Boxed Warning
Addiction, abuse, and misuse:
Oxymorphone exposes patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient's risk prior to prescribing oxymorphone, and monitor all patients regularly for the development of these behaviors and conditions.
Opioid analgesic risk evaluation and mitigation strategy (REMS)
To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the FDA has required a REMS for these products. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS-compliant education programs available to health care providers. Health care providers are strongly encouraged to complete a REMS-compliant education program and counsel patients and/or their caregivers, with every prescription, on safe use, serious risks, storage, and disposal of these products; emphasize to patients and their caregivers the importance of reading the Medication Guide every time it is provided by their pharmacist, and consider other tools to improve patient, household, and community safety.
Life-threatening respiratory depression:
Serious, life-threatening, or fatal respiratory depression may occur with use of oxymorphone. Monitor for respiratory depression, especially during initiation of oxymorphone or following a dose increase. Instruct patients to swallow oxymorphone extended-release (ER) tablets whole; crushing, chewing, or dissolving oxymorphone ER tablets can cause rapid release and absorption of a potentially fatal dose of oxymorphone.
Accidental ingestion (oral only):
Accidental ingestion of even 1 dose of oxymorphone, especially by children, can result in a fatal overdose of oxymorphone.
Neonatal opioid withdrawal syndrome:
Prolonged use of oxymorphone during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available.
Interaction with alcohol (oral only):
Instruct patients not to consume alcoholic beverages or use prescription or nonprescription products that contain alcohol while taking oxymorphone. The coingestion of alcohol with oxymorphone may result in increased plasma levels and a potentially fatal overdose of oxymorphone
Risks from concomitant use with benzodiazepines or other CNS depressants:
Concomitant use of opioids with benzodiazepines or other CNS depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of oxymorphone and benzodiazepine or other CNS depressants for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Injection, as hydrochloride:
Opana: 1 mg/mL (1 mL [DSC])
Tablet, Oral, as hydrochloride:
Opana: 5 mg [contains fd&c blue #2 aluminum lake]
Opana: 10 mg [contains d&c red #30 aluminum lake]
Generic: 5 mg, 10 mg
Tablet ER 12 Hour Abuse-Deterrent, Oral, as hydrochloride:
Opana ER: 5 mg [DSC], 7.5 mg [DSC]
Opana ER: 10 mg [DSC] [contains fd&c yellow #6 (sunset yellow)]
Opana ER: 15 mg [DSC]
Opana ER: 20 mg [DSC] [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Opana ER: 30 mg [DSC]
Opana ER: 40 mg [DSC] [contains fd&c yellow #10 (quinoline yellow), fd&c yellow #6 (sunset yellow)]
Tablet Extended Release 12 Hour, Oral, as hydrochloride:
Generic: 5 mg, 7.5 mg, 10 mg, 15 mg, 20 mg, 30 mg, 40 mg
Pharmacology
Mechanism of Action
Oxymorphone is a potent opioid analgesic with uses similar to those of morphine. The drug is a semisynthetic derivative of morphine (phenanthrene derivative) and is closely related to hydromorphone chemically (Dilaudid).
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: IV: 1.94 to 4.22 L/kg
Metabolism
Hepatic via glucuronidation to active and inactive metabolites
Excretion
Urine (<1% as unchanged drug); feces
Onset of Action
Parenteral: 5 to 10 minutes
Duration of Action
Analgesic: Parenteral: 3 to 6 hours
Half-Life Elimination
Oral: Immediate release: 7 to 9 hours; Extended release: 9 to 11 hours
Protein Binding
10% to 12%
Use in Specific Populations
Special Populations: Renal Function Impairment
There is an increase of 26%, 57%, and 65% in bioavailability in patients with mild, moderate, and severe renal impairment, respectively.
Special Populations: Hepatic Function Impairment
Bioavailability of orally administered oxymorphone may be markedly increased in patients with moderate to severe hepatic impairment.
Special Populations: Elderly
On average, patients >65 years of age experience 1.4- and 1.5-fold increases in oxymorphone AUC and Cmax, respectively.
Use: Labeled Indications
Pain management:
Parenteral: Management of pain severe enough to require an opioid analgesic and for which alternative treatments are inadequate; obstetrical analgesia; preoperative medication; anesthesia support; relief of anxiety in patients with dyspnea associated with pulmonary edema secondary to acute left ventricular dysfunction.
Oral, immediate release: Management of acute pain severe enough to require an opioid analgesic and for which alternative treatments are inadequate.
Oral, extended release: Management of pain severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate.
Limitations of use: Reserve oxymorphone for use in patients for whom alternative treatment options (eg, nonopioid analgesics, opioid combination products) are ineffective, not tolerated, or would be otherwise inadequate to provide sufficient pain management. Oxymorphone ER is not indicated as an as-needed analgesic.
Contraindications
Hypersensitivity (eg, anaphylaxis, angioedema) to oxymorphone or any component of the formulation; significant respiratory depression; acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment; GI obstruction, including paralytic ileus (known or suspected); moderate and severe hepatic impairment.
Documentation of allergenic cross-reactivity for opioids is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Note: Opana injection has been discontinued in the United States for more than 1 year.
Pain management: Note: Dosage must be individualized.
Parenteral:
IM, SubQ: Initial: 1 to 1.5 mg; may repeat every 4 to 6 hours as needed
Labor analgesia: IM: 0.5 to 1 mg
IV: Initial: 0.5 mg
Conversion from oral oxymorphone to parenteral oxymorphone: Initiate parenteral oxymorphone with approximately one-tenth (1/10) of the total daily oral dose and administer in 4 or 6 equally divided doses. Due to patient variability, closely monitor patient for analgesia and adverse reactions upon conversion.
Oral:
Immediate release: Acute pain:
Opioid-naive: Initial: 5 to 10 mg every 4 to 6 hours as needed (American Pain Society [Miaskowski 2016]). Dosage adjustment should be based on level of analgesia, side effects, pain intensity, and patient comorbidities.
Conversion from a stable dose of parenteral oxymorphone: Initiate oral oxymorphone with approximately 10 times the total daily parenteral requirement administered in 4 to 6 equally divided doses.
Conversion from other opioids: Use standard conversion chart to convert total daily dose of current opioid to oxymorphone equivalent. Generally, start with one-half (1/2) the calculated total daily oxymorphone dosage and administer in divided doses every 4 to 6 hours.
Extended release: Chronic pain:
Opioid-naive (use as the first opioid analgesic or in patients who are not opioid tolerant): Initial: 5 mg every 12 hours.
Note: Opioid tolerance is defined as: Patients already taking at least 60 mg of oral morphine daily, 25 mcg of transdermal fentanyl per hour, 30 mg of oral oxycodone daily, 8 mg oral hydromorphone daily, 25 mg oral oxymorphone daily, or an equivalent dose of another opioid for at least 1 week.
Conversion from stable dose of parenteral oxymorphone to extended-release oxymorphone: Initiate extended-release oxymorphone with approximately 10 times the total daily parenteral requirement administered in 2 equally divided doses. Due to patient variability, closely monitor patient for analgesia and adverse reactions upon conversion.
Conversion of stable dose of immediate-release oxymorphone to extended-release oxymorphone: Using the same total daily dose, administer one-half (1/2) of the daily dose of immediate-release oxymorphone as the extended-release formulation every 12 hours
Conversion from other oral opioids to extended-release oxymorphone: Discontinue all other around-the-clock opioids when extended release oxymorphone is initiated. Substantial interpatient variability exists in relative potency of opioids. Therefore, it is safer to underestimate a patient’s daily oral oxymorphone requirement and provide breakthrough pain relief with rescue medication (eg, immediate release opioid) than to overestimate requirements. The conversion factors, per the manufacturer, in the chart (see table) provide an estimate to convert the daily dose of current opioid to an oxymorphone equivalent. Select the prior oral opioid, sum the current total daily dose, multiply by the conversion factor on the table to calculate the approximate oral oxymorphone daily dose, then divide daily dose by 2 to administer every 12 hours as oxymorphone extended release. Round down, if necessary, to the nearest strength available. For patients on a regimen of more than one opioid, calculate the approximate oral oxymorphone dose for each opioid and sum the totals to obtain the approximate total oxymorphone daily dose. For patients on a regimen of fixed-ratio opioid/nonopioid analgesic medications, only the opioid component of these medications should be used in the conversion. Note: The conversion factors in this conversion table are only to be used for the conversion from current opioid therapy to oxymorphone ER. Conversion factors in this table cannot be used to convert from oxymorphone ER to another opioid (doing so may lead to fatal overdose due to overestimation of the new opioid). This is not a table of equianalgesic doses. When converting from methadone to extended release oxymorphone, close monitoring is required. Ratio between methadone and other opioid agonists varies widely according to previous dose exposure. Methadone has a long half-life and can accumulate in the plasma.
|
Prior Oral Opioid |
Approximate Oral Conversion Factor |
|---|---|
|
Oxymorphone |
1 |
|
Hydrocodone |
0.5 |
|
Oxycodone |
0.5 |
|
Methadone |
0.5 |
|
Morphine |
0.333 |
Conversion Factors to Oxymorphone ER
Prior oral opioid: Oxymorphone
Approximate oral conversion factor: 1
Prior oral opioid: Hydrocodone
Approximate oral conversion factor: 0.5
Prior oral opioid: Oxycodone
Approximate oral conversion factor: 0.5
Prior oral opioid: Methadone
Approximate oral conversion factor: 0.5
Prior oral opioid: Morphine
Approximate oral conversion factor: 0.333
Titration and maintenance: Adjust therapy incrementally by 5 to 10 mg every 12 hours at intervals of every 3 to 7 days. Breakthrough pain may require a dose increase or rescue medication with an immediate-release analgesic.
Discontinuation of therapy: When discontinuing chronic opioid therapy, the dose should be gradually tapered down. An optimal universal tapering schedule for all patients has not been established (CDC [Dowell 2016]). Proposed schedules range from slow (eg, 10% reductions per week) to rapid (eg, 25% to 50% reduction every few days) (CDC 2015). Tapering schedules should be individualized to minimize opioid withdrawal while considering patient-specific goals and concerns as well as the pharmacokinetics of the opioid being tapered. An even slower taper may be appropriate in patients who have been receiving opioids for a long duration (eg, years), particularly in the final stage of tapering, whereas more rapid tapers may be appropriate in patients experiencing severe adverse events (CDC [Dowell 2016]). Monitor carefully for signs/symptoms of withdrawal. If the patient displays withdrawal symptoms, consider slowing the taper schedule; alterations may include increasing the interval between dose reductions, decreasing amount of daily dose reduction, pausing the taper and restarting when the patient is ready, and/or coadministration of an alpha-2 agonist (eg, clonidine) to blunt withdrawal symptoms (Berna 2015; CDC [Dowell 2016]). Continue to offer nonopioid analgesics as needed for pain management during the taper; consider nonopioid adjunctive treatments for withdrawal symptoms (eg, GI complaints, muscle spasm) as needed (Berna 2015; Sevarino 2018).
Dosing: Geriatric
Refer to adult dosing. Note: Initiate dosing at the lower end of the dosage range; titrate slowly with careful monitoring.
Administration
Oral: Administer on an empty stomach, 1 hour before or 2 hours after eating. Swallow ER tablet whole; do not break, crush, dissolve, or chew.
Injectable: Administer IV, IM, or SubQ.
Dietary Considerations
Immediate release and extended release tablets should be taken 1 hour before or 2 hours after eating.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect injection from light.
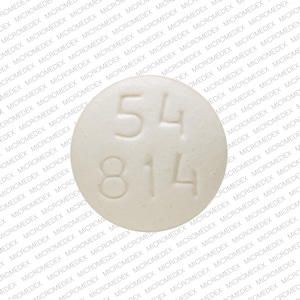
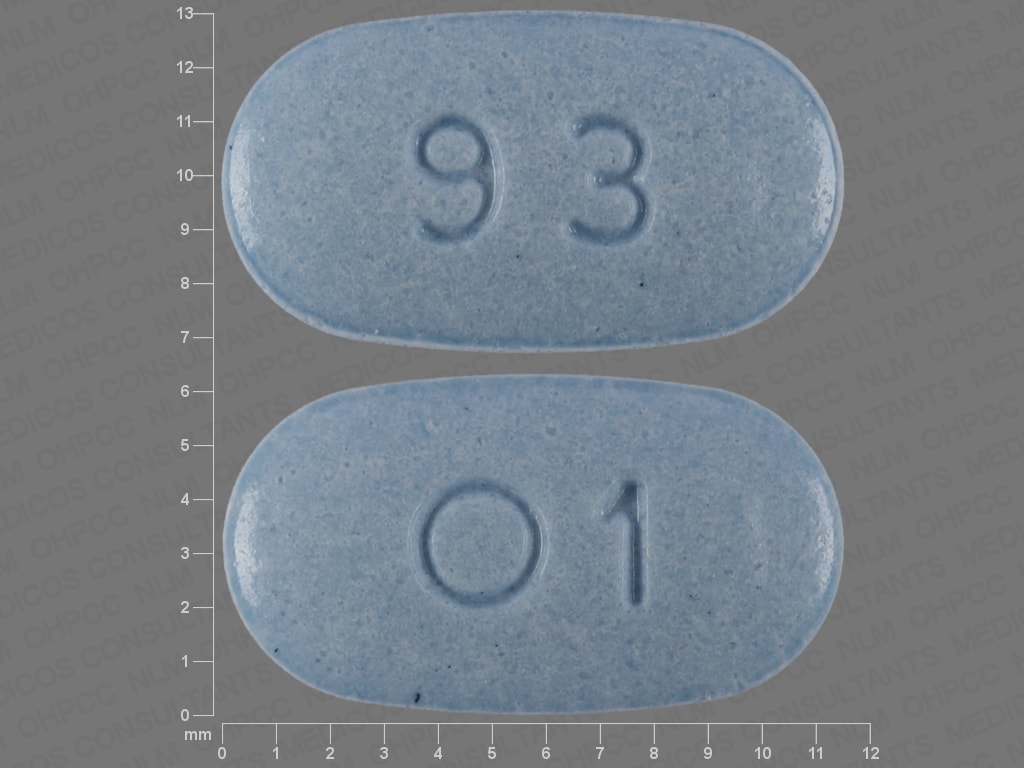
Oxymorphone Images
Drug Interactions
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Alvimopan: Opioid Agonists may enhance the adverse/toxic effect of Alvimopan. This is most notable for patients receiving long-term (i.e., more than 7 days) opiates prior to alvimopan initiation. Management: Alvimopan is contraindicated in patients receiving therapeutic doses of opioids for more than 7 consecutive days immediately prior to alvimopan initiation. Consider therapy modification
Amphetamines: May enhance the analgesic effect of Opioid Agonists. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Desmopressin: Opioid Agonists may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Diuretics: Opioid Agonists may enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Eluxadoline: Opioid Agonists may enhance the constipating effect of Eluxadoline. Avoid combination
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Gastrointestinal Agents (Prokinetic): Opioid Agonists may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Monoamine Oxidase Inhibitors: OxyMORphone may enhance the adverse/toxic effect of Monoamine Oxidase Inhibitors. Avoid combination
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nalmefene: May diminish the therapeutic effect of Opioid Agonists. Management: Avoid the concomitant use of nalmefene and opioid agonists. Discontinue nalmefene 1 week prior to any anticipated use of opioid agonistss. If combined, larger doses of opioid agonists will likely be required. Consider therapy modification
Naltrexone: May diminish the therapeutic effect of Opioid Agonists. Management: Seek therapeutic alternatives to opioids. See full drug interaction monograph for detailed recommendations. Consider therapy modification
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Opioids (Mixed Agonist / Antagonist): May diminish the analgesic effect of Opioid Agonists. Management: Seek alternatives to mixed agonist/antagonist opioids in patients receiving pure opioid agonists, and monitor for symptoms of therapeutic failure/high dose requirements (or withdrawal in opioid-dependent patients) if patients receive these combinations. Avoid combination
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pegvisomant: Opioid Agonists may diminish the therapeutic effect of Pegvisomant. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Ramosetron: Opioid Agonists may enhance the constipating effect of Ramosetron. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Serotonergic Agents (High Risk): Opioid Agonists may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Succinylcholine: May enhance the bradycardic effect of Opioid Agonists. Monitor therapy
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
Some quinolones may produce a false-positive urine screening result for opioids using commercially-available immunoassay kits. This has been demonstrated most consistently for levofloxacin and ofloxacin, but other quinolones have shown cross-reactivity in certain assay kits. Confirmation of positive opioid screens by more specific methods should be considered. May cause elevation in amylase (due to constriction of the sphincter of Oddi).
Adverse Reactions
Incidence usually on higher end with extended release (ER) tablet.
>10%:
Central nervous system: Dizziness (5% to 18%), drowsiness (2% to 17%), headache (3% to 12%)
Dermatologic: Pruritus (3% to 15%)
Gastrointestinal: Nausea (3% to 33%), constipation (4% to 28%), vomiting (9% to 16%)
Miscellaneous: Fever (1% to 14%)
1% to 10%:
Cardiovascular: Edema (oral), flushing, hypertension (oral), hypotension, tachycardia
Central nervous system: Fatigue (4%), insomnia (4%), confusion (3%), anxiety (oral), depression, disorientation (oral), lethargy (oral), nervousness, restlessness
Dermatologic: Diaphoresis
Endocrine & metabolic: Dehydration (oral), weight loss (oral)
Gastrointestinal: Xerostomia (6%), abdominal pain (3%), decreased appetite (oral: 3%), abdominal distention, diarrhea (oral), dyspepsia (oral), flatulence
Neuromuscular & skeletal: Asthenia
Ophthalmic: Blurred vision
Respiratory: Dyspnea, hypoxia
Frequency not defined:
Central nervous system: Agitation, cognitive dysfunction, drug abuse, opioid dependence, sedation
Dermatologic: Allergic dermatitis
Endocrine & metabolic: Adrenocortical insufficiency
Gastrointestinal: Anorexia, biliary colic, paralytic ileus
Genitourinary: Oliguria, ureteral spasm, urinary hesitancy
Local: Injection site reaction
Ophthalmic: Diplopia
Respiratory: Apnea, atelectasis, bronchospasm, laryngeal edema, laryngospasm
<1%, postmarketing, and/or case reports: Anaphylaxis, angioedema, bradycardia, bradypnea, central nervous system depression, choking sensation (tablets), cold and clammy skin, decreased oxygen saturation, dermatitis, difficulty in micturition, dysphagia, dysphoria, euphoria, facial edema, foreign body sensation (tablet stuck in throat), gag reflex (tablets; including regurgitation), hallucination, hand edema, hot flash, hypersensitivity reaction, hypogonadism (Brennan 2013; Debono 2011), impaired consciousness, increased serum prolactin (Molitch 2008; Vuong 2010), intestinal obstruction, lip edema, mental status changes, miosis, mouth edema, orthostatic hypotension, palpitations, periorbital edema, pharyngeal edema, respiratory depression, respiratory distress, skin rash, syncope, tongue edema, urinary retention, urticaria, visual disturbance
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Constipation: May cause constipation which may be problematic in patients with unstable angina and patients post-myocardial infarction. Consider preventive measures (eg, stool softener, increased fiber) to reduce the potential for constipation.
- Hypotension: May cause severe hypotension (including orthostatic hypotension and syncope); use with caution in patients with hypovolemia, cardiovascular disease (including acute MI), or with drugs which may exaggerate hypotensive effects (including phenothiazines or general anesthetics). Monitor for symptoms of hypotension following initiation or dose titration. Avoid use in patients with circulatory shock.
- Phenanthrene hypersensitivity: Use with caution in patients with hypersensitivity reactions to other phenanthrene-derivative opioid agonists (codeine, hydrocodone, hydromorphone, levorphanol, oxycodone).
- Respiratory depression: [US Boxed Warning]: Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely for respiratory depression, especially during initiation or dose escalation. Swallow ER tablets whole; crushing, chewing, or dissolving can cause rapid release and a potentially fatal dose. Carbon dioxide retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids.
- Thrombotic thrombocytopenic purpura (TTP): Cases of TTP resulting in kidney failure (requiring dialysis) and death have been reported as a result of misuse by drug abusers injecting the extended-release tablets intravenously. Tablets are intended for oral administration only.
Disease-related concerns:
- Abdominal conditions: May obscure diagnosis or clinical course of patients with acute abdominal conditions.
- Adrenocortical insufficiency: Use with caution in patients with adrenal insufficiency, including Addison disease. Long-term opioid use may cause secondary hypogonadism, which may lead to sexual dysfunction, infertility, mood disorders, and osteoporosis (Brennan 2013).
- Biliary tract impairment: Use with caution in patients with biliary tract dysfunction including acute pancreatitis; opioids may cause constriction of sphincter of Oddi.
- CNS depression/coma: Avoid use in patients with impaired consciousness or coma as these patients are susceptible to intracranial effects of CO2 retention.
- Delirium tremens: Use with caution in patients with delirium tremens.
- Head trauma: Use with extreme caution in patients with head injury, intracranial lesions, or elevated intracranial pressure (ICP); exaggerated elevation of ICP may occur.
- Hepatic impairment: Use with caution in patients with mild hepatic impairment; use is contraindicated in moderate to severe impairment.
- Mental health conditions: Use opioids with caution for chronic pain in patients with mental health conditions (eg, depression, anxiety disorders, post-traumatic stress disorder) due to increased risk for opioid use disorder and overdose; more frequent monitoring is recommended (Dowell [CDC 2016]).
- Obesity: Use with caution in patients who are morbidly obese.
- Prostatic hyperplasia/urinary stricture: Use with caution in patients with prostatic hyperplasia and/or urinary stricture.
- Psychosis: Use with caution in patients with toxic psychosis.
- Renal impairment: Use with caution in patients with renal impairment.
- Respiratory disease: Use with caution and monitor for respiratory depression in patients with significant chronic obstructive pulmonary disease or cor pulmonale, and those with a substantially decreased respiratory reserve, hypoxia, hypercarbia, or preexisting respiratory depression, particularly when initiating therapy and titrating therapy; critical respiratory depression may occur, even at therapeutic dosages. Consider the use of alternative nonopioid analgesics in these patients.
- Seizure disorders: Use with caution in patients with seizure disorders; may cause or exacerbate preexisting seizures.
- Sleep-related disorders: Opioid use increases the risk for sleep-related disorders (eg, central sleep apnea [CSA], hypoxemia) in a dose-dependent fashion. Use with caution for chronic pain and titrate dosage cautiously in patients with risk factors for sleep-disordered breathing (eg, heart failure and obesity). Consider dose reduction in patients presenting with CSA. Avoid opioids in patients with moderate to severe sleep-disordered breathing (Dowell [CDC 2016]).
- Thyroid dysfunction: Use with caution in patients with thyroid dysfunction.
Concurrent drug therapy issues:
- Benzodiazepines or other CNS depressants: [US Boxed Warning]: Concomitant use of opioids with benzodiazepines or other CNS depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of oxymorphone and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate. Limit dosage and durations to the minimum required and follow patients for signs and symptoms of respiratory depression and sedation.
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Ethanol use: Oral: [US Boxed Warning]: Patients should not consume alcoholic beverages or medication containing ethanol while taking oxymorphone; ethanol may increase oxymorphone plasma levels resulting in a potentially fatal overdose.
Special populations:
- Cachectic or debilitated patients: Use with caution in debilitated or cachectic patients; there is a greater potential for critical respiratory depression, even at therapeutic dosages. Consider the use of alternative nonopioid analgesics in these patients.
- Elderly: Use with caution in the elderly; may be more sensitive to adverse effects. Decrease initial dose. Use opioids for chronic pain with caution in this age group; monitor closely due to an increased potential for risks, including certain risks such as falls/fracture, cognitive impairment, and constipation. Clearance may also be reduced in older adults (with or without renal impairment) resulting in a narrow therapeutic window and increasing the risk for respiratory depression or overdose (Dowell [CDC 2016]). Consider the use of alternative nonopioid analgesics in these patients.
- Neonates: Neonatal withdrawal syndrome: [US Boxed Warning]: Prolonged use of opioids during pregnancy can cause neonatal withdrawal syndrome, which may be life-threatening if not recognized and treated according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, ensure treatment is available and warn patient of risk to the neonate. Signs and symptoms include irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea and failure to gain weight. Onset, duration and severity depend on the drug used, duration of use, maternal dose, and rate of drug elimination by the newborn.
Dosage form specific issues:
- Extended-release tablets: Therapy should only be prescribed by healthcare professionals familiar with the use of potent opioids for chronic pain. Reports of intestinal obstruction requiring medical intervention to remove the tablet have been reported (rare). Consider use of an alternative analgesic in patients who have difficulty swallowing and patients at risk for underlying GI disorders resulting in a small gastrointestinal lumen (eg, patients with esophageal cancer or colon cancer with a small GI lumen).
Other warnings/precautions:
- Abrupt discontinuation/withdrawal: Abrupt discontinuation in patients who are physically dependent to opioids has been associated with serious withdrawal symptoms, uncontrolled pain, attempts to find other opioids (including illicit), and suicide. Use a collaborative, patient-specific taper schedule that minimizes the risk of withdrawal, considering factors such as current opioid dose, duration of use, type of pain, and physical and psychological factors. Monitor pain control, withdrawal symptoms, mood changes, suicidal ideation, and for use of other substances and provide care as needed. Concurrent use of mixed agonist/antagonist analgesics (eg, pentazocine, nalbuphine, butorphanol) or partial agonist (eg, buprenorphine) analgesics may also precipitate withdrawal symptoms and/or reduced analgesic efficacy in patients following prolonged therapy with mu opioid agonists.
- Abuse/misuse/diversion: [US Boxed Warning]: Use exposes patients and other users to the risks of addiction, abuse, and misuse, potentially leading to overdose and death. Assess each patient's risk prior to prescribing; monitor all patients regularly for development of these behaviors or conditions. Use with caution in patients with a history of drug abuse or acute alcoholism; potential for drug dependency exists. Other factors associated with increased risk for misuse include younger age, concomitant depression (major), and psychotropic medication use. Consider offering naloxone prescriptions in patients with factors associated with an increased risk for overdose, such as history of overdose or substance use disorder, higher opioid dosages (≥50 morphine milligram equivalents/day orally), and concomitant benzodiazepine use (Dowell [CDC 2016]).
- Accidental exposure: Oral: [US Boxed Warning]: Accidental ingestion of even one dose, especially in children, can result in a fatal overdose of oxymorphone.
- Appropriate use: Chronic pain (outside of end-of-life or palliative care, active cancer treatment, sickle cell disease, or medication-assisted treatment for opioid use disorder) in outpatient setting in adults: Opioids should not be used as first-line therapy for chronic pain management (pain >3-month duration or beyond time of normal tissue healing) due to limited short-term benefits, undetermined long-term benefits, and association with serious risks (eg, overdose, MI, auto accidents, risk of developing opioid use disorder). Preferred management includes nonpharmacologic therapy and nonopioid therapy (eg, NSAIDs, acetaminophen, certain anticonvulsants and antidepressants). If opioid therapy is initiated, it should be combined with nonpharmacologic and nonopioid therapy, as appropriate. Prior to initiation, known risks of opioid therapy should be discussed and realistic treatment goals for pain/function should be established, including consideration for discontinuation if benefits do not outweigh risks. Therapy should be continued only if clinically meaningful improvement in pain/function outweighs risks. Therapy should be initiated at the lowest effective dosage using immediate-release opioids (instead of extended-release/long-acting opioids). Risk associated with use increases with higher opioid dosages. Risks and benefits should be re-evaluated when increasing dosage to ≥50 morphine milligram equivalents (MME)/day orally; dosages ≥90 MME/day orally should be avoided unless carefully justified (Dowell [CDC 2016]).
- Optimal regimen: An opioid-containing analgesic regimen should be tailored to each patient's needs and based upon the type of pain being treated (acute versus chronic), the route of administration, degree of tolerance for opioids (naive versus chronic user), age, weight, and patient comorbidities. The optimal analgesic dose varies widely among patients; doses should be titrated to pain relief/prevention.
- REMS program: [US Boxed Warning]: To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, a REMS is required. Drug companies with approved opioid analgesic products must make REMS-compliant education programs available to health care providers. Health care providers are encouraged to complete a REMS-compliant education program; counsel patients and/or their caregivers, with every prescription, on safe use, serious risks, storage, and disposal of these products; emphasize to patients and their caregivers the importance of reading the Medication Guide every time it is provided by their pharmacist; and consider other tools to improve patient, household, and community safety.
- Surgery: Opioids decrease bowel motility; monitor for decreased bowel motility in postop patients receiving opioids. Use with caution in the perioperative setting; individualize treatment when transitioning from parenteral to oral analgesics.
Monitoring Parameters
Pain relief, respiratory and mental status, heart rate, blood pressure; bowel function; signs/symptoms of misuse, abuse, and addiction; signs or symptoms of hypogonadism or hypoadrenalism (Brennan 2013)
Alternate recommendations: Chronic pain (long-term therapy outside of end-of-life or palliative care, active cancer treatment, sickle cell disease, or medication-assisted treatment for opioid use disorder): Evaluate benefits/risks of opioid therapy within 1 to 4 weeks of treatment initiation and with dose increases. Re-evaluate benefits/risks every 3 months during therapy or more frequently in patients at increased risk of overdose or opioid use disorder. Urine drug testing is recommended prior to initiation and re-checking should be considered at least yearly (includes controlled prescription medications and illicit drugs of abuse). State prescription drug monitoring program (PDMP) data should be reviewed by clinicians prior to initiation and periodically during therapy (frequency ranging from every prescription to every 3 months) (Dowell [CDC 2016]).
Pregnancy
Pregnancy Considerations
Opioids cross the placenta.
According to some studies, maternal use of opioids may be associated with birth defects (including neural tube defects, congenital heart defects, and gastroschisis), poor fetal growth, stillbirth, and preterm delivery (CDC [Dowell 2016]).
[US Boxed Warning]: Prolonged use of oxymorphone during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. If chronic opioid exposure occurs in pregnancy, adverse events in the newborn (including withdrawal) may occur (Chou 2009). Symptoms of neonatal abstinence syndrome (NAS) following opioid exposure may be autonomic (eg, fever, temperature instability), gastrointestinal (eg, diarrhea, vomiting, poor feeding/weight gain), or neurologic (eg, high-pitched crying, hyperactivity, increased muscle tone, increased wakefulness/abnormal sleep pattern, irritability, sneezing, seizure, tremor, yawning) (Dow 2012; Hudak 2012). Mothers who are physically dependent on opioids may give birth to infants who are also physically dependent. Opioids may cause respiratory depression and psycho-physiologic effects in the neonate; newborns of mothers receiving opioids during labor should be monitored.
Oxymorphone is not commonly used to treat pain during labor and immediately postpartum (ACOG 209 2019) or chronic noncancer pain in pregnant women or those who may become pregnant (CDC [Dowell 2016]; Chou 2009).
Long-term opioid use may cause secondary hypogonadism, which may lead to sexual dysfunction or infertility in men and women (Brennan 2013).
Patient Education
What is this drug used for?
- It is used to ease pain.
Frequently reported side effects of this drug
- Dry mouth
- Passing gas
- Sweating a lot
- Itching
- Loss of strength and energy
- Tablet shell in stool
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea.
- Adrenal gland problems like severe nausea, vomiting, severe dizziness, passing out, muscle weakness, severe fatigue, mood changes, lack of appetite, or weight loss.
- Severe dizziness
- Passing out
- Trouble breathing
- Slow breathing
- Shallow breathing
- Noisy breathing
- Sexual dysfunction (males)
- Decreased sex drive
- No menstrual periods
- Trouble getting pregnant
- Confusion
- Severe nausea
- Vomiting
- Severe constipation
- Chest pain
- Fast heartbeat
- Slow heartbeat
- Abnormal heartbeat
- Sensing things that seem real but are not
- Mood changes
- Seizures
- Severe abdominal pain
- Severe headache
- Difficult urination
- Swelling
- Vision changes
- Trouble with memory
- Severe fatigue
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.