximum single dose: 4 mg); Maintenance: 0.02 to 0.06 mg/kg every 2 to 6 hours as needed (maximum single dose: 4 mg) (Carson 2006; Cernaianu 1996; Rozendaal 2009; SCCM [Barr 2013]; Tietze 2019).
Continuous: IV: 0.01 to 0.1 mg/kg/hour continuous infusion (maximum dose: 10 mg/hour) (Rozendaal 2009; SCCM [Barr 2013]; Tietze 2019).
Seizures: Note: If IV access is not available, IM lorazepam is not recommended due to erratic absorption and a slow time to peak drug levels. May consider sublingual or subcutaneous lorazepam or IM midazolam (Drappatz 2019; Harman 2019; Leppik 2015).
Acute active seizures (non-status epilepticus) (off-label use): IV: 4 mg given at a maximum rate of 2 mg/minute; may repeat at 3 to 5 minutes if seizures continue (Drislane 2019; McKee 2015; O’Connor 2019; Schachter 2019).
Status epilepticus: IV: 4 mg given at a maximum rate of 2 mg/minute; may repeat at 3 to 5 minutes if seizures continue; a nonbenzodiazepine antiseizure agent should follow to prevent seizure recurrence, even if seizures have ceased (Drislane 2019; manufacturer's labeling).
Serotonin syndrome (serotonin toxicity) (off-label use): IV: 2 to 4 mg IV every 8 to 10 minutes based upon patient response (Boyer 2019a).
Substance withdrawal:
Alcohol withdrawal syndrome (alternative agent) (off-label use): Note: Symptom-triggered regimens preferred over fixed-dose regimens. Dosage and frequency may vary based on institution-specific protocols. Although longer-acting benzodiazepines are preferred in general, shorter-acting benzodiazepines, including lorazepam, may be preferable in patients with impaired liver function. Some experts recommend avoiding IM administration due to variable absorption (Hoffman 2019; WFSBP [Soyka 2017]).
Symptom-triggered regimen: Oral, IV: 2 to 4 mg as needed; dose and frequency determined by withdrawal symptom severity using a validated severity-assessment scale such as the Clinical Institute Withdrawal Assessment for Alcohol, revised scale (CIWA-Ar) (Hoffman 2019; WFSBP [Soyka 2017]).
Fixed-dose regimen: Oral, IV: 6 to 8 mg/day in divided doses for 1 day, then gradually taper dose over 3 to 4 days; additional doses may be considered based on withdrawal symptoms and validated assessment scale scores (eg, CIWA-Ar) (Malcolm 2002; Myrick 2009; WFSBP [Soyka 2017]).
Opioid withdrawal (autonomic instability and agitation) (adjunctive therapy) (alternative agent) (off-label use): Based on limited data: IV: 1 to 2 mg every 10 minutes until hemodynamically stable and adequate sedation (Hanna 2018; Stolbach 2019; Wightman 2018).
Vertigo, acute episodes, treatment (alternative agent) (off-label use): IM, IV, Oral: 0.5 to 2 mg every 4 to 12 hours as needed for 24 to 48 hours (Furman 2019; Hain 2003; Swartz 2005).
Discontinuation of therapy: In patients receiving extended- or higher-dose benzodiazepine therapy, unless safety concerns require a more rapid withdrawal, gradually withdraw to detect reemerging symptoms and minimize rebound and withdrawal symptoms. Taper total daily dose by 10% to 20% every 1 to 2 weeks based on response and tolerability. The optimal taper rate and duration will vary; durations up to 6 months may be necessary for some patients on higher doses (Bystritsky 2019; Lader 2011; VA/DoD 2015). For patients on high doses, taper more rapidly in the beginning and slow the reduction rate as the taper progresses. For example, reduce the dose weekly by 25% until half of the dose remains. Thereafter, continue to reduce by ~12% every 4 to 7 days. For benzodiazepines with half-lives significantly less than 24 hours, including lorazepam, consider substituting an equivalent dose of a long-acting benzodiazepine to allow for a more gradual reduction in drug serum concentrations (VA/DoD 2015).
Dosing: Geriatric
Refer to adult dosing. Dose selection should generally be on the low end of the dosage range (initial dose not to exceed 2 mg).
Dosing: Pediatric
Chemotherapy-induced nausea and vomiting, anticipatory: Limited data available: Infants, Children, and Adolescents: Oral: 0.04 to 0.08 mg/kg/dose; maximum dose: 2 mg/dose; administer a dose the night before chemotherapy and again the next day prior to chemotherapy administration (Dupuis 2014).
Chemotherapy-associated nausea and vomiting, breakthrough: Limited data available: Children and Adolescents: IV: 0.025 to 0.05 mg/kg/dose every 6 hours as needed; maximum dose: 2 mg/dose (Dupuis 2003).
Anxiety, acute:
Infants and Children <12 years: Limited data available: Oral, IV: Usual: 0.05 mg/kg/dose (maximum dose: 2 mg/dose) every 4 to 8 hours; range: 0.02 to 0.1 mg/kg/dose (Kliegman 2007).
Children ≥12 years and Adolescents: Oral: 0.25 to 2 mg/dose 2 or 3 times daily; maximum dose: 2 mg/dose (Kliegman 2011).
Sedation (preprocedure): Limited data available: Children and Adolescents: Oral: Usual: 0.05 mg/kg; range reported in literature: 0.02 to 0.09 mg/kg (Burtles 1983; Henry 1991; Mundeleer 1980; Peters 1982). Note: In adults, the maximum dose is 4 mg/dose.
Status epilepticus: Limited data available:
IV: Infants, Children, and Adolescents: 0.1 mg/kg slow IV; may repeat dose once in 5 to 10 minutes; maximum dose: 4 mg/dose (AES [Glauser 2016]; NCS [Brophy 2012]).
Intranasal: Note: Lorazepam is not the preferred agent for intranasal administration, guidelines recommend midazolam as the preferred agent (AES [Glauser 2016]).
Infants, Children, and Adolescents: 0.1 mg/kg/dose; maximum dose: 5 mg/dose (Ahmad 2006; Arya 2011; Kliegman 2020).
Dosing adjustment for lorazepam with concomitant medications: Children ≥12 years and Adolescents: Probenecid or valproic acid: Reduce lorazepam dose by 50%.
Reconstitution
IV injection: According to the manufacturer, dilute IV dose prior to use with an equal volume of compatible diluent (D5W, NS, SWFI).
Infusion: Precipitation may occur upon dilution when preparing an infusion. Use 2 mg/mL injectable vial to prepare; there may be decreased stability when using 4 mg/mL vial. Dilute to ≤1 mg/mL with a compatible diluent in a non-PVC (eg, polyolefin, glass) container (consult parenteral admixture resource for additional detailed recommendations). Can also be administered undiluted (up to 4 mg/mL) via infusion into a central vein or into a peripheral vein with a running compatible maintenance IV solution (Johnson 2002).
IM: Administer undiluted.
Extemporaneously Prepared
Note: Commercial oral solution is available (2 mg/mL)
Two different 1 mg/mL oral suspensions may be made from different generic lorazepam tablets (Mylan Pharmaceuticals or Watson Laboratories), sterile water, Ora-Sweet, and Ora-Plus.
Mylan tablets: Place one-hundred-eighty 2 mg tablets in a 12-ounce amber glass bottle; add 144 mL of sterile water to disperse the tablets; shake until slurry is formed. Add 108 mL Ora-Plus in incremental proportions; then add a quantity of Ora-Sweet sufficient to make 360 mL. Label "shake well" and "refrigerate". Stable for 91 days when stored in amber glass prescription bottles at room temperature or refrigerated (preferred).
Watson tablets: Place one-hundred-eighty 2 mg tablets in a 12-ounce amber glass bottle; add 48 mL sterile water to disperse the tablets; shake until slurry is formed. Add 156 mL of Ora-Plus in incremental proportions; then add a quantity of Ora-Sweet sufficient to make 360 mL. Label "shake well" and "refrigerate". Store in amber glass prescription bottles. Stable for 63 days at room temperature or 91 days refrigerated.
Lee WM, Lugo RA, Rusho WJ, Mackay M, Sweeley J. Chemical stability of extemporaneously prepared Lorazepam suspension at two temperatures. J Pediatr Pharmacol Ther. 2004;9(4):254-258.
Administration
IM: Should be administered (undiluted) deep into the muscle mass.
IV injection: Dilute prior to use (according to the manufacturer). Do not exceed 2 mg/minute or 0.05 mg/kg over 2 to 5 minutes. Monitor IV site during administration. Avoid intra-arterial administration. Avoid extravasation.
Oral: Oral concentrate: Use only the provided calibrated dropper to withdraw the prescribed dose. Mix the dose with liquid (eg, water, juice, soda, soda-like beverage) or semisolid food (eg, applesauce, pudding), and stir for a few seconds to blend completely. The prepared mixture should be administered immediately.
SubQ: Some experts administer the injectable solution subcutaneously when other routes are unavailable (eg, comfort care settings) (von Gunten 2019).
Rectal: Injectable solution may be administered rectally when other routes are unavailable (eg, comfort care settings) (Graves 1987).
Sublingual:
Oral concentrate: May be administered sublingually when other routes are unavailable (eg, comfort care settings (Howard 2014).
Oral tablet: May be administered sublingually when other routes are unavailable (eg, comfort care settings (Greenblatt 1982).
Sublingual tablet [Canadian product]: Place under tongue; patient should not swallow for at least 2 minutes.
Storage
Parenteral: Intact vials should be refrigerated (room temperature storage information may be available; contact product manufacturer to obtain current recommendations). Protect from light. Parenteral admixture in D5W, LR, or NS is stable at room temperature (25°C) for 24 hours (consult parenteral admixture resource for additional detail).
Oral concentrate: Store at colder room temperature or refrigerate at 2°C to 8°C (36°F to 46°F). Discard open bottle after 90 days.
Oral tablet: Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F).
Sublingual tablet [Canadian product]: Store at 15°C to 25°C (59°F to 77°F). Protect from light.
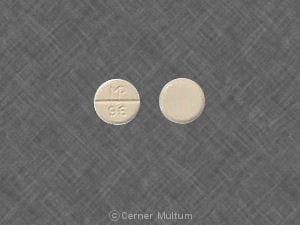
LORazepam Images
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CloZAPine: Benzodiazepines may enhance the adverse/toxic effect of CloZAPine. Management: Consider decreasing the dose of (or possibly discontinuing) benzodiazepines prior to initiating clozapine. Consider therapy modification
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Fexinidazole [INT]: May increase the serum concentration of Products Containing Propylene Glycol. Avoid combination
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosphenytoin: Benzodiazepines may increase the serum concentration of Fosphenytoin. Short-term exposure to benzodiazepines may not present as much risk as chronic therapy. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Loxapine: May enhance the adverse/toxic effect of LORazepam. Specifically, prolonged stupor, respiratory depression, and/or hypotension. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Melatonin: May enhance the sedative effect of Benzodiazepines. Monitor therapy
Methadone: Benzodiazepines may enhance the CNS depressant effect of Methadone. Management: Clinicians should generally avoid concurrent use of methadone and benzodiazepines when possible; any combined use should be undertaken with extra caution. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetroNIDAZOLE (Systemic): May enhance the adverse/toxic effect of Products Containing Propylene Glycol. A disulfiram-like reaction may occur. Avoid combination
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
OLANZapine: May enhance the adverse/toxic effect of Benzodiazepines. Management: Avoid concomitant use of parenteral benzodiazepines and IM olanzapine due to risks of additive adverse events (e.g., cardiorespiratory depression). Olanzapine prescribing information provides no specific recommendations regarding oral administration. Avoid combination
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Phenytoin: Benzodiazepines may increase the serum concentration of Phenytoin. Short-term exposure to benzodiazepines may not present as much risk as chronic therapy. Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Probenecid: May increase the serum concentration of LORazepam. Consider therapy modification
Pyrimethamine: LORazepam may enhance the hepatotoxic effect of Pyrimethamine. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: Benzodiazepines may enhance the CNS depressant effect of Sodium Oxybate. Avoid combination
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Teduglutide: May increase the serum concentration of Benzodiazepines. Monitor therapy
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Theophylline Derivatives: May diminish the therapeutic effect of Benzodiazepines. Consider therapy modification
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Valproate Products: May increase the serum concentration of LORazepam. Consider therapy modification
Yohimbine: May diminish the therapeutic effect of Antianxiety Agents. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
>10%:
Central nervous system: Drowsiness, sedation
Local: Pain at injection site (IM: 1% to 17%; IV: 2%)
Miscellaneous: Paradoxical reaction
1% to 10%:
Cardiovascular: Hypotension (≤2%)
Central nervous system: Dizziness (7%), unsteadiness (3%), hallucinations (1%), coma (≤1%), confusion (≤1%), delirium (≤1%), depression (≤1%), excessive crying (≤1%), headache (≤1%), restlessness (≤1%), stupor (≤1%)
Local: Erythema at injection site (2%)
Neuromuscular & skeletal: Asthenia (≤4%)
Respiratory: Respiratory failure (2%), apnea (1%), hypoventilation (≤1%)
Frequency not defined:
Central nervous system: Disinhibition, disorientation, drug dependence, dysarthria, dysautonomia, euphoria, extrapyramidal reaction, fatigue, hypothermia, memory impairment, sleep apnea (exacerbation), slurred speech, suicidal ideation, suicidal tendencies, vertigo, withdrawal syndrome
Dermatologic: Alopecia, skin rash
Endocrine & metabolic: Change in libido, hyponatremia, increased lactate dehydrogenase, SIADH
Gastrointestinal: Changes in appetite, constipation
Genitourinary: Impotence, orgasm disturbance
Hematologic & oncologic: Agranulocytosis, leukopenia, pancytopenia
Hepatic: Increased serum bilirubin, increased serum transaminases, jaundice
Hypersensitivity: Anaphylactoid reaction, anaphylaxis, hypersensitivity reaction
Ophthalmic: Visual disturbance
Respiratory: Exacerbation of chronic obstructive pulmonary disease), respiratory depression
<1%, postmarketing, and/or case reports: Abnormal gait, abnormal hepatic function tests, abnormality in thinking, acidosis, agitation, amnesia, ataxia, blurred vision, bradycardia, cardiac arrhythmia, cardiac failure, cerebral edema, chills, cystitis, diplopia, disorder of hemostatic components of blood, gastrointestinal hemorrhage, hearing loss, heart block, hepatotoxicity, hypertension, hyperventilation, increased serum alkaline phosphatase, infection, injection site reaction, myoclonus, nausea, nervousness, neuroleptic malignant syndrome, paralysis, pericardial effusion, pheochromocytoma (aggravation), pneumothorax, propylene glycol toxicity (IV), pulmonary edema, pulmonary hemorrhage, pulmonary hypertension, seizure, sialorrhea, tachycardia, thrombocytopenia, tremor, urinary incontinence, ventricular arrhythmia, vomiting
Warnings/Precautions
Concerns related to adverse effects:
- Anterograde amnesia: Benzodiazepines have been associated with anterograde amnesia (Nelson 1999).
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Paradoxical reactions: Paradoxical reactions, including hyperactive or aggressive behavior, have been reported with benzodiazepines; risk may be increased in adolescent/pediatric patients, geriatric patients, or patients with a history of alcohol use disorder or psychiatric/personality disorders (Mancuso 2004).
- Sleep-related activities: Hazardous sleep-related activities, such as sleep-driving, cooking and eating food, and making phone calls while asleep, have been noted with benzodiazepines (Dolder 2008).
Disease-related concerns:
- Drug abuse: Risk of dependence increases in patients with a history of alcohol or drug abuse and those with significant personality disorders; use with caution in these patients. Tolerance, psychological and physical dependence may also occur with higher dosages and prolonged use. The risk of dependence is decreased with short-term treatment (2 to 4 weeks); evaluate the need for continued treatment prior to extending therapy duration.
- Hepatic impairment: Use with caution in patients with hepatic impairment, insufficiency, and/or encephalopathy. Dose adjustment (lower doses) may be needed. May worsen hepatic encephalopathy.
- Psychiatric disorders: Preexisting depression may emerge or worsen during therapy. Not recommended for use in primary depressive or psychotic disorders. Should not be used in patients at risk for suicide without adequate antidepressant treatment.
- Renal impairment: Use with caution in patients with renal impairment.
- Respiratory disease: Use with caution in patients with respiratory disease, including chronic obstructive pulmonary disease or sleep apnea. Benzodiazepines may cause significant respiratory depression.
Concurrent drug therapy issues:
- Concomitant use with opioids: [US Boxed Warning]: Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation. In patients already receiving an opioid analgesic, prescribe a lower initial dose of lorazepam than indicated in the absence of an opioid and titrate based on clinical response. If an opioid is initiated in a patient already taking lorazepam, prescribe a lower initial dose of the opioid and titrate based upon clinical response.
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Debilitated patients: Use with caution in debilitated patients; initial doses should be at the lower end of dosing range.
- Elderly patients: Elderly patients may be at an increased risk of death with use; risk has been found highest within the first 4 months of use in elderly dementia patients (Jennum 2015; Saarelainen 2018).
- Fall risk: Use with extreme caution in patients who are at risk of falls; benzodiazepines have been associated with falls and traumatic injury (Nelson 1999).
- Pediatrics: In pediatric and neonatal patients <3 years of age, the repeated or lengthy exposure to sedatives or anesthetics during surgery/procedures may have detrimental effects on the child's brain development and may contribute to various cognitive and behavioral problems. Epidemiological studies have reported various cognitive and behavioral problems, including neurodevelopmental delay (and related diagnoses), learning disabilities, and ADHD. Clinical data suggest that single, relatively short exposures are not likely to have similar negative effects. Further studies are needed to fully characterize findings and ensure that these findings are not related to underlying conditions or the procedure itself. No specific anesthetic/sedative has been found to be safer. For elective procedures, risk versus benefits should be evaluated and discussed with parents/caregivers/patients; critical surgeries should not be delayed (FDA 2016).
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein-binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol with caution in neonates. See manufacturer's labeling.
- Polyethylene glycol: Parenteral formulation may contain polyethylene glycol. May be associated with toxicity in high-dose and/or longer-term therapy.
- Propylene glycol: Parenteral formulation may contain propylene glycol; large amounts are potentially toxic and have been associated with hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP 1997; Zar 2007). See manufacturer's labeling. May consider using enteral delivery of lorazepam tablets to decrease the risk of propylene glycol toxicity (Lugo 1999).
Other warnings/precautions:
- Appropriate use: Does not have analgesic, antidepressant, or antipsychotic properties. Status epilepticus should not be treated with injectable benzodiazepines alone; requires close observation and management and possibly ventilatory support. When used as a component of preanesthesia, monitor for heavy sedation and airway obstruction; equipment necessary to maintain airway and ventilatory support should be available.
- Hypnotic: Appropriate use: As a hypnotic, should be used only after evaluation of potential causes of sleep disturbance. Failure of sleep disturbance to resolve after 7 to 10 days may indicate psychiatric or medical illness. A worsening of insomnia or the emergence of new abnormalities of thought or behavior may represent unrecognized psychiatric or medical illness and requires immediate and careful evaluation.
- Tolerance: Lorazepam is a short half-life benzodiazepine. Duration of action after a single dose is determined by redistribution rather than metabolism. Tolerance develops to the sedative, hypnotic, and anticonvulsant effects. It does not develop to the anxiolytic effects (Vinkers 2012). Chronic use of this agent may increase the perioperative benzodiazepine dose needed to achieve desired effect.
- Withdrawal: Rebound or withdrawal symptoms may occur following abrupt discontinuation or large decreases in dose. Use caution when reducing dose or withdrawing therapy; decrease slowly and monitor for withdrawal symptoms. Flumazenil may cause acute withdrawal in patients receiving long-term benzodiazepine therapy.
Monitoring Parameters
Respiratory and cardiovascular status, blood pressure, heart rate, symptoms of anxiety
Long-term therapy: CBC, liver function tests, LDH
High-dose or continuous IV use or IV use in patients with renal impairment: Clinical signs of propylene glycol toxicity, serum creatinine, BUN, serum lactate, osmol gap; Note: An osmol gap of ≥10 was predictive of elevated propylene glycol concentrations; values of ≥12 suggest propylene glycol toxicity (Arroliga 2004; Barnes 2006; Yahwak 2008)
Critically ill patients: Assess and adjust sedation according to scoring system (Richmond Agitation-Sedation Scale [RASS] or Sedation-Agitation Scale [SAS]) (SCCM [Devlin 2018]).
Pregnancy
Pregnancy Considerations
Lorazepam and its metabolite cross the human placenta. Teratogenic effects in humans have been observed with some benzodiazepines (including lorazepam); however, additional studies are needed. The incidence of premature birth and low birth weights may be increased following maternal use of benzodiazepines; hypoglycemia and respiratory problems in the neonate may occur following exposure late in pregnancy. Neonatal withdrawal symptoms may occur within days to weeks after birth and “floppy infant syndrome” (which also includes withdrawal symptoms) have been reported with some benzodiazepines (including lorazepam). Elimination of lorazepam in the newborn infant is slow; following in utero exposure, term infants may excrete lorazepam for up to 8 days (Bergman 1992; Iqbal 2002; Wikner 2007).
Patient Education
What is this drug used for?
- It is used to treat anxiety.
- It is used to treat seizures.
- It is used to ease anxiety before surgery.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Fatigue
- Headache
- Injection site irritation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, emotional instability, or illogical thinking.
- Sensing things that seem real but are not
- Behavioral changes
- Change in balance
- Confusion
- Trouble with memory
- Severe loss of strength and energy
- Severe dizziness
- Passing out
- Vision changes
- Muscle weakness
- Dark urine
- Yellow skin
- Difficulty breathing
- Slow breathing
- Shallow breathing
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.