Boxed Warning
Tardive dyskinesia:
Metoclopramide can cause tardive dyskinesia, a serious movement disorder that is often irreversible. There is no known treatment for tardive dyskinesia. The risk of developing tardive dyskinesia increases with duration of treatment and total cumulative dose. Discontinue metoclopramide in patients who develop signs or symptoms of tardive dyskinesia. In some patients, symptoms lessen or resolve after metoclopramide is stopped. Avoid treatment with metoclopramide for longer than 12 weeks because of the increased risk of developing tardive dyskinesia with longer-term use.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Injection:
Generic: 5 mg/mL (2 mL)
Solution, Injection [preservative free]:
Generic: 5 mg/mL (2 mL)
Solution, Oral:
Generic: 5 mg/5 mL (10 mL, 473 mL); 10 mg/10 mL (10 mL)
Tablet, Oral:
Reglan: 5 mg [contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake]
Reglan: 10 mg [dye free]
Generic: 5 mg, 10 mg
Tablet Disintegrating, Oral:
Metozolv ODT: 5 mg [DSC]
Generic: 5 mg, 10 mg
Pharmacology
Mechanism of Action
Metoclopramide blocks dopamine receptors and (when given in higher doses) also blocks serotonin receptors in chemoreceptor trigger zone of the CNS; enhances the response to acetylcholine of tissue in upper GI tract causing enhanced motility and accelerated gastric emptying without stimulating gastric, biliary, or pancreatic secretions; increases lower esophageal sphincter tone
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Rapid, well absorbed
Distribution
Vd: Neonates, PMA 31 to 40 weeks: 6.94 L/kg (Kearns 1998); Infants: 4.4 L/kg; Children: 3 L/kg; Adults: ~3.5 L/kg
Excretion
Urine (~85%); feces
Onset of Action
Oral: 30 to 60 minutes; IV: 1 to 3 minutes; IM: 10 to 15 minutes
Time to Peak
Serum: Oral: Neonates, PMA 31 to 40 weeks: 2.45 hours (Kearns 1998); Infants: 2.2 hours; Adults: 1 to 2 hours
Duration of Action
Therapeutic: 1 to 2 hours, regardless of route
Half-Life Elimination
Normal renal function: Neonates, PMA 31 to 40 weeks: 5.4 hours (Kearns 1998); Infants: 4.15 hours (range: 2.23 to 10.3 hours) (Kearns 1988); Children: ~4 hours (range: 2 to 12.5 hours); half-life and clearance may be dose-dependent; Adults: 5 to 6 hours (may be dose dependent)
Protein Binding
~30%
Use in Specific Populations
Special Populations: Renal Function Impairment
AUC increased ~2-fold in patients with moderate to severe renal impairment and ~3.5 fold in patients with ESRD on dialysis.
Special Populations: Hepatic Function Impairment
Clearance was reduced by ~50% in patients with severe hepatic impairment.
Special Populations Note
CYP2D6 poor metabolizers: Elimination may be slowed.
Use: Labeled Indications
Injection:
Chemotherapy-induced nausea and vomiting, prophylaxis: Prophylaxis of nausea and vomiting associated with emetogenic cancer chemotherapy. Note: Injectable metoclopramide prior to moderate- to high-emetic-risk chemotherapy is rarely indicated due to the potential for neurologic events and availability of more efficacious alternative agents.
Gastroparesis, diabetic: Relief of symptoms associated with acute and recurrent diabetic gastric stasis.
Oral:
Gastroesophageal reflux disease (GERD), refractory: Short-term (4 to 12 weeks) treatment in adults with documented symptomatic GERD who fail to respond to conventional therapy.
Note: May use metoclopramide as an adjunctive therapy only if gastroparesis is confirmed. The American College of Gastroenterology (ACG) guidelines for the treatment of GERD recommend that diagnostic evaluation to confirm underlying gastroparesis be performed prior to considering the use of prokinetic agents (ACG [Katz 2013]). Furthermore, American Gastroenterological Association (AGA) guidelines for the treatment of GERD recommend against the use of metoclopramide as monotherapy or adjunctive therapy in patients with GERD (AGA [Kahrilas 2008]).
Gastroparesis, diabetic: Relief of symptoms associated with acute and recurrent diabetic gastroparesis in adults.
Use: Off Label
Aspiration prophylaxis in patients undergoing anesthesiabyes
Data from multiple studies of varying methodologies (including randomized, double-blind, placebo-controlled trials) support the use of metoclopramide for the prevention of aspiration in patients undergoing anesthesia Manchikanti 1982, Olsson 1982, Orr 1993, Rocke 1994, Stuart 1996. Studies have encompassed a wide variety of patient populations and surgical and procedural settings, including (but not limited to) elective and emergency surgeries, rapid sequence intubation, and scheduled or emergent cesarean deliveries. Clinical experience and case reports also suggest use may be especially beneficial in patients at high risk for aspiration (eg, patients with a full stomach, severe GERD, gastroparesis and/or pregnant patients undergoing anesthesia for electroconvulsive therapy [ECT]) Berkow 2018, Hagberg 2018, Kellner 2018, Lovas 2011, O'Reardon 2011, Rabheru 2001.
Based on the American Society of Anesthesiologists (ASA) practice guidelines for obstetric anesthesia, metoclopramide is an effective and recommended prophylactic agent for the prevention of aspiration during surgical procedures (eg, cesarean delivery, postpartum tubal ligation) in pregnant patients.
Bowel obstruction (partial), malignant inoperablecyes
Clinical experience suggests the utility of metoclopramide in the management of patients with inoperable partial malignant bowel obstruction Gupta 2013, Ripamonti 2002.
Based on the 2016 Multinational Association of Supportive Care in Cancer and European Society of Medical Oncology (MASCC/ESMO) guidelines for the prevention of chemotherapy- and radiotherapy-induced nausea and vomiting and of nausea and vomiting in advanced cancer patients, metoclopramide may be used cautiously in the management of inoperable partial malignant bowel obstruction. Do not use for complete bowel obstruction MASCC/ESMO [Roila 2016].
Chemotherapy-induced nausea and vomiting, prophylaxis of delayed emesis (high-risk regimen)b
Limited data from a randomized, double-blind trial evaluating metoclopramide, in combination with dexamethasone, for prophylaxis against cisplatin-induced delayed emesis showed similar efficacy and similar toxicity with the metoclopramide regimen compared to the comparator regimen (aprepitant in combination with dexamethasone) Roila 2015. Routine use of metoclopramide is not recommended for prevention of delayed emesis (alternative agents recommended); therefore, the significance, if any, of this trial is unknown.
Dyspepsia, functional (refractory)byes
Data from 2 double-blind, placebo-controlled trials that compared different doses and formulations of metoclopramide Banani 2008 and metoclopramide and other prokinetic agents De Loose 1979 support the efficacy of metoclopramide in the treatment of dyspepsia. However, guidelines from the American College of Gastroenterology (ACG) and the Canadian Association of Gastroenterology (CAG) on the treatment of dyspepsia recommend limiting the use of metoclopramide to patients <60 years of age with dyspepsia unresponsive to proton pump inhibitors (PPI) or Helicobacter pylori eradication therapy or to any patient (including those ≥60 years of age) with functional dyspepsia that has not responded to PPIs, H. pylori eradication therapy, or tricyclic antidepressants [ACG/CAG [Moayyedi 2017].
Gastroparesis, nondiabeticyes
Based on the ACG clinical guideline on the management of gastroparesis, metoclopramide given for treatment of gastroparesis regardless of the etiology is effective and recommended in the management of this condition.
Hiccupsb
In small controlled trials and noncontrolled evaluations, metoclopramide was effective for the treatment of hiccups; however, cases of delayed onset of efficacy and cases of only partial efficacy were reported
Medication-overuse headache or intractable migraine headache (status migrainosus)c
Data from nonblinded, nonrandomized descriptive and observational trials suggest that metoclopramide may be beneficial as an adjunctive agent when used in combination with dihydroergotamine for the treatment of medication-overuse headache or status migrainosus Ford 1997, Raskin 1986, Silberstein 1990, Silberstein 1992.
Migraine, severe acute (emergency setting)yes
Based on the American Headache Society (AHS) guidelines on management of adults with acute migraine in the emergency department and the European Federation of Neurological Societies (EFNS) guidelines on the drug treatment of migraine, use of IV metoclopramide is effective and recommended in the management of acute migraine AHS [Orr 2016], EFNS [Evers 2009]. While IV administration is preferred, the IM, oral, and subcutaneous routes may also be used EFNS [Evers 2009].
Nausea and vomiting: Advanced cancer-associatedc
Clinical experience suggests the utility of metoclopramide in the treatment of nausea and vomiting in patients with advanced cancer without an identifiable etiology Gupta 2013, in the palliative care setting Bruera 1996, Del Fabbro 2020, in patients with malignant partial bowel obstruction MASCC/ESMO [Roila 2016], Ripamonti 2002, or in patients with malignancy-associated gastroparesis Bruera 2020.
Nausea and vomiting: Pregnancy-associated, severe or refractorybyes
Data from randomized, double-blind, active-controlled studies support the use of metoclopramide in the treatment of severe nausea and vomiting of pregnancy Abas 2014, Tan 2010.
Based on the American College of Obstetricians and Gynecologists (ACOG) practice bulletin on nausea and vomiting of pregnancy, metoclopramide may be considered for adjunctive treatment of nausea and vomiting in pregnant women when symptoms persist following initial pharmacologic therapy.
Nausea and/or vomiting: Undifferentiated or due to a variety of medical conditions associated with acute self-limiting nausea/vomitingc
Limited data from a small number of randomized trials, primarily in the emergency department setting in patients presenting with undifferentiated acute nausea and/or vomiting, suggest metoclopramide's utility in this condition Barrett 2011, Egerton-Warburton 2014. However, definitive, high-quality trials supporting efficacy are lacking Furyk 2015.
Clinical experience also suggests the utility of metoclopramide in the treatment of acute nausea and/or vomiting due to a variety of medical conditions associated with acute self-limiting nausea/vomiting Longstreth 2018.
Nausea and vomiting: Vertigo-associatedc
Clinical experience suggests the utility of metoclopramide in the acute treatment of nausea and vomiting associated with vertigo Furman 2018.
Radiation therapy-induced nausea and vomiting (rescue therapy)yes
Based on the American Society of Clinical Oncology (ASCO) clinical practice guideline update for antiemetics in oncology, metoclopramide may be used as rescue therapy on an as-needed basis for the prevention of radiation therapy-induced nausea and vomiting when emetic risk is low or minimal.
Tension-type headache, acute (emergency setting)b
Data from 2 prospective, randomized, double-blind trials support the use of metoclopramide, either alone Cicek 2004 or in combination with diphenhydramine Friedman 2013, for the treatment of acute tension-type headaches in the emergency department setting.
Contraindications
Hypersensitivity (eg, laryngeal and glossal angioedema, bronchospasm) to metoclopramide or any component of the formulation; situations where stimulation of gastrointestinal (GI) motility may be dangerous, including mechanical GI obstruction, perforation, or hemorrhage (except when used prior to endoscopy for evaluation of acute upper GI bleeding [Barkun 2010]); pheochromocytoma or other catecholamine-releasing paragangliomas; seizure disorder (eg, epilepsy); history of tardive dyskinesia or dystonic reaction to metoclopramide; concomitant use with other agents likely to increase extrapyramidal reactions.
Canadian labeling: Additional contraindications (not in the US labeling): Infants <1 year of age.
Dosage and Administration
Dosing: Adult
Note: To decrease the risk of tardive dyskinesia (TD), metoclopramide should not be used continuously for ≥12 weeks. Discontinue immediately if the diagnosis of TD is made; consider the use of alternative agents. In Canada, product information limits the total daily dose to 0.5 mg/kg except when used for prophylaxis of delayed emesis associated with cisplatin chemotherapy.
Aspiration prophylaxis in patients undergoing anesthesia (off-label use):
Note: May be considered in patients at high risk for aspiration (ASA 2016; Berkow 2018; Hagberg 2018; Lovas 2011; O'Reardon 2011; Rabheru 2001):
IV: 10 mg administered over 1 to 2 minutes as a single dose ~30 to 60 minutes prior to induction of anesthesia; usually given with nonparticulate antacid(s) (eg, oral sodium citrate, citric acid) and/or an H2 receptor antagonist (ASA 2016; ASA 2017; Lovas 2011; McCammon 1986; Nixon 2018; O'Reardon 2011; Orr 1993; Rocke 1994).
Bowel obstruction (partial), malignant inoperable (off-label use):
Note: Do not use in patients with confirmed or suspected complete mechanical obstruction (Gupta 2013; MASCC/ESMO [Roila 2016]; Ripamonti 2002). Often given in combination regimen (eg, with an antisecretory agent, corticosteroid, and/or anticholinergic) (Berger 2016; Gupta 2013).
Oral, IV, SubQ: 10 mg every 4 to 6 hours (Del Fabbro 2020; Glare 2008); if insufficient relief with intermittent dosing, may switch to an IV or SubQ continuous infusion.
Continuous IV or SubQ infusion (off-label): Initial: 1.25 to 1.75 mg/hour; titrate as needed and tolerated up to 5 mg/hour (Del Fabbro 2020; Twycross 2017).
Chemotherapy-induced nausea and vomiting, prophylaxis (alternative agent):
Note: Not for routine use; may be considered in select patients (eg, patients refractory to first-line agents or patients with a history of nausea/vomiting following low-emetic-risk regimens). Other agents are safer and more effective (Hesketh 2008; Hesketh 2018).
Low-emetic-risk IV chemotherapy:
Oral: Dosing regimen based on expert opinion: 10 mg before chemotherapy or 10 mg every 6 hours as needed (Hesketh 2018).
Prophylaxis of delayed emesis (high-emetic-risk chemotherapy regimen) (alternative agent) (off-label use):
Note: Routine use is not recommended for prophylaxis of delayed emesis (alternative agents recommended); however, potential alternative to neurokinin 1 (NK1) receptor antagonist (eg, aprepitant, fosaprepitant) in patients receiving cisplatin.
Oral: 10 to 20 mg 4 times daily on postchemotherapy days 2 through 4; given in combination with dexamethasone (Roila 2015).
Dyspepsia, functional (refractory) (off-label use):
Note: For patients unresponsive to first-line therapies (eg, proton pump inhibitors, Helicobacter pylori eradication, and/or tricyclic antidepressants) (ACG/CAG [Moayyedi 2017]); some experts recommend limiting duration of metoclopramide therapy to 4 weeks (Longstreth 2018b):
Oral: 5 to 10 mg 3 to 4 times daily administered prior to meals and at bedtime (Banani 2008; De Loose 1979). A lower dose of 2 mg 3 times daily (using oral liquid formulation) may provide sufficient response (Banani 2008).
Gastroparesis, diabetic (labeled use) and nondiabetic (off-label use):
Note: For patients who have had insufficient response to appropriate initial interventions (eg, dietary therapy, discontinuing drugs that impair GI motility, improved glycemic control in diabetic gastroparesis) (ACG [Camilleri 2013]; ADA 2019). With diabetic gastroparesis, some experts suggest limiting use to severe refractory cases (ADA 2019). Initiating treatment with an oral liquid formulation is preferred and may improve absorption.
Oral (preferred), IM, IV, SubQ: 5 to 10 mg 2 to 3 times daily administered prior to meals. Titrate to the lowest effective dose; maximum: 40 mg/day in 4 divided doses (ACG [Camilleri 2013]). If parenteral administration is indicated, a maximum of 30 mg/day in 3 divided doses is suggested by some experts (Camilleri 2018). In gastroparesis associated with anorexia nervosa, a lower oral dose of 2.5 mg administered prior to each meal and at bedtime may provide sufficient symptom relief according to some experts (Mehler 2019).
Duration: In chronic therapy, limit course to ≤12 weeks. Consider a “drug holiday” or dose reduction (eg, 5 mg twice daily before the 2 main meals of the day) for ~2 weeks whenever clinically feasible or at least every 12 weeks (whichever is shorter) to evaluate efficacy and necessity of continued treatment (ACG [Camilleri 2013]; Camilleri 2018).
Hiccups (off-label use):
Note: Limited data available. Treatment generally continues for up to 5 to 10 days. May discontinue treatment the day after hiccups subside; if hiccups recur, longer treatment duration may be needed (eg, in palliative care) (Lembo 2018).
IV: 5 to 10 mg every 8 hours (Madanagopolan 1975; Middleton 1973).
Oral: 10 mg every 6 to 8 hours (Madanagopolan 1975; Middleton 1973; Wang 2014).
Medication-overuse headache (MOH) or intractable migraine headache (status migrainosus) (adjunctive agent) (off-label use): Adjunct for prevention of nausea and vomiting in patients receiving dihydroergotamine (Ford 1997; Raskin 1986):
IV: Initial: 10 mg administered immediately prior to dihydroergotamine; repeat as needed every 8 hours, either prior to each intermittent dihydroergotamine dose or during continuous IV administration of dihydroergotamine (Ford 1997; Raskin 1986; Silberstein 1990; Silberstein 1992). Doses of metoclopramide up to 20 mg have been used in patients experiencing severe nausea (Garza 2018; Silberstein 1990).
Migraine, severe acute (emergency setting) (off-label use):
Note: As monotherapy or in combination with a migraine-specific agent (eg, triptan) (AAN [Silberstein 2000]; Colman 2004). IV administration may be more efficacious (AAN [Silberstein 2000]; AHS [Orr 2016]; Kelley 2012). Premedication with diphenhydramine is suggested to prevent akathisia and other acute dystonic reactions (Kelley 2012). Avoid rapid IV administration of metoclopramide doses >10 mg.
IV (preferred), IM, Oral, SubQ: 10 mg as a single dose; for migraine with severe nausea and vomiting, some experts increase the dose to 20 mg (AHS [Orr 2016]; Bajwa 2019; EFNS [Evers 2009]).
Alternative high-dose regimen: IV: 20 mg every 30 minutes as needed for up to 4 doses in combination with IV diphenhydramine (Friedman 2005).
Nausea and/or vomiting:
Undifferentiated or due to a variety of medical conditions associated with acute self-limiting nausea/vomiting (alternative agent) (off-label use): Limited data available:
IV: 10 mg or 20 mg as a single dose (Barrett 2011; Braude 2006; Cham 2004; Egerton-Warburton 2014); avoid rapid IV administration of doses >10 mg.
Oral: 10 mg as a single dose; may repeat after 4 to 6 hours if needed.
Advanced cancer-associated (off-label use):
Note: Limited data available; dosing recommendations based primarily on expert opinion:
Empiric therapy in patients without an identifiable etiology:
Oral, IV, SubQ: 10 mg every 6 hours (Gupta 2013).
Malignancy-associated gastroparesis:
Oral, IV, SubQ: 5 to 10 mg every 6 hours or 3 to 4 times daily before meals and at night (Donthireddy 2007; Kelly 2014; Leung 2009; Shivshanker 1983); if needed and tolerated, some experts titrate up to 20 mg every 6 hours (Shafi 2018).
Palliative care setting:
Oral, IV, SubQ: Initial: 5 to 10 mg every 4 to 6 hours (Bruera 1996; Del Fabbro 2020; Glare 2011). For severe symptoms, some experts titrate up to 100 mg/day (in divided doses) if needed (Del Fabbro 2020). If insufficient relief with intermittent dosing, may switch to an IV or SubQ continuous infusion.
Continuous IV or SubQ infusion: Initial: 1.25 to 1.75 mg/hour; titrate as needed and tolerated up to 5 mg/hour (Bruera 1996; Twycross 2017).
Pregnancy-associated, severe or refractory (off-label use):
Note: May be considered as add-on or alternative therapy for nausea and vomiting when symptoms persist following initial pharmacologic therapy and IV hydration if hypovolemic (ACOG 2018).
Oral, IV, IM: 5 to 10 mg every 6 to 8 hours, added to current treatment regimen or as alternative therapy (ACOG 2018; Smith 2019); if feasible, give 30 minutes before meals and bedtime.
Vertigo-associated (alternative agent) (off-label use):
Oral, IV: 5 to 10 mg every 6 hours as needed (Furman 2018); discontinue as soon as severe symptoms resolve, usually after 1 to 2 days (Furman 2018; Swartz 2005).
Radiation therapy-induced nausea and vomiting (rescue therapy) (alternative agent) (off-label use):
Low-emetic-risk radiation therapy (head and neck, thorax, or pelvis):
Oral, IV: 5 to 20 mg if needed after each radiation treatment and repeated every 6 to 8 hours; depending on symptom severity and remaining duration of radiation therapy, patients can receive subsequent rescue therapy as needed or begin prophylactic therapy (ASCO [Hesketh 2017]).
Minimal-emetic-risk radiation therapy (extremities, breast):
Oral, IV: 5 to 20 mg if needed after each radiation treatment (ASCO [Hesketh 2017]).
Note: Avoid rapid IV administration of doses >10 mg.
Tension-type headache, acute (emergency setting) (alternative agent) (off-label use):
Note: Limited data available.
IV: 10 mg as a single dose (Cicek 2004) or 20 mg as a single dose; premedicate with IV diphenhydramine to prevent akathisia and other acute dystonic reactions (Friedman 2013). Note: Avoid rapid IV administration of metoclopramide doses >10 mg.
Dosing: Geriatric
Initial: Dose at the lower end of the recommended range (may require only 5 mg/dose) and use the lowest effective dose. Refer to adult dosing.
Dosing: Pediatric
Postpyloric feeding tube placement (short bowel intubation): IV:
Patient age:
<6 years: 0.1 mg/kg as a single dose
6 to 14 years: 2.5 to 5 mg as a single dose
>14 years: 10 mg as a single dose
Gastroesophageal reflux: Limited data available; efficacy results variable (Vandenplas, 2009): Note: NASPGHAN/ESPGHAN guidelines do not recommend metoclopramide for routine treatment of GERD; evaluate risk:benefit prior to use (Vandenplas, 2009): Infants, Children, and Adolescents: Oral: 0.1 to 0.2 mg/kg/dose every 6 to 8 hours; maximum dose: 10 mg (Chicella, 2005; Forbes, 1986; Rode, 1987; Tolia, 1989)
Postoperative nausea and vomiting; prevention: Limited data available; optimal dose not established; efficacy results variable: Note: Guidelines discourage use of metoclopramide; considered ineffective (Gan, 2007): Children and Adolescents: IV: 0.1 to 0.5 mg/kg/dose as a single dose administered after induction or on arrival to PACU; maximum dose: 10 mg/dose (Ferrari, 1992; Furst, 1994; Henzi, 1999; Lin, 1992)
Chemotherapy-induced nausea and vomiting (CINV), prevention: Limited data available; optimal dose not established; efficacy results variable. Note: Doses required to prevent CINV are high and should not be used first-line due to increased risk of extrapyramidal symptoms (acute dystonic reactions); concurrent administration of diphenhydramine or benztropine is recommended to prevent drug-induced adverse effects (Dupuis, 2013; Roila, 1998).
POGO Guidelines (Dupuis, 2013): Infants, Children and Adolescents: Note: For use in patients in whom corticosteroids are contraindicated; use in combination with 5-HT3 receptor antagonists.
Initial dose: IV: 1 mg/kg as a single dose prior to chemotherapy
Subsequent doses: Oral: 0.0375 mg/kg/dose every 6 hours
Alternate dosing: Children and Adolescents: IV: 1 to 2 mg/kg/dose prior to and then every 2 to 4 hours up to every 6 hours following chemotherapy; maximum: 5 doses/day (Roila, 1998; Terrin, 1984); another trial administered 2 mg/kg when chemotherapy was started followed by 2 mg/kg/dose 2, 6, and 12 hours later (Marshall, 1989)
Reconstitution
Injection: Lower doses (≤10 mg): No dilution required; Higher doses (>10 mg): Dilute in 50 mL of compatible solution (preferably NS).
Administration
Injection: May be given IM, direct IV push, short infusion (at least 15 minutes), or continuous infusion; lower doses (≤10 mg) of metoclopramide can be given IV push undiluted over 1 to 2 minutes; higher doses (>10 mg) to be diluted in 50 mL of compatible solution (preferably NS) and given IVPB over at least 15 minutes. Note: Rapid IV administration may be associated with a transient (but intense) feeling of anxiety and restlessness, followed by drowsiness.
Tablets and oral solution: Administer 30 minutes prior to meals and at bedtime.
Orally disintegrating tablets: Administer on an empty stomach at least 30 minutes prior to food and at bedtime (do not repeat if inadvertently taken with food). Do not remove from packaging until time of administration. If tablet breaks or crumbles while handling, discard and remove new tablet. Using dry hands, place tablet on tongue and allow to dissolve (disintegrates within ~1 minute [range: 10 seconds to 14 minutes]). Swallow with saliva (formulation is designed to be taken without liquids).
Subcutaneous administration (off-label route) has been reported, either as an intermittent bolus injection or as continuous infusion (Bruera 1996; McCallum 1991).
Storage
Injection: Store intact vials at 20°C to 25°C (68°F to 77°F); protect from light. Injection is photosensitive and should be protected from light during storage; parenteral admixtures in D5W, D51/2NS, NS, LR, or Ringer's injection are stable for up to 24 hours after preparation at normal light conditions or up to 48 hours if protected from light. When mixed with NS, can be stored frozen for up to 4 weeks; metoclopramide is degraded when admixed and frozen with D5W.
Oral solution/orally disintegrating tablet/tablet: Store at 20°C to 25°C (68°F to 77°F). Protect from light. Do not freeze oral solution. Keep orally disintegrating tablet in original packaging until just prior to use.
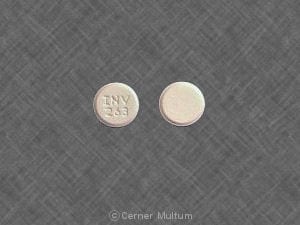
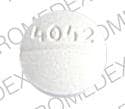
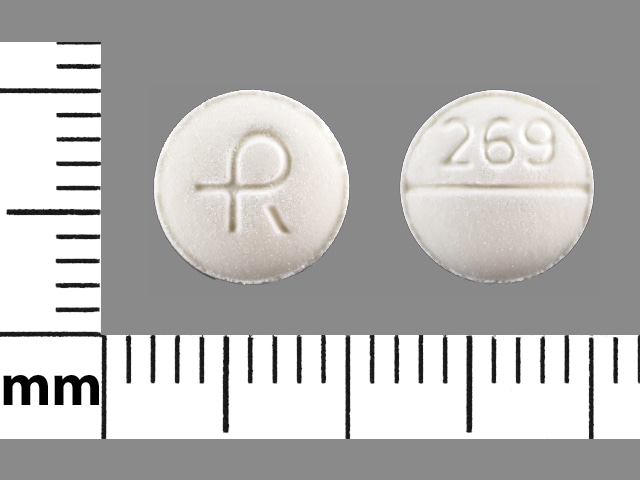
Metoclopramide Images
Drug Interactions
Anticholinergic Agents: May diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Anti-Parkinson Agents (Dopamine Agonist): Metoclopramide may diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Monitor therapy
Antipsychotic Agents: Metoclopramide may enhance the adverse/toxic effect of Antipsychotic Agents. Avoid combination
Atovaquone: Metoclopramide may decrease the serum concentration of Atovaquone. Management: Consider alternatives to metoclopramide when possible; atovaquone should only be used with metoclopramide if no other antiemetics are available. Consider therapy modification
CycloSPORINE (Systemic): Metoclopramide may increase the absorption of CycloSPORINE (Systemic). Monitor therapy
CYP2D6 Inhibitors (Strong): May increase the serum concentration of Metoclopramide. Management: Reduce metoclopramide dose to 5 mg 4 times daily (30 minutes before each meal and at bedtime) and limit the maximum daily dose to 20 mg if combined with strong CYP2D6 inhibitors. Consider therapy modification
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Deutetrabenazine: May enhance the adverse/toxic effect of Metoclopramide. Specifically, the risk for akathisia, parkinsonism, or neuroleptic malignant syndrome may be increased. Monitor therapy
Droperidol: May enhance the adverse/toxic effect of Metoclopramide. Avoid combination
Fosfomycin: Gastrointestinal Agents (Prokinetic) may decrease the serum concentration of Fosfomycin. Monitor therapy
Levosulpiride: Benzamide Derivatives may enhance the adverse/toxic effect of Levosulpiride. Monitor therapy
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
MetyroSINE: May enhance the adverse/toxic effect of Metoclopramide. Management: Seek alternatives to this combination when possible. Monitor patients receiving metoclopramide with metyrosine for development of extrapyramidal symptoms. Consider therapy modification
Monoamine Oxidase Inhibitors: Metoclopramide may enhance the hypertensive effect of Monoamine Oxidase Inhibitors. Avoid combination
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Opioid Agonists: May diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Posaconazole: Metoclopramide may decrease the serum concentration of Posaconazole. Monitor therapy
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Promethazine: Metoclopramide may enhance the adverse/toxic effect of Promethazine. Avoid combination
Quinagolide: Metoclopramide may diminish the therapeutic effect of Quinagolide. Monitor therapy
Rivastigmine: May enhance the adverse/toxic effect of Metoclopramide. Specifically, the risk of extrapyramidal adverse reactions may be increased with this combination. Avoid combination
Selective Serotonin Reuptake Inhibitors: Metoclopramide may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Management: Seek alternatives to this combination when possible. Monitor patients receiving metoclopramide with selective serotonin reuptake inhibitors for signs of extrapyramidal symptoms, neuroleptic malignant syndrome, and serotonin syndrome. Consider therapy modification
Serotonin/Norepinephrine Reuptake Inhibitors: Metoclopramide may enhance the adverse/toxic effect of Serotonin/Norepinephrine Reuptake Inhibitors. Management: Seek alternatives to this combination when possible. Monitor patients receiving metoclopramide with serotonin/norepinephrine reuptake inhibitors for signs of extrapyramidal symptoms, neuroleptic malignant syndrome, and serotonin syndrome. Consider therapy modification
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Tacrolimus (Systemic): Metoclopramide may increase the serum concentration of Tacrolimus (Systemic). Specifically, treatment of gastroparesis may increase tacrolimus concentrations. Monitor therapy
Tetrabenazine: Metoclopramide may enhance the adverse/toxic effect of Tetrabenazine. Avoid combination
Thiopental: Metoclopramide may enhance the therapeutic effect of Thiopental. Management: Consider thiopental dose reduction when used concomitantly with metoclopramide. Monitor patient response to treatment closely if using this combination. Consider therapy modification
Tricyclic Antidepressants: Metoclopramide may enhance the adverse/toxic effect of Tricyclic Antidepressants. Management: Seek alternatives to this combination when possible. Monitor patients receiving metoclopramide with tricyclic antidepressants for signs of extrapyramidal symptoms, neuroleptic malignant syndrome, and serotonin syndrome. Consider therapy modification
Trimetazidine: Metoclopramide may enhance the adverse/toxic effect of Trimetazidine. Specifically, the risk of extrapyramidal symptoms may be enhanced. Avoid combination
Adverse Reactions
Frequency not always defined.
Cardiovascular: Atrioventricular block, bradycardia, cardiac failure, flushing (following high IV doses), hypertension, hypotension, supraventricular tachycardia
Central nervous system: Drowsiness (~10% to 70%; dose related), dystonic reaction (<1% to 25%; dose and age related), lassitude (~10%), restlessness (~10%), fatigue (2% to 10%), headache (4% to 5%), dizziness (1% to 4%), somnolence (2% to 3%), akathisia, confusion, depression, drug-induced Parkinson's disease, hallucination (rare), insomnia, neuroleptic malignant syndrome (rare), seizure, suicidal ideation, tardive dyskinesia
Dermatologic: Skin rash, urticaria
Endocrine & metabolic: Amenorrhea, fluid retention, galactorrhea, gynecomastia, hyperprolactinemia, porphyria
Gastrointestinal: Nausea (4% to 6%), vomiting (1% to 2%), diarrhea
Genitourinary: Impotence, urinary frequency, urinary incontinence
Hematologic & oncologic: Agranulocytosis, leukopenia, methemoglobinemia, neutropenia, sulfhemoglobinemia
Hepatic: Hepatotoxicity (rare)
Hypersensitivity: Angioedema (rare), hypersensitivity reaction
Neuromuscular & skeletal: Laryngospasm (rare)
Ophthalmic: Visual disturbance
Respiratory: Bronchospasm, laryngeal edema (rare)
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery or driving).
- Depression: Depression has occurred (in patients with and without a history of depression); symptoms have included suicidal ideation and suicide; avoid use in patients with a history of depression.
- Extrapyramidal symptoms (EPS): May cause extrapyramidal symptoms, generally manifested as acute dystonic reactions within the initial 24 to 48 hours of use at the usual adult dose (30 to 40 mg/day). Risk of these reactions is increased at higher than recommended doses, and in patients <30 years of age. Symptoms may include involuntary limb movements, facial grimacing, torticollis, oculogyric crisis, rhythmic tongue protrusion, bulbar type speech, trismus, or dystonic reactions resembling tetanus. May also rarely present as stridor and dyspnea (may be due to laryngospasm). Dystonic symptoms may be managed with IM diphenhydramine or benztropine. Pseudoparkinsonism (eg, bradykinesia, tremor, cogwheel rigidity, mask-like facies) may also occur (usually within first 6 months of therapy but also after longer periods) and is generally reversible within 2 to 3 months following discontinuation. Motor restlessness (eg, anxiety, agitation, jitteriness, insomnia) may occur; if symptoms resolve, consider restarting at a lower dosage. Avoid metoclopramide in patients receiving other drugs that are likely to cause EPS (eg, antipsychotics).
- Hyperprolactinemia: Metoclopramide elevates prolactin levels. Hyperprolactinemia may suppress hypothalamic GnRH, resulting in reduced pituitary gonadotropin secretion. This, in turn, may inhibit reproductive function by impairing gonadal steroidogenesis. Galactorrhea, amenorrhea, gynecomastia, and impotence have been reported. Hyperprolactinemia may potentially stimulate prolactin-dependent breast cancer. However, some clinical studies and epidemiology studies have not shown an association between administration of dopamine D2 receptor antagonists and tumorigenesis in humans.
- Hypertension: May elevate blood pressure; avoid use in patients with hypertension (IV administration was shown to release catecholamines). There are reports of hypertensive crises in patients with undiagnosed pheochromocytoma; use is contraindicated in patients with pheochromocytoma or other catecholamine-releasing paragangliomas. Discontinue therapy in any patient with a rapid rise in blood pressure.
- Neuroleptic malignant syndrome: Use may be associated with neuroleptic malignant syndrome (NMS); may be fatal. Monitor for manifestations of NMS, which include hyperpyrexia, muscle rigidity, altered mental status, and autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac arrhythmias); additional signs may include elevated creatine phosphokinase, myoglobinuria, and acute renal failure. Discontinue immediately if signs/symptoms of NMS appear and begin intensive symptomatic management and monitoring.
- Proarrhythmic effects: Metoclopramide has been known to cause sinus arrest (usually with rapid IV administration or higher doses) (Bentsen 2002; Malkoff 1995). The torsadogenic potential for metoclopramide is considered to be low (Claassen 2005). Based on case reports, however, metoclopramide may cause QT prolongation and torsades de pointes in certain individuals (eg, heart failure patients with renal impairment) (Siddique 2009). There is data in healthy male volunteers to show that metoclopramide actually shortens the QT interval while at the same time increasing QT variance (Ellidokuz 2003). No human data other than case reports, however, has demonstrated a consistent QT prolonging effect with metoclopramide nor is there any substantiated evidence to show a direct association with the development of torsades de pointes.
- Tardive dyskinesia: [US Boxed Warning]: May cause tardive dyskinesia, a serious movement disorder that is often irreversible with no known treatment; the risk of developing tardive dyskinesia increases with duration of treatment and total cumulative dose. Discontinue metoclopramide in patients who develop signs/symptoms of tardive dyskinesia; in some patients, symptoms may lessen or resolve after metoclopramide is stopped. Avoid treatment with metoclopramide for longer than 12 weeks because of the increased risk of developing tardive dyskinesia with longer-term use. Avoid metoclopramide in patients receiving other drugs that are likely to cause tardive dyskinesia (eg, antipsychotics). Tardive dyskinesia is characterized by disfiguring involuntary movements of the face, tongue, and sometimes of the trunk and/or extremities; movements may be choreoathetotic in appearance. Metoclopramide may mask underlying tardive disease by suppressing or partially suppressing tardive dyskinesia signs; the effect of this symptomatic suppression upon the long-term course of tardive dyskinesia is unknown. The risk of developing tardive dyskinesia is increased in the elderly, especially elderly women, and diabetics, although it is not possible to predict which patients will develop tardive dyskinesia. Discontinue metoclopramide immediately in patients who develop signs/symptoms of tardive dyskinesia. There is no known effective treatment for established cases of tardive dyskinesia, although in some patients, tardive dyskinesia may remit (partially or completely) within several weeks to months after metoclopramide is withdrawn.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with heart failure and concomitant renal impairment; may be at risk for development of QT prolongation and torsades de pointes (Siddique 2009).
- Edematous conditions: Use with caution in patients who are at risk of fluid overload (HF, cirrhosis). Metoclopramide causes a transient increase in serum aldosterone and increases the risk for fluid retention and volume overload. Discontinue if adverse events or signs/symptoms appear.
- Hepatic impairment: Use caution in patients with moderate to severe hepatic impairment; risk of adverse reactions may be increased due to increased systemic exposure; dosage adjustment recommended.
- Nicotinamide adenine dinucleotide hydrogen (NADH)-cytochrome b5 reductase deficiency: Patients with NADH-cytochrome b5 reductase deficiency are at increased risk of methemoglobinemia and/or sulfhemoglobinemia.
- Parkinson disease: Symptoms of Parkinson disease may be exacerbated; avoid use in patients with Parkinson disease and other patients being treated with antiparkinsonian drugs.
- Renal impairment: Use with caution in patients with moderate to severe renal impairment; risk of adverse reactions may be increased due to increased systemic exposure; dosage adjustment recommended.
- Surgical anastomosis/closure: Use with caution following surgical anastomosis/closure; promotility agents may theoretically increase pressure in suture lines.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- CYP2D6 poor metabolizers: Elimination of metoclopramide may be slowed possibly increasing the risk of dystonic and other adverse reactions; dosage reduction recommended.
- Elderly: Risk of tardive dyskinesia may be increased in elderly, especially in elderly women.
- Pediatric: Not recommended for use (oral formulation) due to increased risk of tardive dyskinesia and other extrapyramidal symptoms as well as the risk of methemoglobinemia in neonates (neonates may have decreased levels of NADH-cytochrome b5 reductase, which increases the risk of methemoglobinemia).
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggest that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer's labeling.
Monitoring Parameters
Signs of tardive dyskinesias, extrapyramidal symptoms; signs/symptoms of neuroleptic malignant syndrome
Pregnancy
Pregnancy Considerations
Metoclopramide crosses the placenta and can be detected in cord blood and amniotic fluid (Arvela 1983; Bylsma-Howell 1983). Available studies do not report an increased risk of adverse pregnancy-related outcomes following maternal use. Extrapyramidal symptoms or methemoglobinemia may potentially occur in the neonate.
Metoclopramide is one of the agents that may be considered for adjunctive treatment of nausea and vomiting in pregnant women when symptoms persist following initial pharmacologic therapy. Oral or IM therapy may be given in patients who are not dehydrated; IV therapy should be used when dehydration is present (ACOG 189 2018). Metoclopramide may be used for prophylaxis of nausea and vomiting associated with cesarean delivery (ASA 2016; Smith 2011).
Patient Education
What is this drug used for?
- It is used to treat heartburn.
- It is used to treat or prevent upset stomach and throwing up.
- It is used to treat gastroesophageal reflux disease (GERD; acid reflux).
- It is used to treat a slow moving GI (gastrointestinal) tract in some people.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Diarrhea
- Fatigue
- Nausea
- Loss of strength and energy
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea.
- Tardive dyskinesia like being unable to control body movements; tongue, face, mouth, or jaw sticking out; mouth puckering; or puffing cheeks.
- Neuroleptic malignant syndrome like fever, muscle cramps or stiffness, dizziness, severe headache, confusion, change in thinking, fast heartbeat, abnormal heartbeat, or sweating a lot.
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Severe headache
- Severe dizziness
- Passing out
- Vision changes
- Tremors
- Difficulty moving
- Rigidity
- Enlarged breasts
- Nipple discharge
- Sexual dysfunction
- Menstrual changes
- Agitation
- Abnormal movements
- Twitching
- Change in balance
- Difficulty swallowing
- Difficulty speaking
- Panic attacks
- Irritability
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.