Boxed Warning
Lactic acidosis
Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. The onset of metformin-associated lactic acidosis is often subtle, accompanied only by nonspecific symptoms such as malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Metformin-associated lactic acidosis was characterized by elevated blood lactate levels (>5 mmol/L), anion gap acidosis (without evidence of ketonuria or ketonemia), and increased lactate/pyruvate ratio; and metformin plasma levels generally >5 mcg/mL.
Risk factors for metformin-associated lactic acidosis include renal impairment, concomitant use of certain drugs (eg, carbonic anhydrase inhibitors such as topiramate), ≥65 years, having a radiological study with contrast, surgery and other procedures, hypoxic states (eg, acute congestive heart failure), excessive alcohol intake, and hepatic impairment.
Steps to reduce the risk of and manage metformin-associated lactic acidosis in these high-risk groups are provided in the full prescribing information.
If metformin-associated lactic acidosis is suspected, immediately discontinue metformin and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Kit, Combination:
D-Care DM2: Extended release tablet, as hydrochloride: 500 mg [DSC]
Solution, Oral, as hydrochloride:
Riomet: 500 mg/5 mL (118 mL, 473 mL) [contains propylene glycol; strawberry flavor]
Riomet: 500 mg/5 mL (118 mL, 473 mL) [contains saccharin calcium; cherry flavor]
Generic: 500 mg/5 mL (473 mL)
Suspension Reconstituted ER, Oral, as hydrochloride:
Riomet ER: 500 mg/5 mL (480 mL) [contains methylparaben, propylene glycol, propylparaben]
Tablet, Oral, as hydrochloride:
Glucophage: 500 mg, 850 mg
Glucophage: 1000 mg [scored]
Generic: 500 mg, 850 mg, 1000 mg
Tablet Extended Release 24 Hour, Oral, as hydrochloride:
Fortamet: 500 mg, 1000 mg
Glucophage XR: 500 mg, 750 mg
Glumetza: 500 mg, 1000 mg
Generic: 500 mg, 750 mg, 1000 mg
Pharmacology
Mechanism of Action
Decreases hepatic glucose production, decreases intestinal absorption of glucose and improves insulin sensitivity (increases peripheral glucose uptake and utilization)
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: 654 ± 358 L; partitions into erythrocytes; concentrates in liver, kidney, and GI tract
Metabolism
Not metabolized by the liver
Excretion
Urine (90% as unchanged drug; active secretion)
Onset of Action
Within days; maximum effects up to 2 weeks
Time to Peak
Serum: Immediate release: 2 to 3 hours; ER tablet: 7 hours (range: 4 to 8 hours); ER suspension: 4.5 hours (range: 3.5 to 6.5 hours).
Half-Life Elimination
Plasma: 4 to 9 hours; Blood ~17.6 hours
Protein Binding
Negligible
Use in Specific Populations
Special Populations: Renal Function Impairment
Peak and systemic exposure is increased, and oral and renal Cl is decreased.
Special Populations: Elderly
Total plasma Cl is decreased, half-life is prolonged, and Cmax is increased.
Use: Labeled Indications
Diabetes mellitus, type 2: Management of type 2 diabetes mellitus when hyperglycemia cannot be managed with diet and exercise alone.
Note: If not contraindicated and if tolerated, metformin is the preferred initial pharmacologic agent for type 2 diabetes management (ADA 2019).
Use: Off Label
Antipsychotic-induced weight gainbyes
Data from multiple meta-analyses of randomized controlled trials with varying degrees of heterogeneity (primarily in patients with schizophrenia and schizoaffective disorder) support the use of metformin in promoting modest weight loss and preventing weight gain associated with second-generation antipsychotics in adult patients de Silva 2016, Mizuno 2014, Zheng 2015. Additional trials may be necessary to further define the role of metformin in this condition.
Based on British Association for Psychopharmacology guidelines on the management of weight gain, metabolic disturbances, and cardiovascular risk associated with psychosis and antipsychotic drug treatment, metformin should be considered to attenuate or reduce weight gain caused by antipsychotics after behavioral interventions have failed
Diabetes mellitus, type 2 (prevention)ayes
Data from a multicenter, placebo-controlled clinical trial involving 3,234 nondiabetic patients at high risk for developing diabetes showed that metformin treatment reduced the incidence of diabetes compared to placebo Knowler 2002.
Based on the American Diabetic Association (ADA) Standards of Medical Care in Diabetes, metformin is effective and may be considered for the prevention of type 2 diabetes in patients with prediabetes (ie, impaired glucose tolerance [IGT], impaired fasting glucose [IFG], or an HbA1c 5.7% to 6.4%), especially for those with BMI ≥35 kg/m2, those <60 years of age, and women with prior gestational diabetes mellitus.
Based on the Endocrine Society guidelines for the diagnosis and treatment of polycystic ovary syndrome (PCOS), metformin is recommended for prevention of type 2 diabetes in women with PCOS and IGT when lifestyle modification has not been successful Legro 2013.
Gestational diabetes mellitus (GDM) (treatment)yes
Based on the American Diabetic Association (ADA) Standards of Medical Care in Diabetes, metformin may be considered an option in the treatment of gestational diabetes mellitus based on short-term safety and efficacy studies. However, because long-term safety data are not available, insulin is the preferred treatment when pharmacologic therapy is needed.
Polycystic ovary syndrome (PCOS): Oligomenorrhea due to PCOS (treatment)byes
Data from controlled trials and meta-analyses indicate that metformin may improve menstrual patterns in some women with PCOS, but metformin is less effective than combination oral contraceptives. It is unknown whether the improvement in ovulation rate from metformin is associated with a risk reduction for endometrial carcinoma. Additional trials may be necessary to further define the role of metformin in this condition.
Endocrine Society clinical guidelines on PCOS consider metformin a second-line therapy for menstrual irregularities in women who cannot take or tolerate hormonal contraception.
Polycystic ovary syndrome: Ovarian hyperstimulation syndrome (OHSS) in women with PCOS due to in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI) (prevention)byes
Controlled trials and meta-analyses indicate that metformin significantly reduces the risk of ovarian hyperstimulation syndrome (OHSS) in women with polycystic ovary syndrome (PCOS) receiving a gonadotropin during IVF. The number needed to treat for metformin to prevent one case of OHSS is 5. Additional trials may be necessary to further define the role of metformin in this condition.
Endocrine Society guidelines for management of PCOS suggest using metformin as adjuvant therapy to prevent OHSS in women with PCOS undergoing IVF.
Contraindications
US labeling: Hypersensitivity to metformin or any component of the formulation; severe renal dysfunction (eGFR <30 mL/minute/1.73 m2); acute or chronic metabolic acidosis with or without coma (including diabetic ketoacidosis)
Canadian labeling: Hypersensitivity to metformin or any component of the formulation; renal function unknown, renal impairment, and serum creatinine levels above the upper limit of normal range; renal disease or renal dysfunction (serum creatinine ≥136 micromol/L in males or ≥124 micromol/L in females or abnormal creatinine clearance <60 mL/minute) which may result from conditions such as cardiovascular collapse (shock), acute myocardial infarction, and septicemia; unstable and/or insulin-dependent (type I) diabetes mellitus; acute or chronic metabolic acidosis, including diabetic ketoacidosis, with or without coma, history of ketoacidosis with or without coma; history of lactic acidosis (regardless of precipitating factors); excessive alcohol intake (acute or chronic); severe hepatic dysfunction or clinical or laboratory evidence of hepatic disease; cardiovascular collapse and disease states associated with hypoxemia including cardiorespiratory insufficiency, which are often associated with hyperlactacidemia; stress conditions (eg, severe infection, trauma, surgery and postoperative recovery phase); severe dehydration; pregnancy; breastfeeding
Dosage and Administration
Dosing: Adult
Antipsychotic-induced weight gain, treatment (off-label use):
Immediate release: Oral: Dosage range studied in trials: 750 mg to 2 g daily in 2 to 3 divided doses. Doses up to 2.55 g/day have also been used. To minimize GI adverse effects, most trials initiated therapy with 250 mg or 500 mg twice daily or 850 mg once daily, and increased the dose gradually based on tolerability (Baptista 2007; Chen 2013; Das 2012; de Silva 2016; Jarskog 2013; Wang 2012; Zheng 2015).
Extended release: Oral: Maintenance dosage range in trials: 1 to 2 g once daily. To minimize GI adverse effects, trials initiated therapy with 500 mg once daily and titrated dosage upwards in 500 mg increments every 2 to 6 weeks based on tolerability (Carrizo 2009; Rado 2016).
Diabetes mellitus, type 2, prevention (off-label use):
Note: For select patients with prediabetes, particularly for those with BMI ≥35 kg/m2, age <60 years, and women with prior gestational diabetes mellitus, in whom lifestyle interventions fail to improve glycemic indices (ADA 2019; McCulloch 2018a).
Immediate release: Oral: Initial: 850 mg once daily for 1 month, then increase to 850 mg twice daily; unless GI adverse effects warrant a longer titration period (Knowler 2002)
Diabetes mellitus, type 2, treatment:
Note: For patients who are not meeting glycemic targets despite diet, exercise, and metformin, combination therapy is necessary to achieve optimal results (McCulloch 2018b).
Immediate release: Oral:
Initial: 500 mg once or twice daily or 850 mg once daily (Nathan 2009)
Dosage adjustments: The dose should be increased gradually to minimize GI adverse effects. Titration strategies vary widely, but usually done in 500 mg or 850 mg increments every 7 days (range: 5 days to 1 month).
Usual maintenance dosage: 1 g twice daily or 850 mg twice daily (Nathan 2009)
Maximum: 2.55 g/day. Modest additional benefit has been observed with doses up to ~2.5 g/day; however, GI adverse effects may limit use (Nathan 2009). If doses >2 g/day are needed, consider administering in 3 divided doses to minimize GI adverse effects.
Extended release: Oral:
Initial: 500 mg to 1 g once daily
Dosage adjustments: The dose should be increased gradually to minimize GI adverse effects. Titration strategies vary widely, but usually done in 500 mg increments every 7 days (range: 7 days to 6 weeks).
Maximum: 2 g/day. If glycemic control is not achieved at maximum dose given once daily, may divide maximum dose and administer twice daily.
Gestational diabetes mellitus, treatment (alternative agent) (off-label use): Immediate release: Oral: Initial: 500 mg once or twice daily; increase dosage to meet glycemic targets, typically over 1 to 2 weeks, up to a maximum of 2 to 2.5 g daily in 2 to 3 divided doses. If targets not achieved with metformin alone, insulin may be added (Nachum 2017; Niromanesh 2012; Rowan 2008; Tertti 2013). Note: Insulin is the preferred medication for gestational diabetes as it does not cross the placenta to a measurable extent; all oral agents lack long-term safety data (ADA 2019).
Polycystic ovary syndrome (PCOS): Note: Metformin is no longer recommended for anovulatory infertility in women with PCOS (ASRM 2017).
Oligomenorrhea due to PCOS, treatment (alternative agent) (off-label use): Immediate release: Oral: Dosage range studied in trials: 1.5 to 2 g daily in 2 to 3 divided doses; to minimize GI adverse effects, most trials initiated therapy with 500 mg once or twice daily and gradually increased the dose in 500 mg increments every 7 days (Costello 2007; Moghetti 2000; Morin-Papunen 2003; Nestler 2002). Note: Cyclic progestin therapy may be added for the first 6 months of metformin treatment, until regular cycles are established (Barbieri 2018).
Ovarian hyperstimulation syndrome (OHSS) in women with PCOS due to in vitro fertilization (IVF)/intracytoplasmic sperm injection (ICSI), prevention (alternative agent) (off-label use): Immediate release: Oral: Dosage range studied in trials: 1 to 2.55 g daily in 2 to 3 divided doses (Doldi 2006; Palomba 2011; Palomba 2013; Tang 2006; Tso 2014). Note: In most trials, metformin was used as a pretreatment and coadministered with gonadotropins; one trial coadministered metformin with gonadotropins only. Metformin was given until oocyte retrieval, hCG administration, or embryo transfer in most trials; in some trials, it was given until pregnancy test or 12 weeks' gestation (Palomba 2013).
Metformin conversion recommendations:
Conversion from IR to ER dosage forms: Patients receiving metformin immediate-release may be switched to metformin extended-release once daily at the same total daily dose, up to 2 g once daily. However, in patients who are doing well with immediate-release metformin, some experts recommend they continue using it, as there is little additional benefit documented with ER tablets (Wexler 2019).
Dosing: Geriatric
Refer to adult dosing. The initial and maintenance dosing should be conservative, due to the potential for decreased renal function (monitor).
Dosing: Pediatric
Diabetes mellitus, type 2; treatment: Note: Allow 1 to 2 weeks between dose titrations. Generally, clinically significant responses are not seen at doses less than 1,500 to 2,000 mg/day (AAP [Copeland 2013]); however, a lower recommended starting dose with a gradual increase in dosage is recommended to minimize gastrointestinal symptoms.
Immediate-release tablet or solution: Children ≥10 years and Adolescents: Oral: Initial: 500 to 1,000 mg once daily or 500 mg twice daily; increase dose every 1 to 2 weeks as tolerated in 500 to 1,000 mg increments; maximum dose: 1,000 mg twice daily or 850 mg 3 times daily (AAP [Copeland 2013]; ADA [Arslanian 2018]; ISPAD [Zeitler 2018]; manufacturer labeling)
Extended-release tablets: Note: Fewer gastrointestinal effects may be seen with extended-release products; however, no pediatric studies have compared extended-release products to standard metformin (ADA [Arslanian 2018]).
Children ≥10 years and Adolescents: Limited data available: Oral: Initial: 500 to 1,000 mg once daily for 7 to 14 days; may increase dose in 500 to 1,000 mg increments every 1 to 2 weeks as tolerated; maximum daily dose: 2,000 mg/day (AAP [Copeland 2013]; ADA [Arslanian 2018]; ISPAD [Zeitler 2018]). Note: If glycemic control is not achieved at maximum dose, may divide dose and administer twice daily.
Obesity: Severe, adjunct therapy with lifestyle interventions: Limited data available; data has shown modest efficacy (BMI reduction ~3%); optimal treatment duration not established; most trials 6 to 12 months in duration with largest BMI change usually observed in the first 3 to 4 months of therapy; a daily multivitamin supplement may be considered with therapy (AHA [Kelly 2013]; Matson 2012; McDonagh 2014):
Immediate release: Dosing regimens variable: Children ≥6 years and Adolescents: Oral: Initial: 500 mg once or twice daily, titrate upward at weekly intervals by 500 mg/day increments to a target dose of 1,000 mg administered in the morning and 500 mg in the evening or 1,000 mg twice daily (Kendall 2013; Yanovski 2011); several other trials have reported doses of 500 mg twice daily dosing (Matson 2012)
Extended release: Metformin XR: Adolescents: Oral: Initial: 500 mg once daily with dinner for 2 weeks; increase to 1,000 mg once daily for 2 weeks, and then 2,000 mg once daily; may slow titration if adverse gastrointestinal effects; treatment continued for a total of 48 weeks (Glaser Pediatric Research Network [Wilson 2010])
Reconstitution
Oral suspension (extended release): Reconstitute with accompanying diluent; shake continuously for ≥2 minutes.
Administration
Oral: Administer with a meal (to decrease GI upset). Administer Riomet solution and suspension with supplied dosing cup.
ER tablets: Swallow whole; do not crush, cut, or chew. Administer once-daily doses with the evening meal.
Dietary Considerations
Drug may cause GI upset; take with food (to decrease GI upset). Take at the same time(s) each day. Dietary modification based on ADA recommendations is a part of therapy. Monitor for signs and symptoms of vitamin B12 and/or folic acid deficiency; supplementation may be required.
Storage
Oral solution (immediate release): Store at 15°C to 30°C (59°F to 86°F).
Oral suspension (extended release): Store at 20°C to 25°C (68°F to 77°F); excursion permitted to 15°C to 30°C (59°F to 86°F). Discard unused portion of reconstituted suspension after 100 days.
Tablets: Store at 20°C to 25°C (68°F to 77°F); excursion permitted to 15°C to 30°C (59°F to 86°F). Protect from light and moisture.
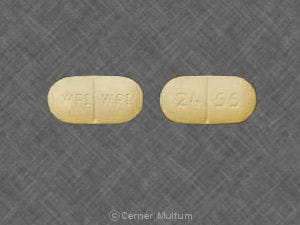
MetFORMIN Images
Drug Interactions
Abemaciclib: May increase the serum concentration of MetFORMIN. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of MetFORMIN. Specifically, alcohol may potentiate the risk of lactic acidosis Avoid combination
Alpha-Lipoic Acid: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Androgens: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Exceptions: Danazol. Monitor therapy
Bictegravir: May increase the serum concentration of MetFORMIN. Monitor therapy
Carbonic Anhydrase Inhibitors: May enhance the adverse/toxic effect of MetFORMIN. Specifically, the risk of developing lactic acidosis may be increased. Exceptions: Brinzolamide; Dorzolamide. Monitor therapy
Cephalexin: May increase the serum concentration of MetFORMIN. Monitor therapy
Cimetidine: May increase the serum concentration of MetFORMIN. Management: Consider alternatives to cimetidine in patients receiving metformin due to a potential for increased metformin concentrations and toxicity (including lactic acidosis). Consider therapy modification
Dalfampridine: MetFORMIN may increase the serum concentration of Dalfampridine. Dalfampridine may increase the serum concentration of MetFORMIN. Monitor therapy
Direct Acting Antiviral Agents (HCV): May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Dofetilide: MetFORMIN may increase the serum concentration of Dofetilide. Monitor therapy
Dolutegravir: May increase the serum concentration of MetFORMIN. Management: Consider the risks and benefits of this combination. If combined, limit the daily metformin dose to 1,000 mg when used with dolutegravir. Monitor for increased metformin effects/toxicities (including lactic acidosis) during concomitant use. Consider therapy modification
Erdafitinib: May increase the serum concentration of OCT2 Substrates. Monitor therapy
Glycopyrrolate (Systemic): May increase the serum concentration of MetFORMIN. Monitor therapy
Guanethidine: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Hyperglycemia-Associated Agents: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Hypoglycemia-Associated Agents: Antidiabetic Agents may enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Iodinated Contrast Agents: May enhance the adverse/toxic effect of MetFORMIN. Renal dysfunction that may be caused by iodinated contrast agents may lead to metformin-associated lactic acidosis. Management: Management advice varies. Refer to the full drug interaction monograph content for details. Exceptions: Diatrizoate Meglumine; Diatrizoate Sodium; Ethiodized Oil. Consider therapy modification
Isavuconazonium Sulfate: May increase the serum concentration of MetFORMIN. Monitor therapy
LamoTRIgine: May increase the serum concentration of MetFORMIN. Management: The lamotrigine Canadian product monograph states that coadministration of these drugs is not recommended. Monitor therapy
Maitake: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May enhance the adverse/toxic effect of MetFORMIN. Monitor therapy
Ombitasvir, Paritaprevir, and Ritonavir: May enhance the adverse/toxic effect of MetFORMIN. Specifically, the risk for lactic acidosis may be increased. Monitor therapy
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: May enhance the adverse/toxic effect of MetFORMIN. Specifically, the risk for lactic acidosis may be increased. Monitor therapy
Ondansetron: May increase the serum concentration of MetFORMIN. Monitor therapy
Patiromer: May decrease the serum concentration of MetFORMIN. Management: Administer metformin at least 3 hours before or 3 hours after patiromer. Consider therapy modification
Pegvisomant: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Prothionamide: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Quinolones: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
Ranolazine: May increase the serum concentration of MetFORMIN. Management: Limit the metformin dose to a maximum of 1,700 mg per day when used together with ranolazine 1,000 mg twice daily. Monitor patients for metformin toxicities, including lactic acidosis and carefully weigh the risks and benefits of this combination. Consider therapy modification
Ritodrine: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Salicylates: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Tafenoquine: May increase the serum concentration of MATE1 Substrates. Management: Avoid use of MATE substrates with tafenoquine, and if the combination cannot be avoided, monitor closely for evidence of toxicity of the MATE substrate and consider a reduced dose of the MATE substrate according to that substrate's labeling. Consider therapy modification
Tafenoquine: May increase the serum concentration of OCT2 Substrates. Management: Avoid use of OCT2 substrates with tafenoquine, and if the combination cannot be avoided, monitor closely for evidence of toxicity of the OCT2 substrate and consider a reduced dose of the OCT2 substrate according to that substrate's labeling. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Topiramate: May enhance the adverse/toxic effect of MetFORMIN. Monitor therapy
Trimethoprim: May increase the serum concentration of MetFORMIN. Monitor therapy
Trospium: MetFORMIN may decrease the serum concentration of Trospium. Monitor therapy
Vandetanib: May increase the serum concentration of MetFORMIN. Monitor therapy
Verapamil: May diminish the therapeutic effect of MetFORMIN. Monitor therapy
Adverse Reactions
>10%:
Gastrointestinal: Diarrhea (IR tablet: 12% to 53%; ER tablet: 10% to 17%), nausea and vomiting (IR tablet: 26%; ER tablet: 7%), flatulence (4% to 12%)
Infection: Infection (21%)
1% to 10%:
Cardiovascular: Chest discomfort, flushing, palpitations
Central nervous system: Headache (5% to 6%), chills, dizziness, taste disorder
Dermatologic: Diaphoresis, nail disease, skin rash
Endocrine & metabolic: Decreased vitamin B12 serum concentrate (7%), hypoglycemia
Gastrointestinal: Nausea (7% to 9%), dyspepsia (≤7%), abdominal distress (6%), abdominal pain (3% to 4%), abdominal distention, abnormal stools, constipation, heartburn
Neuromuscular & skeletal: Weakness (9%), myalgia
Respiratory: Rhinitis (4% to 6%), dyspnea, flu-like symptoms, upper respiratory tract infection
Miscellaneous: Accidental injury (6% to 7%)
<1%, postmarketing and/or case reports: Hepatic injury (cholestatic, hepatocellular, and mixed), lactic acidosis
Warnings/Precautions
Concerns related to adverse effects:
- Lactic acidosis: [US Boxed Warning]: Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. The onset is often subtle, accompanied by nonspecific symptoms (eg, malaise, myalgias, respiratory distress, somnolence, abdominal pain); elevated blood lactate levels (>5 mmol/L); anion gap acidosis (without evidence of ketonuria or ketonemia); increased lactate:pyruvate ratio; metformin plasma levels generally >5 mcg/mL. Risk factors for lactic acidosis include patients with renal impairment, concomitant use of certain drugs (eg, carbonic anhydrase inhibitors such as topiramate), ≥65 years of age, having a radiologic study with contrast, surgery and other procedures, hypoxic states (eg, acute heart failure), excessive alcohol intake, and hepatic impairment. Discontinue immediately if lactic acidosis is suspected; prompt hemodialysis is recommended. Lactic acidosis should be suspected in any patient with diabetes receiving metformin with evidence of acidosis but without evidence of ketoacidosis. Discontinue use in patients with conditions associated with dehydration, hypoperfusion, sepsis, or hypoxemia. Temporarily discontinue therapy in patients with restricted food and fluid intake. The risk of accumulation and lactic acidosis increases with the degree of impairment of renal function.
- Vitamin B12 concentrations: Long-term metformin use is associated with vitamin B12 deficiency; monitor vitamin B12 serum concentrations periodically with long-term therapy. Monitoring of B12 serum concentrations should be considered in all patients receiving metformin and in particular those with peripheral neuropathy or anemia (ADA 2019).
Disease-related concerns:
- Bariatric surgery: Altered absorption: Use IR tablets or solution after surgery. ER tablets (Glucophage XR [hydrophilic polymer matrix], Fortamet [osmotic technology], Glumetza [gastric-retentive technology]) may have a reduced effect after gastric bypass or sleeve gastrectomy due to the direct bypass of the stomach and proximal small bowel with gastric bypass or a more rapid gastric emptying and proximal small bowel transit with sleeve gastrectomy (Mechanick 2013; Melissas 2013). After gastric bypass (Roux-en-Y gastric bypass [RYGB]), administration of IR tablets led to increased absorption (AUC0-∞ increased by 21%) and bioavailability (increased by 50%) (Padwal 2011). Lactate levels decrease after gastric bypass (RYGB)-induced weight loss irrespective of the use of metformin. Routinely lowering metformin dose after gastric bypass is not necessary as long as normal renal function is preserved (Deden 2018).
- Heart failure: Metformin may be used in patients with stable heart failure (HF); avoid use in unstable or hospitalized patients with heart failure (ADA 2019). Risk of lactic acidosis may be increased secondary to hypoperfusion. In a scientific statement from the American Heart Association, metformin has been determined to be an agent that may exacerbate underlying myocardial dysfunction (magnitude: major) (AHA [Page 2016]). Use of metformin in patients with HF may be associated with reduced mortality and reduction in hospital readmission for HF (Crowley 2017; Eurich 2013).
- Hepatic impairment: The manufacturer recommends to generally avoid use in patients with hepatic impairment due to potential for lactic acidosis. However, continued use of metformin in patients with diabetes with liver dysfunction, including cirrhosis, may be associated with a survival benefit in carefully selected patients (Brackett 2010; Crowley 2017; Zhang 2014).
- Renal impairment: Metformin is substantially excreted by the kidney; assess renal function prior to initiation of therapy and periodically thereafter using eGFR; the risk of metformin accumulation and lactic acidosis increases with degree of renal impairment. Use is contraindicated in patients with eGFR <30 mL/minute/1.73 m2. Assess benefits/risks of metformin use in patients with eGFR 30 to 45 mL/minute/1.73 m2; if used, dosage reduction is recommended (ADA [Lipska 2011]; Inzucchi 2014; Wexler 2019). Some experts recommend avoiding initiation of metformin in these patients (AACE [Garber 2019]; ADA 2019; Inzucchi 2014), while others suggest initiation may be reasonable in the absence of active kidney disease and/or conditions that predispose to hypoperfusion and hypoxemia (Wexler 2019). Use of concomitant medications that may affect renal function (ie, affect tubular secretion) may also affect metformin disposition. Metformin should be withheld in patients with dehydration and/or prerenal azotemia.
- Stress-related states: It may be necessary to discontinue metformin and administer insulin if the patient is exposed to stress (fever, trauma, infection, surgery).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution; risk of metformin associated lactic acidosis increases with age.
Dosage form specific issues:
- ER tablet: Insoluble tablet shell (Glumetza 1,000 mg tablet) may remain intact and be visible in the stool. Other ER tablets (Fortamet, Glucophage XR, Glumetza 500 mg) may appear in the stool as a soft mass resembling the tablet.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP 1997; Zar 2007). See manufacturer's labeling.
Other warnings/precautions:
• Appropriate use: Not indicated for use in patients with type 1 diabetes mellitus or with diabetic ketoacidosis (DKA).
- Ethanol use: Instruct patients to avoid excessive acute or chronic ethanol use; ethanol may potentiate metformin's effect on lactate metabolism.
- Iodinated contrast: According to the manufacturer, it is recommended to temporarily discontinue metformin at the time of or before iodinated contrast imaging procedures in patients with an eGFR 30 to 60 mL/minute/1.73 m2; or with a history of hepatic disease, alcoholism, or heart failure; or in patients who will receive intra-arterial iodinated contrast. Reevaluate eGFR 48 hours after imaging procedure; restart if renal function is stable. Alternatively, the American College of Radiology (ACR) guidelines recommend that metformin may be used prior to or following administration of iodinated contrast media in patients with no evidence of acute kidney injury (AKI) and with an eGFR ≥30 mL/minute/1.73 m2; ACR guidelines recommend temporary discontinuation of metformin in patients with known AKI or severe chronic kidney disease ([stage IV or V [ie, eGFR <30 mL/minute/1.73 m2]) or who are undergoing arterial catheter studies (ACR 2017).
- Patient education: Diabetes self-management education is essential to maximize the effectiveness of therapy.
- Surgical procedures: Metformin should be withheld the day of surgery (all other oral hypoglycemic agents should be withheld the morning of surgery or procedure) (ADA 2019). Restart only after normal oral intake resumed and normal renal function is verified.
Monitoring Parameters
Urine for glucose and ketones, fasting blood glucose, hemoglobin A1c (at least twice yearly in patients who have stable glycemic control and are meeting treatment goals; quarterly in patients not meeting treatment goals or with therapy change [ADA 2019]). Initial and annual monitoring of hematologic parameters (eg, hemoglobin/hematocrit and red blood cell indices); renal function (eGFR) prior to therapy initiation and at least annually (more often in patients at risk of developing renal impairment; every 3 to 6 months if eGFR 45 to <60 mL/minute/1.73 m2; every 3 months if eGFR 30 to <45 mL/minute/1.73 m2 [Lipska 2011]). Monitor vitamin B12 serum concentrations every 2 to 3 years; folate (if megaloblastic anemia is suspected).
Pregnancy
Pregnancy Considerations
Metformin crosses the placenta; concentrations may be comparable to those found in the maternal plasma (Charles 2006; de Oliveira Baraldi 2011; Eyal 2010; Vanky 2005).
An increased risk of birth defects or adverse fetal/neonatal outcomes has not been observed following maternal use of metformin for gestational diabetes mellitus or type 2 diabetes mellitus when glycemic control is maintained (Balani 2009; Coetzee 1979; Coetzee 1984; Ekpebegh 2007; Niromanesh 2012; Rowan 2008; Rowan 2010; Tertti 2008). However, available guidelines note that long-term safety data are not available (ACOG 190 2018; ACOG 201 2018; ADA 2020).
Poorly controlled diabetes during pregnancy can be associated with an increased risk of adverse maternal and fetal outcomes, including diabetic ketoacidosis, preeclampsia, spontaneous abortion, preterm delivery, delivery complications, major birth defects, stillbirth, and macrosomia (ACOG 201 2018). To prevent adverse outcomes, prior to conception and throughout pregnancy, maternal blood glucose and HbA1c should be kept as close to target goals as possible but without causing significant hypoglycemia (ADA 2020; Blumer 2013).
Agents other than metformin are currently recommended to treat diabetes mellitus in pregnancy (ADA 2020). However, metformin may be used as an alternative agent in some patients requiring therapy for gestational diabetes mellitus or type 2 diabetes mellitus (ACOG 190 2018; ACOG 201 2018). Pharmacokinetic studies suggest that clearance of metformin may increase during pregnancy and dosing may need adjusted in some women when used during the third trimester (Charles 2006; Eyal 2010; Gardiner 2003; Hughes 2006; Vanky 2005).
Ovulation rates may increase in some anovulatory females; contraception should be discussed for women who do not wish to conceive (ACOG 194 2018). Females with diabetes mellitus who wish to conceive should use adequate contraception until glycemic control is achieved (ADA 2020).
Patient Education
What is this drug used for?
- It is used to lower blood sugar in patients with high blood sugar (diabetes).
Frequently reported side effects of this drug
- Diarrhea
- Passing gas
- Nausea
- Vomiting
- Heartburn
- Headache
- Loss of strength and energy
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Lactic acidosis like fast breathing, fast heartbeat, abnormal heartbeat, vomiting, fatigue, shortness of breath, severe loss of strength and energy, severe dizziness, feeling cold, or muscle pain or cramps.
- Low blood sugar like dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating.
- Severe abdominal pain
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.