Boxed Warning
Carcinogenic:
Metronidazole has been shown to be carcinogenic in mice and rats. Unnecessary use of the drug should be avoided. Its use should be reserved for the conditions for which this drug is indicated.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Flagyl: 375 mg
Generic: 375 mg
Solution, Intravenous:
Generic: 500 mg (100 mL)
Solution, Intravenous [preservative free]:
Generic: 500 mg (100 mL); 5 mg/mL (100 mL [DSC])
Tablet, Oral:
Flagyl: 250 mg, 500 mg
Generic: 250 mg, 500 mg
Pharmacology
Mechanism of Action
After diffusing into the organism, interacts with DNA to cause a loss of helical DNA structure and strand breakage resulting in inhibition of protein synthesis and cell death in susceptible organisms
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Well absorbed
Distribution
To bile, seminal fluid, bone, liver, and liver abscesses, lung and vaginal secretions; crosses blood-brain barrier; saliva and CSF concentrations similar to those in plasma
Metabolism
Hepatic (30% to 60%) to several metabolites including an active hydroxyl metabolite which maintains activity ~30% to 65% of the parent compound (Lamp 1999)
Excretion
Urine (unchanged drug and metabolites: 60% to 80%; ~20% of total as unchanged drug); feces (6% to 15%)
Time to Peak
Serum: Oral: 1 to 2 hours
Half-Life Elimination
Neonates <7 days (Jager-Roman 1982): Within first week of life, more prolonged than with lower GA:
GA 28 to 30 weeks: 75.3 ± 16.9 hours
GA 32 to 35 weeks: 35.4 ± 1.5 hours
GA 36 to 40 weeks: 24.8 ± 1.6 hours
Neonates ≥7 days: ~22.5 hours (Upadhyaya 1988)
Children and Adolescents: 6 to 10 hours (Lamp 1999)
Adults: ~8 hours
Protein Binding
<20%
Use in Specific Populations
Special Populations: Renal Function Impairment
CrCl ≤65 mL/minute: Half-life: 18 to 32 hours (hydroxy metabolite [active]) (Lamp 1999)
Special Populations: Hepatic Function Impairment
Half-life: 18.31 hours (mean) in one study (Lau 1987)
According to Child-Pugh classification (Muscara 1995):
Child-Pugh class A: ~10.7 hours
Child-Pugh class B: ~13.5 hours
Child-Pugh class C: ~21.5 hours
Use: Labeled Indications
Amebiasis: Treatment of acute intestinal amebiasis (amebic dysentery) and extraintestinal amebiasis (liver abscess)
Limitations of use: When used for amebic liver abscess, may be used concurrently with percutaneous needle aspiration when clinically indicated.
Anaerobic bacterial infections (caused by Bacteroides spp., including the B. fragilis group):
Bacterial septicemia: Treatment of bacterial septicemia (also caused by Clostridium spp.)
Bone and joint infections: Treatment (adjunctive therapy) of bone and joint infections
CNS Infections: Treatment of CNS infections, including meningitis and brain abscess
Endocarditis: Treatment of endocarditis
Gynecologic infections: Treatment of gynecologic infections including endometritis, endomyometritis, tubo-ovarian abscess, and postsurgical vaginal cuff infection (also caused by Clostridium spp., Peptococcus spp., Peptostreptococcus spp., and Fusobacterium spp.)
Intra-abdominal infections: Treatment of intra-abdominal infections, including peritonitis, intra-abdominal abscess, and liver abscess (also caused by Clostridium spp., Eubacterium spp., Peptococcus spp., and Peptostreptococcus spp.)
Lower respiratory tract infections: Treatment of lower respiratory tract infections, including pneumonia, empyema, and lung abscess
Skin and skin structure infections: Treatment of skin and skin structure infections (also caused by Clostridium spp., Peptococcus spp., Peptostreptococcus spp., and Fusobacterium spp.)
Surgical prophylaxis (colorectal surgery): Injection: Preoperative, intraoperative, and postoperative prophylaxis to reduce the incidence of postoperative infection in patients undergoing elective colorectal surgery classified as contaminated or potentially contaminated
Trichomoniasis: Treatment of infections caused by Trichomonas vaginalis, including treatment of asymptomatic sexual partners
Use: Off Label
Balantidiasiscyes
Data from a single case report of one immunocompromised patient with pulmonary infection treated with metronidazole suggest that metronidazole may be beneficial for the treatment of balantidiasis Anagyrou 2003. Clinical experience also suggests the utility of metronidazole in the treatment of balantidiasis CDC 2013.
Bite wound infection, prophylaxis or treatment (animal or human bite)yes
Based on the Infectious Diseases Society of America (IDSA) guidelines for the diagnosis and management of skin and soft tissue infections (SSTIs), metronidazole, in combination with other appropriate agents, is an effective and recommended alternative for treatment of bite wounds.
Clostridioides (formerly Clostridium) difficile infectionyes
Based on the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA) guidelines for Clostridioides (formerly Clostridium) difficile infection, oral metronidazole is an effective and recommended alternative agent for the management of initial episodes of nonsevere (WBC ≤15,000 cells/mm3 and serum creatinine <1.5 mg/dL) C. difficile infections if access to vancomycin or fidaxomicin is limited or use is contraindicated. IV metronidazole is recommended in combination with oral and/or rectal vancomycin for fulminant C. difficile infections, particularly when ileus is present. Metronidazole should not be used for prolonged therapy because of the potential for cumulative and potentially irreversible neurotoxicity; oral metronidazole should not be used for recurrent infections.
Crohn disease, management after surgical resectionbyes
Data from a small double-blind, randomized, placebo-controlled trial support the use of metronidazole as management of Crohn disease after surgical resection; in the trial, metronidazole reduced the incidence of endoscopic recurrence and decreased early clinical recurrence rates Rutgeerts 1995. Data from 2 randomized, placebo-controlled trials and a meta-analysis suggest that metronidazole alone is of modest benefit in reduction of postoperative recurrence, whereas metronidazole combined with a thiopurine (eg, azathioprine, mercaptopurine) or anti-tumor necrosis factor (anti-TNF) (eg, adalimumab) is moderately effective in reducing recurrence rates De Cruz 2015, D’Haens 2008, Peyrin-Biroulet 2009.
Based on the American Gastroenterological Association Institute guidelines for the management of Crohn disease after surgical resection, metronidazole is a suggested second-line alternative for patients who are concerned about the adverse effects of first-line therapy (eg, anti-TNFs, thiopurines) and who have a lower risk of recurrence. The American College of Gastroenterology Clinical guideline for the management of Crohn disease in adults also suggests that metronidazole may be used following small intestine resection in patients with Crohn disease to prevent recurrence ACG [Lichtenstein 2018].
Crohn disease, treatment of simple perianal fistulasyes
Based on the American College of Gastroenterology guidelines for the management of Crohn disease in adults, metronidazole (with or without ciprofloxacin) is an effective and recommended treatment for patients with simple perianal fistulas ACG [Lichtenstein 2018].
Dientamoeba fragilis infectionyes
Based on the Centers for Disease Control and Prevention (CDC) resources for health professionals, metronidazole is an effective and recommended agent for the treatment of D. fragilis.
Giardiasisayes
In a meta-analysis of trials evaluating the treatment of giardiasis, the use of metronidazole was found to be of similar effectiveness to albendazole for the treatment of giardiasis, although metronidazole may have slightly more adverse effects Granados 2012.
Helicobacter pylori eradicationyes
Based on the American College of Gastroenterology guideline on the treatment of Helicobacter pylori infection, metronidazole is an effective and recommended component of a multiple-drug regimen for the treatment of H. pylori infection.
Periodontitis, severeb
Data from a small randomized, 12-month, double-blind, placebo-controlled trial (N=35) evaluating the use of either amoxicillin and metronidazole or placebo in conjunction with aggressive dental care demonstrated that amoxicillin (in combination with metronidazole) significantly improved dental parameters and increased beneficial bacteria Silva-Senem 2013. In addition, clinical experience suggests the utility of metronidazole (with amoxicillin) for the treatment of severe periodontitis Wilder 2019.
Pouchitis (post ileal pouch-anal anastomosis)a
In a systematic review of available clinical trials evaluating the treatment and prevention of pouchitis after ileal pouch-anal anastomosis for chronic ulcerative colitis, metronidazole was found to be less effective than ciprofloxacin but as effective as budesonide enemas for inducing remission in acute pouchitis. Metronidazole is considered an effective alternative treatment for this condition Holubar 2010.
Data from a noncomparative cohort study suggest that metronidazole, in combination with ciprofloxacin, may be beneficial for the treatment of patients with chronic pouchitis Mimura 2002.
Surgical prophylaxis, colorectal surgery (oral metronidazole)yes
Based on the American Society of Health-System Pharmacists, IDSA, Surgical Infection Society, and SHEA guidelines for antimicrobial prophylaxis in surgery, oral metronidazole, in combination with additional oral antibiotics and in conjunction with mechanical bowel preparation, is effective and recommended for colorectal surgery prophylaxis Bratzler 2013.
Surgical prophylaxis, uterine evacuation (induced abortion or pregnancy loss)yes
Based on the American College of Obstetricians and Gynecologists guidelines for prevention of infection after gynecologic procedures, metronidazole is effective and recommended as an alternative agent for antimicrobial prophylaxis for uterine evacuation procedures in case of induced abortion or pregnancy loss.
Tetanusbyes
Data from an open-label clinical trial in patients with moderate tetanus treated with either metronidazole or intramuscular procaine penicillin suggest that metronidazole may be beneficial and possibly superior to the use of penicillin for the treatment of this condition Ahmadsyah 1985.
Contraindications
Hypersensitivity to metronidazole, nitroimidazole derivatives, or any component of the formulation; pregnant patients (first trimester) with trichomoniasis; use of disulfiram within the past 2 weeks; use of alcohol or propylene glycol-containing products during therapy or within 3 days of therapy discontinuation
Canadian labeling: Additional contraindications (not in the US labeling): Active neurological disorders; history of blood dyscrasia; hypothyroidism; hypoadrenalism
Dosage and Administration
Dosing: Adult
Amebiasis, intestinal (acute dysentery) or extraintestinal (liver abscess): Oral: 500 to 750 mg every 8 hours for 7 to 10 days followed by an intraluminal agent (eg, paromomycin) (Drugs for Parasitic Infections 2013; Leder 2018a; Leder 2018b).
Bacterial vaginosis: Oral: 500 mg twice daily for 7 days (CDC [Workowski 2015]; SOGC [Yudin 2017]).
Balantidiasis (alternative agent) (off-label use): Oral: 750 mg 3 times daily for 5 days (CDC 2013; Drugs for Parasitic Infections 2013; Weller 2018).
Bite wound infection, prophylaxis or treatment, animal or human bite (alternative agent) (off-label use): Oral, IV: 500 mg every 8 hours (Baddour 2019a; Baddour 2019b; IDSA [Stevens 2014]). Duration is 3 to 5 days for prophylaxis; duration of treatment for established infection is typically 5 to 14 days and varies based on clinical response and patient-specific factors (Baddour 2019a; Baddour 2019b). Note: For animal bites, use in combination with an appropriate agent for Pasteurella multocida. For human bites, use in combination with an appropriate agent for Eikenella corrodens (IDSA [Stevens 2014]).
Clostridioides (formerly Clostridium) difficile infection (off-label use): Note: Criteria for disease severity is based on expert opinion and should not replace clinical judgment (IDSA/SHEA [McDonald 2018]).
Nonsevere (supportive clinical data: WBC ≤15,000 cells/mm3 and serum creatinine <1.5 mg/dL), initial episode (alternative agent if oral vancomycin or fidaxomicin unavailable or contraindicated): Oral: 500 mg 3 times daily for 10 days. Note: Treatment duration may be extended to 14 days if patient has improved but has not had symptom resolution (IDSA/SHEA [McDonald 2018]).
Fulminant infection (supportive clinical data: ileus, megacolon, and/or hypotension/shock): IV: 500 mg every 8 hours in combination with oral and/or rectal vancomycin (IDSA/SHEA [McDonald 2018]; Surawicz 2013).
Crohn disease, management after surgical resection (off-label use):
Monotherapy: Oral: 20 mg/kg/day (in 3 divided doses) or 1 to 2 g/day in divided doses for 3 months (ACG [Lichtenstein 2018]; Rutgeerts 1995); begin as soon as oral intake is resumed after surgery (Rutgeerts 1995).
Combination therapy: Oral: 250 mg 3 times daily (D’Haens 2008; Lopez-Sanromán 2017) or 1 to 2 g/day in divided doses for 3 months (ACG [Lichtenstein 2018]); begin as soon as oral intake is resumed after surgery and administer in combination with a thiopurine (azathioprine or mercaptopurine) or a TNF-alpha inhibitor (eg, adalimumab) (De Cruz 2015; D’Haens 2008).
Crohn disease, treatment of simple perianal fistulas (off-label use): Oral: 500 mg twice daily for 4 weeks initially; if clinical response (ie, cessation of drainage and closure of fistula), continue at 250 mg 3 times daily for an additional 4 weeks (Bitton 2019) or 10 to 20 mg/kg/day in divided doses for 4 to 8 weeks with or without ciprofloxacin (ACG [Lichtenstein 2018]).
Dientamoeba fragilis infection (off-label use): Oral: 500 to 750 mg 3 times daily for 10 days (CDC 2012; Nagata 2012).
Giardiasis (alternative agent) (off-label use): Oral: 250 mg 3 times daily or 500 mg 2 times daily for 5 to 7 days (Bartelt 2018; Drugs for Parasitic Infections 2013; Ordonez-Mena 2017).
Helicobacter pylori eradication (off-label use):
Clarithromycin triple regimen: Oral: Metronidazole 500 mg 3 times daily in combination with clarithromycin 500 mg twice daily and a standard-dose or double-dose proton pump inhibitor (PPI) twice daily; continue regimen for 14 days. Note: Avoid use of clarithromycin triple therapy in patients with risk factors for macrolide resistance (eg, prior macrolide exposure, local clarithromycin resistance rates ≥15%) (ACG [Chey 2017]; Fallone 2016).
Bismuth quadruple regimen: Oral: Metronidazole 250 mg 4 times daily or 500 mg 3 or 4 times daily in combination with either bismuth subsalicylate 300 to 524 mg or bismuth subcitrate 120 to 300 mg 4 times daily, tetracycline 500 mg 4 times daily, and a standard-dose PPI twice daily; continue regimen for 10 to 14 days (ACG [Chey 2017]; Fallone 2016).
Concomitant regimen: Oral: Metronidazole 500 mg twice daily in combination with clarithromycin 500 mg twice daily, amoxicillin 1 g twice daily, and a standard-dose PPI twice daily; continue regimen for 10 to 14 days (ACG [Chey 2017]; Fallone 2016).
Sequential regimen (alternative regimen): Oral: Amoxicillin 1 g twice daily plus a standard-dose PPI twice daily for 5 to 7 days; then follow with clarithromycin 500 mg twice daily, metronidazole 500 mg twice daily, and a standard-dose PPI twice daily for 5 to 7 days (ACG [Chey 2017]); some experts prefer the 10-day sequential regimen (amoxicillin for 5 days, followed by metronidazole and clarithromycin for 5 days) over the 14-day sequential regimen (amoxicillin for 7 days, followed by metronidazole and clarithromycin for 7 days) due to the lack of data showing superiority of the 14-day regimen over the 10-day regimen in North America (ACG [Chey 2017]; Crowe 2018).
Hybrid regimen (alternative regimen): Oral: Amoxicillin 1 g twice daily plus a standard-dose PPI twice daily for 7 days; then follow with amoxicillin 1 g twice daily, clarithromycin 500 mg twice daily, metronidazole 500 mg twice daily, and a standard-dose PPI twice daily for 7 days (ACG [Chey 2017]; Wang 2015).
Intra-abdominal infection: Oral, IV: 500 mg every 8 hours as part of an appropriate combination regimen. Duration of therapy is for 4 to 7 days following adequate source control (SIS/IDSA [Solomkin 2010]); for uncomplicated appendicitis and diverticulitis managed nonoperatively, a longer duration is necessary (Barshak 2018; Pemberton 2018). Note: Empiric oral regimens may be appropriate for patients with mild to moderate infection. Other patients may be switched from IV to oral therapy at the same dose when clinically improved and able to tolerate an oral diet (SIS/IDSA [Solomkin 2010]; SIS [Mazuski 2017]).
Intracranial abscess (brain abscess, intracranial epidural abscess): IV: 7.5 mg/kg (usually 500 mg) every 6 to 8 hours for 6 to 8 weeks in combination with other appropriate antimicrobial therapy (Bodilsen 2018; Sexton 2018b; Southwick 2018). Note: May switch IV metronidazole to oral metronidazole at the same dose to complete treatment course (Southwick 2018).
Pelvic inflammatory disease (PID):
Mild to moderate PID: Oral: 500 mg twice daily for 14 days (may be added to a combination of a second- or third-generation parenteral cephalosporin and doxycycline in select women) (CDC [Workowski 2015]).
PID with tubo-ovarian abscess, initial therapy (alternative regimen): IV: 500 mg every 8 hours as part of an appropriate combination regimen (Beigi 2018).
PID with tubo-ovarian abscess, oral therapy following clinical improvement on a parenteral regimen: Oral: 500 mg twice daily with doxycycline to complete at least 14 days of therapy (CDC [Workowski 2015]).
Periodontitis, severe (off-label use): Oral: 500 mg every 8 hours in combination with amoxicillin for 7 to 14 days; used in addition to periodontal debridement (Chow 2019; McGowan 2018; Wilder 2019).
Pneumonia, aspiration (alternative agent): Oral, IV: 500 mg 3 times daily in combination with an appropriate beta-lactam (eg, oral amoxicillin, IV penicillin, or an IV third-generation cephalosporin) for 7 days (Bartlett 2018).
Pouchitis (post ileal pouch-anal anastomosis) (off-label use):
Acute disease (alternative agent): Oral: 500 mg to 1 g every 12 hours for 14 days (Holubar 2010; Navaneethan 2009; Shen 2018; Wall 2011).
Chronic disease: Oral: 500 mg every 12 hours in combination with ciprofloxacin for at least 28 days (Mimura 2002; Shen 2018).
Skin and soft tissue infection:
Necrotizing infection (as a component of an appropriate combination regimen) (alternative agent): IV: 500 mg every 6 hours. Continue until further debridement is not necessary, patient has clinically improved, and patient is afebrile for 48 to 72 hours (IDSA [Stevens 2014]).
Surgical site infection, incisional (eg, intestinal or GU tract; axilla or perineum), warranting anaerobic coverage: IV: 500 mg every 8 hours in combination with other appropriate agents. Duration depends on severity, need for debridement, and clinical response (IDSA [Stevens 2014]).
Surgical prophylaxis:
IV: 500 mg within 60 minutes prior to surgical incision in combination with other antibiotics. Considered a recommended agent for select procedures involving the GI tract, urologic tract, or head and neck (Bratzler 2013).
Oral:
Colorectal surgical prophylaxis (off-label use): 1 g every 3 to 4 hours for 3 doses with additional oral antibiotics, starting after mechanical bowel preparation the evening before a morning surgery and followed by an appropriate IV antibiotic prophylaxis regimen (Bratzler 2013).
Uterine evacuation (induced abortion or pregnancy loss) (alternative agent) (off-label use): 1 g as a single dose ≤12 hours before the procedure (ACOG 2018; Shih 2018).
Tetanus (Clostridium tetani infection) (off-label use): Oral, IV: 500 mg every 6 to 8 hours for 7 to 10 days in combination with supportive therapy (Ahmadsyah 1985; Sexton 2018a).
Trichomoniasis (index case and sex partner):
Initial treatment: Oral: 2 g as a single dose or 500 mg twice daily for 7 days (preferred in HIV-infected women) (Adamski 2014; CDC [Workowski 2015]; Howe 2017; Kissinger 2010; Kissinger 2018; SOGC [van Schalkwyk 2015]). Note: Coverage of trichomoniasis, along with other appropriate antimicrobials, is indicated in cases of recurrent or persistent urethritis in men who have sex with women and who live in regions where T. vaginalis is prevalent and for prophylaxis after sexual assault (CDC [Workowski 2015]).
Persistent or recurrent infection (ie, treatment failure of nitroimidazole [eg, metronidazole] single-dose therapy) (off-label dose): Oral: 500 mg twice daily for 7 days for failure of 2 g single-dose regimen. If this regimen fails, 2 g once daily for 7 days is recommended (CDC [Workowski 2015]).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Some clinicians recommend using adjusted body weight in obese children. Dosing weight = IBW + 0.45 (TBW-IBW)
General dosing, susceptible infection (Red Book [AAP 2018]): Infants, Children, and Adolescents:
Oral: 15 to 50 mg/kg/day in divided doses 3 times daily; maximum daily dose: 2,250 mg/day
IV: 22.5 to 40 mg/kg/day in divided doses 3 or 4 times daily; maximum daily dose: 4,000 mg/day
Amebiasis: Infants, Children, and Adolescents: Oral: 35 to 50 mg/kg/day in divided doses every 8 hours for 7 to 10 days; maximum dose: 750 mg/dose; for severe infection or extraintestinal disease, IV may be necessary (Bradley 2018; Red Book [AAP 2018])
Appendicitis, perforated (divided dosing): Children and Adolescents: IV: 30 mg/kg/day in divided doses 3 times daily (Emil 2003)
Appendicitis, perforated (once-daily dosing): Limited data available: Children and Adolescents: IV: 30 mg/kg/dose once daily in combination with ceftriaxone; maximum reported daily dose: 1,500 mg/day (Yardeni 2013); however, other pediatric trials did not report a maximum; in adult patients, a maximum daily dose of 1,500 mg/day for once-daily dosing is suggested (IDSA [Solomkin 2010]); in pediatric patients, once-daily metronidazole in combination with ceftriaxone has been shown to have similar efficacy as triple-combination therapy with ampicillin, clindamycin, and gentamicin (Fraser 2010; St Peter 2006; St Peter 2008)
Balantidiasis: Infants, Children, and Adolescents: Oral: 35 to 50 mg/kg/day in divided doses every 8 hours for 5 days; maximum dose: 750 mg/dose (Red Book [AAP 2018])
Catheter (peritoneal dialysis); exit-site or tunnel infection: Infants, Children, and Adolescents: Oral: 10 mg/kg/dose 3 times daily. Maximum dose: 500 mg/dose (ISPD [Warady 2012])
Clostridioides (formerly Clostridium) difficile infection:
Infants: Mild to moderate infection: Oral, IV: 7.5 mg/kg/dose every 6 hours for 10 days (Red Book [AAP 2018])
Children and Adolescents:
Non-severe infection, initial or first recurrence: Oral: 7.5 mg/kg/dose 3 to 4 times daily for 10 days; maximum dose: 500 mg/dose (IDSA/SHEA [McDonald 2018])
Severe/fulminant infection, initial: IV: 10 mg/kg/dose every 8 hours for 10 days; maximum dose: 500 mg/dose; use concomitantly with oral or rectal vancomycin (IDSA/SHEA [McDonald 2018])
Dientamoeba fragilis: Infants, Children, and Adolescents: Oral: 35 to 50 mg/kg/day in divided doses every 8 hours for 10 days; maximum dose: 750 mg/dose (Red Book [AAP 2018])
Giardiasis: Infants, Children, and Adolescents: Oral: 15 to 30 mg/kg/day in divided doses every 8 hours for 5 to 7 days; maximum dose: 250 mg/dose (Bradley 2018; Gardner 2001; Granados 2012; Ross 2013; Red Book [AAP 2018])
Helicobacter pylori infection: Children and Adolescents: Oral: 20 mg/kg/day in 2 divided doses for 10 to 14 days in combination with amoxicillin and proton pump inhibitor with or without clarithromycin; maximum daily dose: 1,000 mg/day (NASPGHAN/ESPGHAN [Koletzko 2011])
Inflammatory bowel disease:
Crohn disease, perianal disease; induction: Children and Adolescents: Oral: 7.5 mg/kg/dose 3 times daily for 6 weeks with or without ciprofloxacin; maximum dose: 500 mg/dose (Sandhu 2010)
Ulcerative colitis, pouchitis, persistent: Children and Adolescents: Oral: 20 to 30 mg/kg/day in divided doses 3 times daily for 14 days with or without ciprofloxacin or oral budesonide; maximum dose: 500 mg/dose (Turner 2012)
Intra-abdominal infection: Infants, Children, and Adolescents: IV: 30 to 40 mg/kg/day in divided doses 3 times daily as part of combination therapy; maximum dose: 500 mg/dose (IDSA [Solomkin 2010])
Pelvic inflammatory disease: Adolescents: Oral: 500 mg twice daily for 14 days; give with doxycycline plus a cephalosporin (CDC [Workowski 2015])
Peritonitis (peritoneal dialysis) (ISPD [Warady 2012]):
Prophylaxis: Gastrointestinal or genitourinary procedures: Infants, Children, and Adolescents: IV: 10 mg/kg once prior to procedure in combination with cefazolin; Maximum dose: 1,000 mg/dose
Treatment: Infants, Children, and Adolescents: Oral: 10 mg/kg/dose 3 times daily. Maximum daily dose: 1,200 mg/day
Prophylaxis against sexually transmitted diseases following sexual assault (CDC [Workowski 2015]): Adolescents: Oral: 2,000 mg as a single dose in combination with azithromycin and ceftriaxone
Surgical prophylaxis: Children and Adolescents: IV: 15 mg/kg as a single dose 30 to 60 minutes prior to procedure; maximum single dose: 500 mg (IDSA/ASHP [Bratzler 2013])
Surgical prophylaxis, colorectal: Children and Adolescents: Oral: 15 mg/kg/dose every 3 to 4 hours for 3 doses, starting after mechanical bowel preparation the afternoon and evening before the procedure, with or without additional oral antibiotics and with an appropriate IV antibiotic prophylaxis regimen; maximum dose: 1,000 mg/dose (IDSA/ASHP [Bratzler 2013])
Tetanus (Clostridium tetani infection): Infants, Children, and Adolescents: IV, Oral: 30 mg/kg/day in divided doses 4 times daily for 7 to 10 days; maximum daily dose: 4,000 mg/day (Red Book [AAP 2018])
Trichomoniasis; treatment: Oral:
Children <45 kg: 45 mg/kg/day in divided doses 3 times daily for 7 days; maximum daily dose: 2,000 mg/day (Red Book [AAP 2018])
Children ≥45 kg and Adolescents: 2,000 mg as a single dose once or 500 mg twice daily for 7 days (CDC [Workowski 2015]; Red Book [AAP 2018])
Vaginosis, bacterial: Oral: Children >45 kg and Adolescents: 500 mg twice daily for 7 days (CDC [Workowski 2015]; Red Book [AAP 2018])
Extemporaneously Prepared
Note: A metronidazole suspension (50 mg/mL or 100 mg/mL) is commercially available as a compounding kit.
50 mg/mL Oral Suspension (ASHP Standard Concentration) (ASHP 2017)
A 50 mg/mL oral suspension may be made with tablets and a 1:1 mixture of Ora-Sweet and Ora-Plus. Crush twenty-four 250 mg tablets in a mortar and reduce to a fine powder. Add small portions of the vehicle and mix to a uniform paste; mix while adding the vehicle in incremental portions to almost 120 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 120 mL. Label "shake well". Stable for 60 days at room temperature or refrigerated (Allen 1996).
Allen LV Jr, Erickson MA 3rd. Stability of ketoconazole, metolazone, metronidazole, procainamide hydrochloride, and spironolactone in extemporaneously compounded oral liquids. Am J Health Syst Pharm. 1996;53(17):2073-2078.8870895
Administration
IV: Infuse intravenously over 30 to 60 minutes. Avoid contact of drug solution with equipment containing aluminum.
Oral: Administer with food to minimize stomach upset.
Dietary Considerations
Take with food to minimize stomach upset.
Sodium: Injectable dosage form may contain sodium.
Ethanol: Use of ethanol is contraindicated during therapy and for 3 days after therapy discontinuation.
Storage
Oral: Store at 15°C to 25°C (59°F to 77°F). Protect the tablets from light.
Injection: Store at 20°C to 25°C (68°F to 77°F). Protect from light. Avoid excessive heat. Do not refrigerate. Do not remove unit from overwrap until ready for use. Discard unused solution.
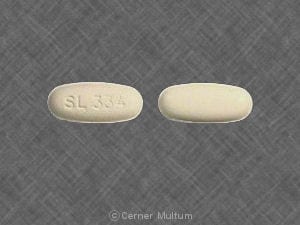
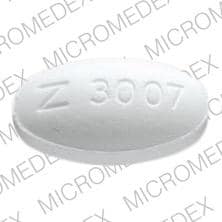
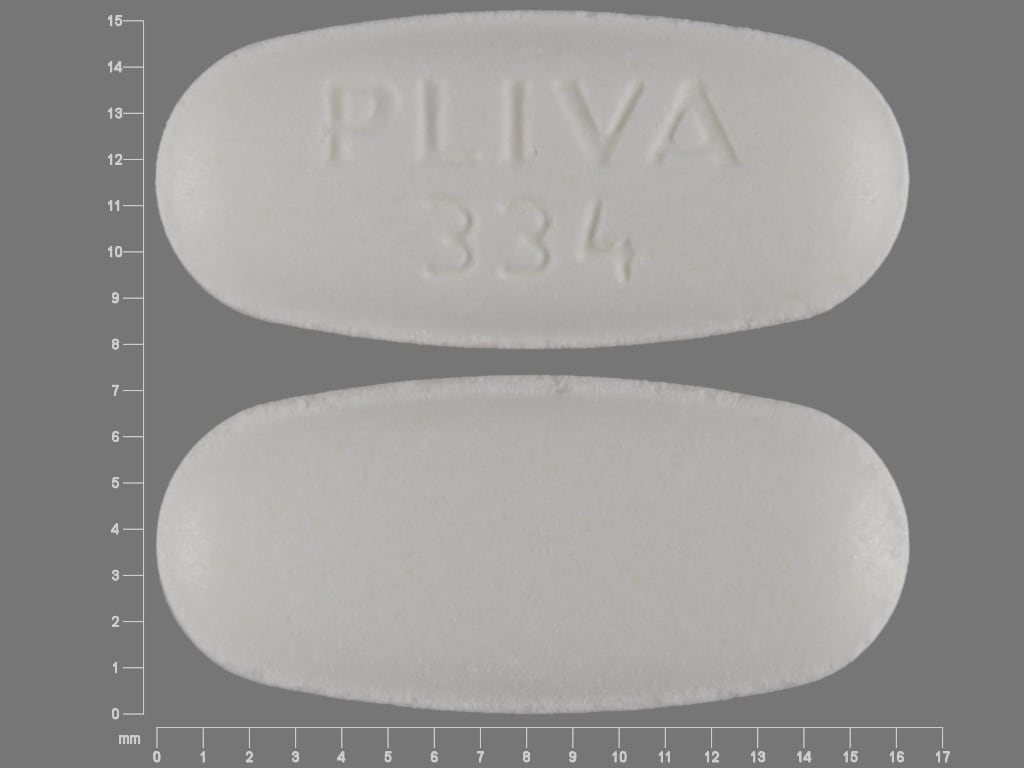
MetroNIDAZOLE (Systemic) Images
Drug Interactions
Alcohol (Ethyl): MetroNIDAZOLE (Systemic) may enhance the adverse/toxic effect of Alcohol (Ethyl). A disulfiram-like reaction may occur. Avoid combination
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Busulfan: MetroNIDAZOLE (Systemic) may increase the serum concentration of Busulfan. Management: The toxic effects of busulfan may be greatly increased with concomitant use of metronidazole. This combination should probably be avoided when possible. If these agents must be used together, increased monitoring for busulfan toxicity is recommended. Consider therapy modification
Carbocisteine: MetroNIDAZOLE (Systemic) may enhance the adverse/toxic effect of Carbocisteine. Specifically, metronidazole may enhance adverse effects of alcohol that is present in liquid formulations of carbocisteine-containing products. Avoid combination
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Disulfiram: May enhance the adverse/toxic effect of MetroNIDAZOLE (Systemic). In particular, the risk for CNS toxicities such as psychosis may be increased. Avoid combination
Dronabinol: MetroNIDAZOLE (Systemic) may enhance the adverse/toxic effect of Dronabinol. Specifically, metronidazole may produce severe intolerance to the alcohol contained in the dronabinol oral solution. Consider therapy modification
Fluorouracil Products: MetroNIDAZOLE (Systemic) may increase the serum concentration of Fluorouracil Products. Monitor therapy
Fosphenytoin: May decrease the serum concentration of MetroNIDAZOLE (Systemic). MetroNIDAZOLE (Systemic) may increase the serum concentration of Fosphenytoin. Monitor therapy
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Lithium: MetroNIDAZOLE (Systemic) may enhance the adverse/toxic effect of Lithium. MetroNIDAZOLE (Systemic) may increase the serum concentration of Lithium. Monitor therapy
Lopinavir: MetroNIDAZOLE (Systemic) may enhance the adverse/toxic effect of Lopinavir. Specifically, the combination of metronidazole and lopinavir/ritonavir solution, which contains 42% alcohol, may result in a disulfiram-like reaction. MetroNIDAZOLE (Systemic) may enhance the arrhythmogenic effect of Lopinavir. Management: Avoid the concomitant use of lopinavir/ritonavir and metronidazole if possible. If these agents are used concomitantly, monitor for QTc prolongation/arrhythmia and if the lopinavir/ritonavir solution is used, development of a disulfiram-like reaction. Consider therapy modification
Mebendazole: May enhance the adverse/toxic effect of MetroNIDAZOLE (Systemic). Particularly the risk for Stevens-Johnson syndrome or toxic epidermal necrolysis may be increased. Avoid combination
Mycophenolate: MetroNIDAZOLE (Systemic) may decrease the serum concentration of Mycophenolate. Specifically, metronidazole may decrease concentrations of the active metabolite of mycophenolate. Monitor therapy
PHENobarbital: May decrease the serum concentration of MetroNIDAZOLE (Systemic). Monitor therapy
Phenytoin: May decrease the serum concentration of MetroNIDAZOLE (Systemic). MetroNIDAZOLE (Systemic) may increase the serum concentration of Phenytoin. Monitor therapy
Primidone: May decrease the serum concentration of MetroNIDAZOLE (Systemic). Monitor therapy
Products Containing Propylene Glycol: MetroNIDAZOLE (Systemic) may enhance the adverse/toxic effect of Products Containing Propylene Glycol. A disulfiram-like reaction may occur. Avoid combination
Ritonavir: May enhance the adverse/toxic effect of MetroNIDAZOLE (Systemic). Specifically, the combination of ritonavir oral solution or ritonavir soft gelatin capsule, both of which contain alcohol, and metronidazole may result in a disulfiram-like reaction. Avoid combination
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Tipranavir: MetroNIDAZOLE (Systemic) may enhance the adverse/toxic effect of Tipranavir. A disulfiram-like reaction may occur due to the alcohol contained in tipranavir capsules. Monitor therapy
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Vecuronium: MetroNIDAZOLE (Systemic) may enhance the neuromuscular-blocking effect of Vecuronium. Monitor therapy
Vitamin K Antagonists (eg, warfarin): MetroNIDAZOLE (Systemic) may increase the serum concentration of Vitamin K Antagonists. Management: Consider alternatives to concomitant therapy with these agents. If concomitant therapy cannot be avoided, consider reducing the dose of the vitamin K antagonist and monitor for increased INR/bleeding. Consider therapy modification
Test Interactions
May interfere with AST, ALT, triglycerides, glucose, and LDH testing
Adverse Reactions
>10%:
Central nervous system: Headache (18%)
Gastrointestinal: Nausea (10% to 12%)
Genitourinary: Vaginitis (15%)
1% to 10%:
Central nervous system: Metallic taste (9%), dizziness (4%)
Dermatologic: Genital pruritus (5%)
Gastrointestinal: Abdominal pain (4%), diarrhea (4%), xerostomia (2%)
Genitourinary: Dysmenorrhea (3%), urine abnormality (3%), urinary tract infection (2%)
Infection: Bacterial infection (7%), candidiasis (3%)
Respiratory: Flu-like symptoms (6%), upper respiratory tract infection (4%), pharyngitis (3%), sinusitis (3%)
Frequency not defined:
Cardiovascular: Chest pain, facial edema, flattened T-wave on ECG, flushing, palpitations, peripheral edema, syncope, tachycardia
Central nervous system: Aseptic meningitis, ataxia, brain disease, cerebral lesion (reversible), chills, confusion, convulsions, depression, disulfiram-like reaction (with alcohol), drowsiness, dysarthria, hypoesthesia, insomnia, irritability, malaise, numbness, paresthesia, peripheral neuropathy, psychosis, seizure, vertigo
Dermatologic: Erythematous rash, hyperhidrosis, pruritus, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Endocrine & metabolic: Decreased libido
Gastrointestinal: Abdominal cramps, abdominal distress, anorexia, constipation, decreased appetite, dysgeusia, glossitis, hairy tongue, pancreatitis (rare), proctitis, stomatitis, vomiting
Genitourinary: Cystitis, dark urine (rare), dyspareunia, dysuria, urinary incontinence, urine discoloration, vaginal dryness, vulvovaginal candidiasis
Hematologic & oncologic: Agranulocytosis, eosinophilia, leukopenia, neutropenia (reversible), thrombocytopenia (reversible, rare)
Hepatic: Increased liver enzymes, jaundice, severe hepatotoxicity (patients with Cockayne syndrome)
Hypersensitivity: Anaphylaxis, hypersensitivity
Immunologic: DRESS syndrome, serum sickness-like reaction (joint pains)
Local: Inflammation at injection site (IV), injection site reaction
Neuromuscular & skeletal: Arthralgia, muscle spasm, myalgia, weakness
Ophthalmic: Abnormal eye movements (saccadic), nystagmus, optic neuropathy
Renal: Polyuria
Respiratory: Dyspnea, nasal congestion, rhinitis
Miscellaneous: Fever
Warnings/Precautions
Concerns related to adverse effects:
- Carcinogenic: [US Boxed Warning]: Possibly carcinogenic based on animal data. Reserve use for conditions described in Use; unnecessary use should be avoided.
- CNS effects: Severe neurological disturbances, including aseptic meningitis (may occur within hours of a dose), cerebellar symptoms (ataxia, dizziness, dysarthria), convulsive seizures, encephalopathy, optic neuropathy, and peripheral neuropathy (usually of sensory type and characterized by numbness or paresthesia of an extremity) have been reported. CNS symptoms and CNS lesions are generally reversible within days to weeks of discontinuation of therapy; peripheral neuropathy symptoms may be prolonged after discontinuation. Avoid repeated or prolonged courses due to risk of cumulative neurotoxicity (IDSA/SHEA [McDonald 2018]). Monitor for neurologic symptoms and discontinue therapy if any abnormal neurologic symptoms occur.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment. Candidiasis infection (known or unknown) may be more prominent during metronidazole treatment, antifungal treatment required.
Disease-related concerns:
- Blood dyscrasias: Use with caution in patients with or history of blood dyscrasias; agranulocytosis, leukopenia, and neutropenia have occurred. Monitor CBC with differential at baseline, during and after treatment.
- Cockayne syndrome: Severe hepatotoxicity/acute hepatic failure (has been fatal) has been reported with systemic metronidazole in patients with Cockayne syndrome; onset is rapid after initiation of treatment. Use metronidazole only after risk vs benefit assessment and if there are no appropriate alternatives in patients with Cockayne syndrome. Obtain LFTs prior to treatment initiation, within the first 2 to 3 days of initiation, frequently during therapy, and after treatment is complete. Discontinue treatment if elevated LFTs occur and monitor until LFTs return to baseline.
- Hepatic impairment: Use with caution in patients with hepatic impairment due to potential accumulation; dosage adjustment recommended in patients with severe hepatic impairment.
- Renal impairment: Use with caution in patients with severe renal impairment or ESRD due to potential accumulation. Accumulated metabolites may be rapidly removed by hemodialysis; supplemental doses may be needed.
- Seizure disorder: Use with caution in patients with a history of seizure disorder.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage-form specific issues:
- Injection: Use injection with caution in patients with heart failure, edema, or other sodium-retaining states, including corticosteroid treatment due to high sodium content. In patients receiving continuous nasogastric secretion aspiration, sufficient metronidazole may be removed in the aspirate to cause a reduction in serum levels.
Other warnings/precautions:
- Ethanol use: Abdominal cramps, nausea, vomiting, headaches, and flushing have been reported with oral and injectable metronidazole and concomitant alcohol consumption (disulfiram-like reactions); avoid alcoholic beverages or products containing propylene glycol during oral or injectable therapy and for at least 3 days after therapy.
Monitoring Parameters
Monitor CBC with differential at baseline, during, and after prolonged or repeated courses of therapy. Monitor LFTs in patients with Cockayne syndrome. Closely monitor elderly patients and patients with severe hepatic impairment or ESRD for adverse reactions. Observe patients carefully if neurologic symptoms occur and consider discontinuation of therapy.
Pregnancy
Pregnancy Considerations
Metronidazole crosses the placenta. Cleft lip with or without cleft palate has been reported following first trimester exposure to metronidazole; however, most studies have not shown an increased risk of congenital anomalies or other adverse events to the fetus following maternal use during pregnancy. Because metronidazole was carcinogenic in some animal species, concern has been raised whether metronidazole should be used during pregnancy. Available studies have not shown an increased risk of infant cancer following metronidazole exposure during pregnancy; however, the ability to detect a signal for this may have been limited.
Metronidazole pharmacokinetics are similar between pregnant and nonpregnant patients (Amon 1981; Visser 1984; Wang 2011).
Bacterial vaginosis and vaginal trichomoniasis are associated with adverse pregnancy outcomes and metronidazole is recommended for the treatment of symptomatic pregnant patients. The dose of oral metronidazole for the treatment of bacterial vaginosis during pregnancy is the same as the CDC recommended twice daily dose in nonpregnant females. When treating vaginal trichomoniasis, the CDC recommends the single oral dose regimen in pregnancy. Although use of metronidazole for vaginal trichomoniasis during the first trimester is contraindicated by the manufacturer; available guidelines note treatment can be given at any stage of pregnancy (CDC [Workowski 2015]).
Metronidazole may also be used for the treatment of giardiasis in pregnant women (some sources recommend second and third trimester administration only) (Gardner 2001; HHS [OI adult 2017]) and symptomatic amebiasis during pregnancy (HHS [OI adult 2017]; Li 1996). Short courses may be used for the treatment of pouchitis or perianal disease in pregnant women with inflammatory bowel disease (avoid use in the first trimester) (van der Woude 2015).The use of other agents is preferred when treatment is needed during pregnancy for Clostridioides (formerly Clostridium) difficile (Surawicz 2013). Consult current recommendations for appropriate use in pregnant women.
Patient Education
What is this drug used for?
- It is used to treat infections.
- It is used to prevent infections during bowel surgery.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Diarrhea
- Constipation
- Lack of appetite
- Abdominal cramps
- Abdominal pain
- Joint pain
- Decreased sex drive
- Injection site irritation
- Metallic taste
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Change in balance
- Dizziness
- Passing out
- Headache
- Trouble speaking
- Seizures
- Thrush
- Vaginal pain, itching, and discharge
- Vision changes
- Irritability
- Depression
- Confusion
- Loss of strength or energy
- Trouble sleeping
- Burning or numbness feeling
- Aseptic meningitis like headache, fever, chills, severe nausea or vomiting, stiff neck, rash, sensitivity to lights, fatigue, or confusion
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.