Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Packet, Oral:
Singulair: 4 mg (30 ea)
Generic: 4 mg (1 ea, 30 ea)
Tablet, Oral:
Singulair: 10 mg
Generic: 10 mg
Tablet Chewable, Oral:
Singulair: 4 mg, 5 mg [contains aspartame]
Generic: 4 mg, 5 mg
Pharmacology
Mechanism of Action
Selective leukotriene receptor antagonist that inhibits the cysteinyl leukotriene receptor. Cysteinyl leukotrienes and leukotriene receptor occupation have been correlated with the pathophysiology of asthma, including airway edema, smooth muscle contraction, and altered cellular activity associated with the inflammatory process, which contribute to the signs and symptoms of asthma. Cysteinyl leukotrienes are also released from the nasal mucosa following allergen exposure leading to symptoms associated with allergic rhinitis (Jarvis, 2000).
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Vd: 8-11 L
Metabolism
Extensively hepatic via CYP3A4, 2C8, and 2C9
Excretion
Feces (86%); urine (<0.2%)
Time to Peak
Tablet: 10 mg: 3 to 4 hours (fasting); Chewable tablet: 4 mg (children 2 to 5 years): 2 hours (fasting); Chewable tablet 5 mg: 2 to 2.5 hours (fasting); Granules: 2.3 ± 1 hours (fasting) and 6.4 ± 2.9 hours (with high-fat meal)
Duration of Action
>24 hours
Half-Life Elimination
2.7-5.5 hours; Mild-to-moderate hepatic impairment: 7.4 hours
Protein Binding
Plasma: >99%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Following a single 10 mg dose, AUC increased 41% and half-life was prolonged to 7.4 hours in patients with mild-to-moderate hepatic impairment and cirrhosis. Patients with severe hepatic impairment or hepatitis have not been evaluated.
Special Populations: Elderly
Plasma half-life is slightly longer in elderly patients.
Special Populations: Children
In children 6-23 months of age, the systemic exposure to montelukast is higher than in adults.
Use: Labeled Indications
Allergic rhinitis (perennial or seasonal): Relief of symptoms of seasonal allergic rhinitis and perennial allergic rhinitis
Asthma: Prophylaxis and chronic treatment of asthma
Bronchoconstriction, exercise-induced (prevention): Prevention of exercise-induced bronchoconstriction.
Note: American Academy of Otolaryngology, Head and Neck Surgery (AAO-HNS) and American Academy of Allergy, Asthma, and Immunology (AAAAI) and American College of Allergy, Asthma, and Immunology (ACAAI) guidelines recommend against montelukast use as first-line therapy for allergic rhinitis (except in patients with concurrent asthma) (Dykewicz 2017; Seidman 2015).
Use: Off Label
Chronic urticariabyes
Data from controlled, double-blind trials regarding the use of montelukast in combination with antihistamines for the management of chronic urticaria are conflicting. Based on clinical practice guidelines from the American Academy of Allergy, Asthma and Immunology (AAAAI); the American College of Allergy, Asthma, and Immunology (ACAAI); the Joint Council of Allergy, Asthma and Immunology (JCAAI); and the World Allergy Organization for the diagnosis and management of acute and chronic urticaria, a leukotriene receptor antagonist may be added to antihistamine therapy in patients who do not respond to antihistamines.
Urticaria (nonsteroidal anti-inflammatory drug-induced)b
Data from a double-blind, placebo-controlled comparison of montelukast and cetirizine in patients with chronic urticaria and intolerance to food additives and/or aspirin supports the use of montelukast in the treatment of patients experiencing urticaria related to the use of nonsteroidal anti-inflammatory drugs Pacor 2001.
Contraindications
Hypersensitivity to montelukast or any component of the formulation
Dosage and Administration
Dosing: Adult
Note: Patients with both asthma and allergic rhinitis should take only one dose in the evening.
Allergic rhinitis (perennial or seasonal): Oral: 10 mg once daily
Asthma: Oral: 10 mg once daily (in the evening)
Bronchoconstriction, exercise-induced (prevention): Oral: 10 mg at least 2 hours prior to exercise. Note: Additional doses should not be administered within 24 hours. Daily administration to prevent exercise-induced bronchoconstriction has not been evaluated. Patients receiving montelukast for another indication should not take an additional dose to prevent exercise-induced bronchoconstriction.
Chronic urticaria (off-label use): Oral: 10 mg once daily (DiLorenzo 2004; Nettis 2004)
Urticaria (nonsteroidal anti-inflammatory drug-induced) (off-label use): Oral: 10 mg once daily (Pacor 2001)
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Patients with both asthma and allergic rhinitis should take only 1 dose in the evening.
Allergic rhinitis:
Perennial: Oral:
Infants ≥6 months and Children <6 years: 4 mg once daily
Children ≥6 years and Adolescents <15 years: 5 mg once daily
Adolescents ≥15 years: 10 mg once daily
Seasonal: Oral:
Children 2 to 5 years: 4 mg once daily
Children ≥6 years and Adolescents <15 years: 5 mg once daily
Adolescents ≥15 years: 10 mg once daily
Asthma, maintenance therapy: Oral:
12 months to 5 years: 4 mg once daily in the evening
6 to 14 years: 5 mg once daily in the evening
≥15 years: 10 mg once daily in the evening
Asthma, acute exacerbation, adjunct therapy: Limited data available: Children 2 to 5 years: Oral: 4 mg as a single dose; in a double-blind, placebo-controlled trial of 52 children with acute asthma exacerbation, a single dose of montelukast (4 mg) with concomitant short-acting beta2-agonist (salbutamol) showed lower respiratory rate and improved pulmonary indices compared to placebo (Harmanci 2006)
Exercise-induced bronchospasm, prevention: Note: Additional doses should not be administered within 24 hours. Daily administration to prevent exercise-induced bronchospasm has not been evaluated. Patients receiving montelukast for another indication should not take an additional dose to prevent exercise-induced bronchoconstriction. Oral:
Children ≥6 years and Adolescents <15 years: 5 mg at least 2 hours prior to exercise
Adolescents ≥15 years: Tablet: 10 mg at least 2 hours prior to exercise
Urticaria (nonsteroidal antiinflammatory drug-induced): Oral: Adolescents ≥15 years: 10 mg once daily (Pacor 2001)
Administration
When treating asthma, administer dose in the evening. Patients with allergic rhinitis may individualize administration time (morning or evening). Patients with both asthma and allergic rhinitis should take a single dose in the evening. May administer without regard to food or meals.
Granules: May be administered directly in the mouth, or mixed with a spoonful of cold or room temperature applesauce, carrots, rice, or ice cream; do not add to any other liquids or foods. Administer within 15 minutes of opening packet.
Dietary Considerations
Some products may contain phenylalanine.
Storage
Store at room temperature of 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Store in original package. Protect from moisture and light. Granules must be used within 15 minutes of opening packet.
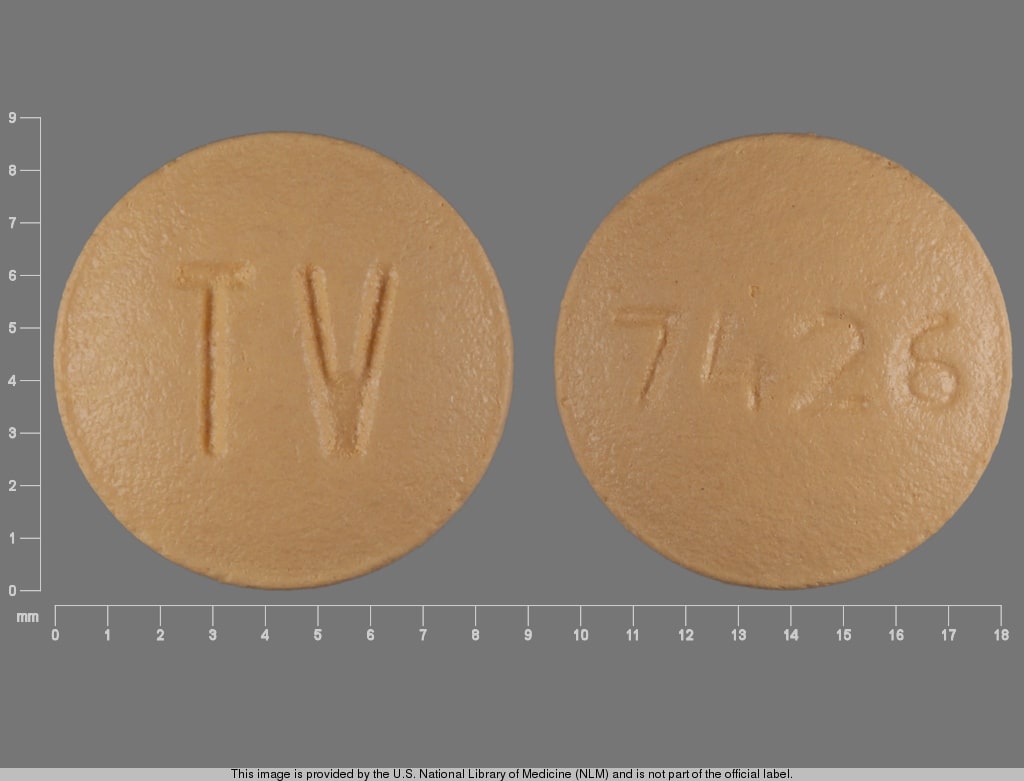
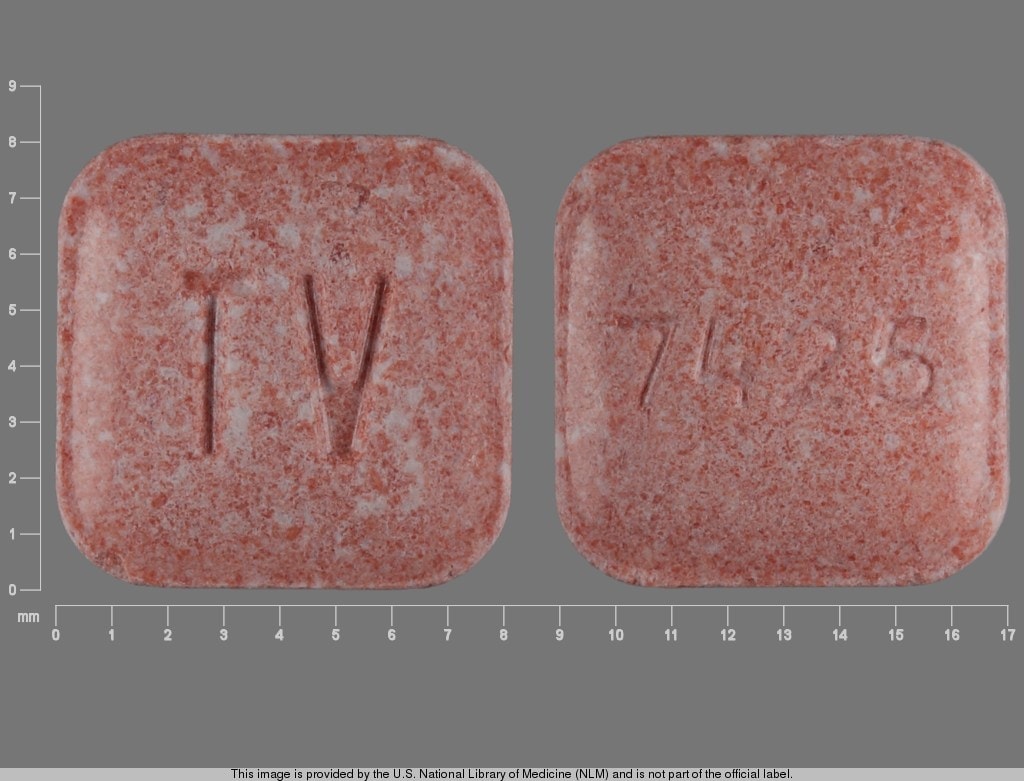
Montelukast Images
Drug Interactions
Gemfibrozil: May increase the serum concentration of Montelukast. Monitor therapy
Loxapine: Agents to Treat Airway Disease may enhance the adverse/toxic effect of Loxapine. More specifically, the use of Agents to Treat Airway Disease is likely a marker of patients who are likely at a greater risk for experiencing significant bronchospasm from use of inhaled loxapine. Management: This is specific to the Adasuve brand of loxapine, which is an inhaled formulation. This does not apply to non-inhaled formulations of loxapine. Avoid combination
Lumacaftor and Ivacaftor: May decrease the serum concentration of Montelukast. Monitor therapy
Adverse Reactions
1% to 10%:
Central nervous system: Headache (children and adolescents: ≥2%), dizziness (adolescents and adults: 2%), fatigue (adolescents and adults: ≤2%)
Dermatologic: Atopic dermatitis (children: ≥2%), dermatitis (children: ≥2%), eczema (children: ≥2%), skin infection (children: ≥2%), urticaria (children: ≥2%), skin rash (2%)
Gastrointestinal: Abdominal pain (children: ≥2%), diarrhea (children and adolescents: ≥2%), nausea (children and adolescents: ≥2%), tooth infection (children: ≥2%), dyspepsia (2%), gastroenteritis (2%), toothache (adolescents and adults: 2%)
Genitourinary: Pyuria (adolescents and adults: 1%)
Hepatic: Increased serum aspartate aminotransferase (adolescents and adults: 2%), increased serum alanine aminotransferase (adolescents and adults: ≥1%)
Infection: Influenza (children and adolescents: ≥2%), varicella zoster infection (children: ≥2%), viral infection (children and adolescents: ≥2%)
Neuromuscular & skeletal: Asthenia (adolescents and adults: ≤2%)
Ophthalmic: Conjunctivitis (children: ≥2%), myopia (children: ≥2%)
Otic: Otalgia (children: ≥2%), otitis (children and adolescents: ≥2%), otitis media (children and adolescents: ≥2%)
Respiratory: Cough (3%), acute bronchitis (children: ≥2%), laryngitis (children and adolescents: ≥2%), pharyngitis (children: ≥2%), pneumonia (children: ≥2%), rhinitis (infective; children: ≥2%), rhinorrhea (children: ≥2%), nasal congestion (adolescents and adults: 2%), epistaxis (adolescents and adults: ≥1%), sinus headache (adolescents and adults: ≥1%), sinusitis (≥1%), upper respiratory tract infection (≥1%)
Miscellaneous: Fever (2%), trauma (adolescents and adults: 1%)
<1%, postmarketing and/or case reports: Abnormal dreams, aggressive behavior, agitation, anaphylaxis, angioedema, anxiety, arthralgia, behavioral changes, bleeding tendency disorder, bruise, depression, diarrhea, disorientation, drowsiness, edema, eosinophilia (systemic), eosinophilic granulomatosis with polyangiitis, eosinophilic pneumonitis, epistaxis, erythema multiforme, erythema nodosum, hallucination, hepatic eosinophilic infiltration, hepatitis (mixed pattern, hepatocellular, and cholestatic), hostility, hypersensitivity reaction, hypoesthesia, insomnia, irritability, lack of concentration, memory impairment, mood changes, muscle cramps, myalgia, nausea, obsessive compulsive disorder, palpitations, pancreatitis, paresthesia, pruritus, restlessness, seizure, somnambulism, Stevens-Johnson syndrome, stuttering, suicidal ideation, suicidal tendencies, thrombocytopenia, tic disorder, toxic epidermal necrolysis, tremor, urinary incontinence, urticaria, vasculitis, vomiting
Warnings/Precautions
Concerns related to adverse effects:
- Eosinophilia and vasculitis: In rare cases, patients may present with systemic eosinophilia, sometimes presenting with clinical features of vasculitis consistent with eosinophilic granulomatosis with polyangiitis (formerly known as Churg-Strauss), a condition which is often treated with systemic corticosteroid therapy. Health care providers should be alert to eosinophilia, vasculitic rash, worsening pulmonary symptoms, cardiac complications, and/or neuropathy presenting in their patients. A causal association between montelukast and these underlying conditions has not been established.
- Neuropsychiatric events: Postmarketing reports of behavioral changes (eg, abnormal dreams, agitation, aggression, anxiety, attention deficit, depression, disorientation, hallucinations, hostility, insomnia, irritability, memory disturbances, restlessness, sleep disturbance, suicide ideation/behavior, and tremor) have been noted in pediatric, adolescent, and adult patients. In a retrospective analysis performed by Merck, serious behavior-related events were rare (Philip 2009a); assess patients for behavioral changes. Patients should be instructed to notify the prescriber if behavioral changes occur.
Disease related concerns:
- Acute asthma/bronchospasm: Not FDA approved for use in the reversal of bronchospasm in acute asthma attacks, including status asthmaticus. Some studies, however, support its use as adjunctive therapy (Cylly 2003; Ferreira 2001; Harmancik 2006). Appropriate rescue medication should be available. Montelukast treatment should continue during acute asthma exacerbation.
- Aspirin-sensitive asthmatics: Montelukast will not interrupt bronchoconstrictor response to aspirin or other NSAIDs. Patients with known aspirin sensitivity should continue to avoid these agents.
Concurrent drug therapy issues:
- Corticosteroids: When inhaled or systemic corticosteroid reduction is considered in patients initiating or receiving montelukast, appropriate clinical monitoring and a gradual dose reduction of the steroid are recommended.
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Chewable tablet: Contains phenylalanine.
Monitoring Parameters
Mood or behavior changes, including suicidal thinking/behavior
Pregnancy
Pregnancy Considerations
Based on available data, an increased risk of teratogenic effects has not been observed with montelukast use in pregnancy (BTS 2016; GINA 2018).
Uncontrolled asthma is associated with adverse events on pregnancy (increased risk of perinatal mortality, preeclampsia, preterm birth, low birth weight infants). Poorly controlled asthma or asthma exacerbations may have a greater fetal/maternal risk than what is associated with appropriately used asthma medications. When clinically indicated, treatment with montelukast should not be withheld during pregnancy (BTS 2016; GINA 2018).
Patient Education
What is this drug used for?
- It is used to ease allergy signs.
- It is used to prevent exercise-induced breathing problems.
- It is used to treat or prevent asthma.
- It may be given to you for other reasons. Talk with the doctor.
For asthma:
- Do not use this drug to treat an asthma attack. Use a rescue inhaler. Talk with your doctor.
Frequently reported side effects of this drug
- Cough
- Diarrhea
- Headache
- Common cold symptoms
- Abdominal pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting.
- Depression like thoughts of suicide, anxiety, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- Sleepwalking
- Sensing things that seem real but are not
- Behavioral changes
- Trouble with memory
- Nightmares
- Restlessness
- Trouble focusing
- Abnormal movements
- Seizures
- Trouble breathing
- Flu-like symptoms
- Sinus pain
- Muscle pain
- Joint pain
- Swelling
- Bedwetting (children)
- Chest pain
- Abnormal heartbeat
- Bruising
- Bleeding
- Confusion
- Burning or numbness feeling
- Ear pain
- Tremors
- Trouble speaking
- Trouble sleeping
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.