Boxed Warning
Addiction, abuse, and misuse
Pentazocine/naloxone expose patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient’s risk prior to prescribing pentazocine/naloxone, and monitor all patients regularly for the development of these behaviors or conditions.
Opioid analgesic REMS
To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the FDA has required a REMS for these products. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS-compliant education programs available to health care providers. Health care providers are strongly encouraged to complete a REMS-compliant education program; counsel patients and/or their caregivers, with every prescription, on safe use, serious risks, storage, and disposal of these products; emphasize to patients and their caregivers the importance of reading the Medication Guide every time it is provided by their pharmacist; and consider other tools to improve patient, household, and community safety.
Life-threatening respiratory depression
Serious, life-threatening, or fatal respiratory depression may occur with use of pentazocine/naloxone. Monitor for respiratory depression, especially during initiation of pentazocine and naloxone tablets or following a dose increase.
Accidental ingestion
Accidental ingestion of even one dose of pentazocine/naloxone, especially by children, can result in a fatal overdose of pentazocine.
Neonatal opioid withdrawal syndrome
Prolonged use of pentazocine/naloxone during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available.
Risks from concomitant use with benzodiazepines or other CNS depressants
Concomitant use of opioids with benzodiazepines or other CNS depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of pentazocine/naloxone and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate.
Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
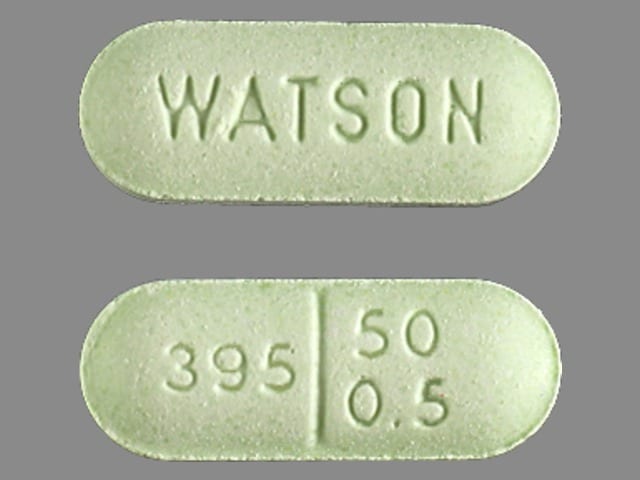
Tablet, oral: Pentazocine 50 mg and naloxone 0.5 mg
Pharmacology
Mechanism of Action
Pentazocine: Agonist of kappa opiate receptors and partial agonist of mu opiate receptors in the CNS, causing inhibition of ascending pain pathways, altering the perception of and response to pain; produces analgesia, respiratory depression and sedation similar to opioids.
Naloxone: Pure opioid antagonist that competes for and displaces opioids at opioid receptor sites in CNS. Lacks pharmacologic activity following oral administration (low dose: 0.5 mg) due to poor systemic absorption. Inhibits the actions of pentazocine when administered parenterally.
Use: Labeled Indications
Pain management: Management of pain severe enough to require an opioid analgesic and for which alternative treatments are inadequate.
Limitations of use: Reserve for use in patients whom alternative treatment options (eg, nonopioid analgesics) are ineffective, not tolerated, or would be otherwise inadequate to provide sufficient management of pain.
Contraindications
Hypersensitivity (eg, anaphylaxis) to pentazocine, naloxone, or any component of the formulation; significant respiratory depression; known or suspected gastrointestinal obstruction, including paralytic ileus; acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment.
Documentation of allergenic cross-reactivity for opioids is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Pain management: Oral: One tablet (pentazocine 50 mg/naloxone 0.5 mg) every 3 to 4 hours; may increase to 2 tablets (pentazocine 100 mg/naloxone 1 mg) if needed. Maximum daily dose: 12 tablets (pentazocine 600 mg/naloxone 6 mg) per day.
Discontinuation of therapy: When discontinuing chronic opioid therapy, the dose should be gradually tapered down. An optimal universal tapering schedule for all patients has not been established (CDC [Dowell 2016]). Proposed schedules range from slow (eg, 10% reductions per week) to rapid (eg, 25% to 50% reduction every few days) (CDC 2015). Tapering schedules should be individualized to minimize opioid withdrawal while considering patient-specific goals and concerns as well as the pharmacokinetics of the opioid being tapered. An even slower taper may be appropriate in patients who have been receiving opioids for a long duration (eg, years), particularly in the final stage of tapering, whereas more rapid tapers may be appropriate in patients experiencing severe adverse events (CDC [Dowell 2016]). Monitor carefully for signs/symptoms of withdrawal. If the patient displays withdrawal symptoms, consider slowing the taper schedule; alterations may include increasing the interval between dose reductions, decreasing amount of daily dose reduction, pausing the taper and restarting when the patient is ready, and/or coadministration of an alpha-2 agonist (eg, clonidine) to blunt withdrawal symptoms (Berna 2015; CDC [Dowell 2016]). Continue to offer nonopioid analgesics as needed for pain management during the taper; consider nonopioid adjunctive treatments for withdrawal symptoms (eg, GI complaints, muscle spasm) as needed (Berna 2015; Sevarino 2018).
Dosing: Geriatric
Refer to adult dosing. Use with caution; may be more sensitive to analgesic and sedative effects; decrease initial dose when appropriate and monitor closely.
Dosing: Pediatric
Pain management: Oral: Children ≥12 years and Adolescents: Refer to adult dosing.
Storage
Store at 20°C to 25°C (68°F to 77°F).
Pentazocine and Naloxone Images
Drug Interactions
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Alvimopan: Opioid Agonists may enhance the adverse/toxic effect of Alvimopan. This is most notable for patients receiving long-term (i.e., more than 7 days) opiates prior to alvimopan initiation. Management: Alvimopan is contraindicated in patients receiving therapeutic doses of opioids for more than 7 consecutive days immediately prior to alvimopan initiation. Consider therapy modification
Amphetamines: May enhance the analgesic effect of Opioid Agonists. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: Opioids (Mixed Agonist / Antagonist) may diminish the therapeutic effect of Buprenorphine. This combination may also induce opioid withdrawal. Avoid combination
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Desmopressin: Opioid Agonists may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Diuretics: Opioid Agonists may enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Eluxadoline: Opioid Agonists may enhance the constipating effect of Eluxadoline. Avoid combination
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Gastrointestinal Agents (Prokinetic): Opioid Agonists may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methylnaltrexone: May enhance the adverse/toxic effect of Opioid Antagonists. Specifically, the risk for opioid withdrawal may be increased. Avoid combination
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Naldemedine: Opioid Antagonists may enhance the adverse/toxic effect of Naldemedine. Specifically, the risk for opioid withdrawal may be increased. Avoid combination
Nalmefene: May diminish the therapeutic effect of Opioid Agonists. Management: Avoid the concomitant use of nalmefene and opioid agonists. Discontinue nalmefene 1 week prior to any anticipated use of opioid agonistss. If combined, larger doses of opioid agonists will likely be required. Consider therapy modification
Naloxegol: Opioid Antagonists may enhance the adverse/toxic effect of Naloxegol. Specifically, the risk for opioid withdrawal may be increased. Avoid combination
Naltrexone: May diminish the therapeutic effect of Opioid Agonists. Management: Seek therapeutic alternatives to opioids. See full drug interaction monograph for detailed recommendations. Consider therapy modification
Opioid Agonists: Opioids (Mixed Agonist / Antagonist) may diminish the analgesic effect of Opioid Agonists. Management: Seek alternatives to mixed agonist/antagonist opioids in patients receiving pure opioid agonists, and monitor for symptoms of therapeutic failure/high dose requirements (or withdrawal in opioid-dependent patients) if patients receive these combinations. Exceptions: Buprenorphine; Butorphanol; Meptazinol; Nalbuphine; Pentazocine. Avoid combination
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pegvisomant: Opioid Agonists may diminish the therapeutic effect of Pegvisomant. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Ramosetron: Opioid Agonists may enhance the constipating effect of Ramosetron. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Serotonergic Agents (High Risk): Opioid Agonists may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Succinylcholine: May enhance the bradycardic effect of Opioid Agonists. Monitor therapy
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Tobacco (Smoked): May decrease the serum concentration of Pentazocine. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
Frequency not defined.
Cardiovascular: Circulatory depression, facial edema, flushing, hypertension, hypotension, syncope, tachycardia
Central nervous system: Central nervous system depression, chills, confusion, disorientation, dizziness, drowsiness, drug dependence, euphoria, excitement, hallucination, headache, increased intracranial pressure, insomnia, irritability, nightmares, paresthesia, sedation, seizure, withdrawal syndrome
Dermatologic: Dermatitis, diaphoresis, erythema multiforme, pruritus, skin rash, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Gastrointestinal: Abdominal distress, anorexia, biliary tract spasm, constipation, diarrhea, nausea, vomiting, xerostomia
Genitourinary: Urinary retention
Hematologic & oncologic: Agranulocytosis (rare), decreased white blood cell count, eosinophilia
Hypersensitivity: Anaphylaxis
Neuromuscular & skeletal: Tremor, weakness
Ophthalmic: Blurred vision, miosis
Otic: Tinnitus
Respiratory: Respiratory depression (rare)
Postmarketing and/or case reports: Hypogonadism (Brennan, 2013; Debono, 2011)
Warnings/Precautions
Concerns related to adverse effects:
- Cardiovascular effects: Pentazocine may increase systemic and pulmonary arterial pressure and systemic vascular resistance; use with caution in patients who may not tolerate these alterations in hemodynamics (eg, acute MI) and in patients with MI who have nausea or vomiting.
- CNS effects: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving). Confusion, disorientation, and visual hallucinations have occurred in some patients, but usually clears within a few hours; observe patients closely.
- Constipation: May cause constipation which may be problematic in patients with unstable angina and patients post-myocardial infarction. Consider preventive measures (eg, stool softener, increased fiber) to reduce the potential for constipation.
- Respiratory depression: [US Boxed Warning]: Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely for respiratory depression, especially during initiation or dose escalation. Carbon dioxide retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids.
Disease-related concerns:
- Abdominal conditions: May obscure diagnosis or clinical course of patients with acute abdominal conditions.
- Adrenal insufficiency: Use with caution in patients with adrenal insufficiency, including Addison disease. Long-term opioid use may cause secondary hypogonadism, which may lead to sexual dysfunction, infertility, mood disorders, and osteoporosis (Brennan 2013).
- Biliary tract impairment: Use with caution in patients with biliary tract dysfunction, including acute pancreatitis; may cause constriction of sphincter of Oddi.
- Bowel disease: Use with caution in patients with inflammatory or obstructive bowel disease.
- CNS depression/coma: Avoid use in patients with CNS depression or coma as these patients are susceptible to intracranial effects of CO2 retention.
- Delirium tremens: Use with caution in patients with delirium tremens.
- Ethanol use: Use with caution due to the potential for increased risk of CNS depressant effects.
- Head trauma: Use with extreme caution in patients with head injury, intracranial lesions, or elevated intracranial pressure; exaggerated elevation of ICP may occur.
- Hepatic impairment: Use with caution in patients with hepatic impairment.
- Mental health conditions: Use opioids with caution for chronic pain in patients with mental health conditions (eg, depression, anxiety disorders, post-traumatic stress disorder) due to increased risk for opioid use disorder and overdose; more frequent monitoring is recommended (Dowell [CDC 2016]).
- Obesity: Use with caution in patients who are morbidly obese.
- Porphyria: Use with caution in patients with a history of porphyria; may exacerbate condition.
- Prostatic hyperplasia/urinary stricture: Use with caution in patients with prostatic hyperplasia and/or urinary stricture.
- Psychosis: Use with caution in patients with toxic psychosis.
- Renal impairment: Use with caution in patients with renal impairment.
- Respiratory disease: Use with caution and monitor for respiratory depression in patients with significant chronic obstructive pulmonary disease or cor pulmonale, and those with a substantially decreased respiratory reserve, hypoxia, hypercapnia, or preexisting respiratory depression, particularly when initiating and titrating therapy; critical respiratory depression may occur, even at therapeutic dosages. Consider the use of alternative nonopioid analgesics in these patients.
- Seizures: Use with caution in patients with a history of seizure disorders; may cause or exacerbate preexisting seizures.
- Sleep-related disorders: Opioid use increases the risk for sleep-related disorders (eg, central sleep apnea [CSA], hypoxemia) in a dose-dependent fashion. Use with caution for chronic pain and titrate dosage cautiously in patients with risk factors for sleep-disordered breathing (eg, heart failure, obesity). Consider dose reduction in patients presenting with CSA. Avoid opioids in patients with moderate to severe sleep-disordered breathing (Dowell [CDC 2016]).
- Thyroid dysfunction: Use with caution in patients with thyroid dysfunction.
Concurrent drug therapy issues:
- Benzodiazepines or other CNS depressants: [US Boxed Warning]: Concomitant use of opioids with benzodiazepines or other CNS depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of pentazocine/naloxone and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate. Limit dosage and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation.
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Cachectic or debilitated patients: Use with caution in cachectic or debilitated patients; there is a greater potential for critical respiratory depression, even at therapeutic dosages. Consider the use of alternative nonopioid analgesics in these patients.
- Elderly: Use with caution in the elderly; may be more sensitive to adverse effects. Decrease initial dose when appropriate. Use opioids for chronic pain with caution in this age group; monitor closely due to an increased potential for risks, including certain risks such as falls/fracture, cognitive impairment, and constipation. Clearance may also be reduced in older adults (with or without renal impairment) resulting in a narrow therapeutic window and increasing the risk for respiratory depression or overdose (Dowell [CDC 2016]). Consider the use of alternative nonopioid analgesics in these patients.
- Neonates: Neonatal withdrawal syndrome: [US Boxed Warning]: Prolonged use of opioids during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure appropriate treatment will be available. Signs and symptoms include irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea, and failure to gain weight. Onset, duration, and severity depend on the drug used, duration of use, maternal dose, and rate of drug elimination by the newborn.
- Smokers: Pentazocine clearance may be increased.
Other warnings/precautions:
- Abrupt discontinuation/withdrawal: Abrupt discontinuation in patients who are physically dependent to opioids has been associated with serious withdrawal symptoms, uncontrolled pain, attempts to find other opioids (including illicit), and suicide. Use a collaborative, patient-specific taper schedule that minimizes the risk of withdrawal, considering factors such as current opioid dose, duration of use, type of pain, and physical and psychological factors. Monitor pain control, withdrawal symptoms, mood changes, suicidal ideation, and for use of other substances and provide care as needed. Concurrent use of mixed agonist/antagonist (eg, pentazocine, nalbuphine, butorphanol) or partial agonist (eg, buprenorphine) analgesics may also precipitate withdrawal symptoms and/or reduced analgesic efficacy in patients following prolonged therapy with mu opioid agonists.
- Abuse/misuse/diversion: [US Boxed Warning]: Use exposes patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient's risk prior to prescribing pentazocine/naloxone, and monitor all patients regularly for the development of these behaviors or conditions. Use with caution in patients with a history of drug abuse, acute alcoholism, or mental illness (eg, major depression); potential for drug dependency exists. Tolerance, psychological, and physical dependence may occur with prolonged use. Other factors associated with increased risk include younger age and psychotropic medication use. Consider offering naloxone prescriptions in patients with factors associated with an increased risk for overdose, such as history of overdose or substance use disorder, higher opioid dosages (≥50 morphine milligram equivalents/day orally), and concomitant benzodiazepine use (Dowell [CDC 2016]).
- Accidental ingestion: [US Boxed Warning]: Accidental ingestion of even one dose of pentazocine/naloxone, especially in children, can result in a fatal overdose of pentazocine.
- Appropriate use: Chronic pain (outside of end-of-life or palliative care, active cancer treatment, sickle cell disease, or medication-assisted treatment for opioid use disorder) in outpatient setting in adults: Opioids should not be used as first-line therapy for chronic pain management (pain >3-month duration or beyond time of normal tissue healing) due to limited short-term benefits, undetermined long-term benefits, and association with serious risks (eg, overdose, MI, auto accidents, risk of developing opioid use disorder). Preferred management includes nonpharmacologic therapy and nonopioid therapy (eg, NSAIDs, acetaminophen, certain anticonvulsants and antidepressants). If opioid therapy is initiated, it should be combined with nonpharmacologic and non-opioid therapy, as appropriate. Prior to initiation, known risks of opioid therapy should be discussed and realistic treatment goals for pain/function should be established, including consideration for discontinuation if benefits do not outweigh risks. Therapy should be continued only if clinically meaningful improvement in pain/function outweighs risks. Therapy should be initiated at the lowest effective dosage using immediate-release opioids (instead of extended-release/long-acting opioids). Risk associated with use increases with higher opioid dosages. Risks and benefits should be re-evaluated when increasing dosage to ≥50 morphine milligram equivalents (MME)/day orally; dosages ≥90 MME/day orally should be avoided unless carefully justified (Dowell [CDC 2016]).
- Optimal regimen: An opioid-containing analgesic regimen should be tailored to each patient's needs and based upon the type of pain being treated (acute versus chronic), the route of administration, degree of tolerance for opioids (naive versus chronic user), age, weight, and medical condition. The optimal analgesic dose varies widely among patients; doses should be titrated to pain relief/prevention.
- Risk Evaluation and Mitigation Strategy (REMS): [US Boxed Warning]: To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the FDA has required a REMS for these products. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS-compliant education programs available to health care providers. Health care providers are strongly encouraged to complete a REMS-compliant education program; counsel patients and/or their caregivers, with every prescription, on safe use, serious risks, storage, and disposal of these products; emphasize to patients and their caregivers the importance of reading the Medication Guide every time it is provided by their pharmacist; and consider other tools to improve patient, household, and community safety.
- Surgery: Opioids decrease bowel motility; monitor for decreased bowel motility in postoperative patients receiving opioids. Patients interrupting therapy to undergo pain-relieving procedures (eg, chordotomy) may require a dosage adjustment when resuming therapy after the postoperative recovery period.
Monitoring Parameters
Pain relief, respiratory (within the first 24 to 72 hours of initiation and following dosage increases) and mental status; blood pressure; bowel function; signs/symptoms of misuse, abuse and addiction; signs or symptoms of hypogonadism or hypoadrenalism (Brennan 2013)
Alternate recommendations: Chronic pain (long-term therapy outside of end-of-life or palliative care, active cancer treatment, sickle cell disease, or medication-assisted treatment for opioid use disorder): Evaluate benefits/risks of opioid therapy within 1 to 4 weeks of treatment initiation and with dose increases. Re-evaluate benefits/risks every 3 months during therapy or more frequently in patients at increased risk of overdose or opioid use disorder. Urine drug testing is recommended prior to initiation and re-checking should be considered at least yearly (includes controlled prescription medications and illicit drugs of abuse). State prescription drug monitoring program (PDMP) data should be reviewed by clinicians prior to initiation and periodically during therapy (frequency ranging from every prescription to every 3 months) (Dowell [CDC 2016]).
Pregnancy
Pregnancy Considerations
[US Boxed Warning]: Prolonged use of opioids during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure appropriate treatment will be available. See individual agents for additional information.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience nausea, vomiting, sweating a lot, diarrhea, dry mouth, abdominal pain, or lack of appetite. Have patient report immediately to prescriber signs of serotonin syndrome (dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea), signs of adrenal gland problems (severe nausea, vomiting, severe dizziness, passing out, muscle weakness, severe fatigue, mood changes, lack of appetite, or weight loss), sexual dysfunction (males), no menstrual periods, decreased sex drive, trouble getting pregnant, severe headache, severe dizziness, passing out, difficulty breathing, slow breathing, shallow breathing, severe fatigue, confusion, severe constipation, severe loss of strength and energy, sensing things that seem real but are not, seizures, chest pain, fast heartbeat, vision changes, difficult urination, mood changes, chills, sore throat, or burning or numbness feeling (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for healthcare professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience and judgment in diagnosing, treating and advising patients.