Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Elixir, Oral:
Generic: 20 mg/5 mL (473 mL)
Solution, Oral:
Generic: 20 mg/5 mL (473 mL)
Solution, Injection, as sodium:
Generic: 65 mg/mL (1 mL); 130 mg/mL (1 mL)
Tablet, Oral:
Generic: 15 mg, 16.2 mg, 30 mg, 32.4 mg, 60 mg, 64.8 mg, 97.2 mg, 100 mg
Pharmacology
Mechanism of Action
Long-acting barbiturate with sedative, hypnotic, and anticonvulsant properties. Barbiturates depress the sensory cortex, decrease motor activity, alter cerebellar function, and produce drowsiness, sedation, and hypnosis. In high doses, barbiturates exhibit anticonvulsant activity; barbiturates produce dose-dependent respiratory depression.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Rapid
Distribution
0.61 L/kg (Patsalos 2018).
Metabolism
Hepatic by oxidation via CYP2C9 and to a lesser extent via CYP2C19 and CYP2E1, and by N-glucosidation (Patsalos 2018).
Excretion
Urine (25% to 50% as unchanged drug); feces (minimal)
Onset of Action
Oral: ≥60 minutes; IV: 5 minutes; Peak effect: IV: CNS depression: ≥15 minutes
Time to Peak
Serum: Oral: 2 to 4 hours (Patsalos 2018).
Duration of Action
Oral: 10 to 12 hours; IV: >6 hours
Half-Life Elimination
Neonates (<48 hours old), Infants, and Children: ~110 hours (60 to 180 hours); Adults: ~79 hours (range: 53 to 118 hours)
Protein Binding
48% (Patsalos 2018).
Use: Labeled Indications
Sedation: Use as a sedative
Seizures: Management of generalized tonic-clonic, status epilepticus, and partial seizures
Use: Off Label
Alcohol withdrawalc
Data from a limited number of patients studied in randomized, double-blind and open-label trials suggest that oral and IV phenobarbital may be beneficial for the treatment of alcohol withdrawal Hendey 2011, Mariani 2006, Rosenson 2013, Rosenthal 1998. Additional data may be necessary to further define the role of phenobarbital in this condition.
Sedative/hypnotic withdrawalc
Data from a limited number of patients in a randomized, double-blind controlled trial, a comparative controlled study, and a retrospective review suggest that phenobarbital may be beneficial for sedative/hypnotic withdrawal Kawasaki 2012, Perry 1981, Sullivan 1993. Additional data may be necessary to further define the role of phenobarbital in this condition.
Contraindications
Hypersensitivity to phenobarbital, barbiturates or any component of the formulation; marked hepatic impairment; dyspnea or airway obstruction; porphyria (manifest and latent); intra-arterial administration, subcutaneous administration (not recommended); use in patients with a history of sedative/hypnotic addiction; nephritic patients (large doses)
Additional contraindications: IV only: Intra-arterial or subcutaneous administration; use in patients with a history of sedative/hypnotic addiction; nephritic patients (large doses)
Dosage and Administration
Dosing: Adult
Sedation:
Oral, IV, IM: 30 to 120 mg/day in 2 to 3 divided doses; maximum: 400 mg/day
Preoperative sedation: IM: 100 to 200 mg 60 to 90 minutes before surgery
Status epilepticus: IV:
American Epilepsy Society recommendations: 15 mg/kg as a single dose. Note: AES recommends phenobarbital as a second line option only if first line options (lorazepam, diazepam, or midazolam) or other second line options (eg, fosphenytoin, valproic acid, levetiracetam) are unavailable (AES [Glauser 2016]).
Neurocritical Care Society recommendation: 20 mg/kg (infused at 50 to 100 mg/minute); if necessary, may repeat once after 10 minutes with an additional 5 to 10 mg/kg (NCS [Brophy 2012])
Note: Additional respiratory support may be required particularly when maximizing loading dose or if concurrent sedative therapy. Repeat doses administered sooner than 10 to 15 minutes may not allow adequate time for peak CNS concentrations to be achieved and may lead to CNS depression.
Seizures: Maintenance dose:
Oral, IV: Usual dosage range (limited data available): 2 mg/kg/day in divided doses (Murphy 2010; Winter 2010). Note: Dosage should be individualized based upon clinical response and serum concentration; 2 mg/kg/day typically produces a steady-state level of 20 mg/L (Winter 2010).
Manufacturer's labeling: Oral: Dosing in the prescribing information may not reflect current clinical practice. 60 to 200 mg/day or 50 to 100 mg 2 to 3 times daily.
Alcohol withdrawal (off-label use):
IV: Initial dose of 260 mg, followed by subsequent doses of 130 mg as needed. Note: Clinical Institute Withdrawal Assessment (CIWA) scores were evaluated at 30 minute intervals in the clinical trial (Hendey 2011).
Oral: Fixed dose regimen of 60 mg 4 times daily on day 1, followed by 60 mg 3 times daily on day 2, 60 mg twice daily on day 3, and 30 mg twice daily on day 4. In addition, provide 60 mg as needed for breakthrough withdrawal symptoms (Mariani 2006; Rosenthal 1998). May also administer 130 mg IM as needed for more substantial withdrawal symptoms (eg, heart rate >120 bpm, SBP >150 mm Hg, marked agitation) (Rosenthal 1998).
Sedative/hypnotic withdrawal (off-label use): Several regimens have been evaluated:
Taper following dosage conversion: Initial daily requirement is determined by substituting phenobarbital in an equivalent dose to the baseline medication (clonazepam 1 mg = phenobarbital 60 mg was used in the study). Divided the calculated baseline total dose into 4 doses and administer every 6 hours for 2 days; then decrease the daily requirement by 10% per day over the next 10 days (Sullivan 1993).
Fixed dose taper: Initial 200 mg, followed by 100 mg every 4 hours for 5 doses, 60 mg every 4 hours for 4 doses, and then 60 mg every 8 hours for 3 doses (Kawasaki 2012).
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Dosing: Pediatric
Status epilepticus: Infants, Children, and Adolescents: IV: Initial: 15-20 mg/kg; maximum dose: 1000 mg; may repeat once after 10-15 minutes if needed; maximum total dose: 40 mg/kg; repeat doses administered sooner than 10-15 minutes may not allow adequate time for peak CNS concentrations to be achieved and may lead to CNS depression (Brophy, 2012; Hegenbarth, 2008). Note: Additional respiratory support may be required particularly when maximizing loading dose or if concurrent sedative therapy.
Seizures, maintenance therapy: Note: Maintenance dose usually starts 12 hours after loading dose:
Manufacturer's labeling: Infants, Children, and Adolescents: Oral: 3-6 mg/kg/day
Alternate dosing: Limited data available (Geurinni, 2006; Kliegman, 2011):
Initial: Oral, IV:
Infants and Children ≤5 years: 3-5 mg/kg/day in 1-2 divided doses
Children >5 years: 2-3 mg/kg/day in 1-2 divided doses
Adolescents: 1-3 mg/kg/day in 1-2 divided doses (Nelson, 1996)
Usual dosing range: Note: Dosage should be individualized based upon clinical response and serum concentration; once daily doses usually administered at bedtime in children and adolescents. Some centers have used:
Infants: 5-6 mg/kg/day in 1-2 divided doses
Children:
1-5 years: 6-8 mg/kg/day in 1-2 divided doses
5-12 years: 4-6 mg/kg/day in 1-2 divided doses
Adolescents: 1-3 mg/kg/day in 1-2 divided doses
Sedation: Note: Newer, shorter-acting agents may be preferable.
Manufacturer's labeling: Children and Adolescents: Oral: 2 mg/kg/dose 3 times daily; maximum dose: 40 mg
Alternate dosing: Limited data available: Infants and Children: IM, Oral: 2-3 mg/kg/day in divided doses every 8-12 hours (Nelson, 1996)
Insomnia (hypnotic): Limited data available; shorter-acting agents may be preferable: Infants and Children: IM, Oral: 2-3 mg/kg/dose; may repeat dose as needed after 12-24 hours (Nelson, 1996); some centers have used: IM, IV: 3-5 mg/kg at bedtime
Hyperbilirubinemia: Limited data available: Infants and Children: Oral: Usual range: 3-8 mg/kg/day in 2-3 divided doses; doses up to 10 mg/kg/day in divided doses have been used in case reports (Cies, 2007; Nelson, 1996); for the treatment of hyperbilirubinemia in Crigler-Najjar Syndrome, a dose of 5 mg/kg/day has been used to reduce serum bilirubin concentrations (Kliegman, 2011); not recommended for management of biliary cirrohisis due to sedation and other adverse effects (Lindor-AASLD, 2009)
Sedative/hypnotic withdrawal; prevention; conversion of PENTobarbital to PHENobarbital (PENTobarbital infusion, a total cumulative PENTobarbital dose ≥25 mg/kg or duration ≥5-7 days): Limited data available: Infants, Children, and Adolescents: The following approach transitioning from PENTobarbital to PHENobarbital has been described: Discontinue PENTobarbital infusion, administer half of the PHENobarbital IV loading dose (see table) over 1 hour followed 6 hours later by the remaining half of PHENobarbital loading dose IV (over 1 hour). Begin IV maintenance PHENobarbital dose 6 hours after loading dose completed; the maintenance PHENobarbital dose should be 1/3 of the initial loading dose and given every 12 hours. Once patient is stabilized, may switch to oral therapy and begin tapering 10% to 20% weekly (Tobias, 2000; Tobias, 2000a). Note: This conversion method is based on preliminary data in mechanically ventilated patients. Closely monitor respiratory status and evaluate patient for withdrawal symptoms.
|
PENTobarbital Infusion Rate (mg/kg/hour) |
PHENobarbital IV Loading Dose (mg/kg) |
|---|---|
|
1 to 2 |
8 |
|
2 to 3 |
15 |
|
3 to 4 |
20 |
PENTobarbital Infusion Rate 1 to 2 mg/kg/hour: PHENobarbital IV Loading Dose 8 mg/kg
PENTobarbital Infusion Rate 2 to 3 mg/kg/hour: PHENobarbital IV Loading Dose 15 mg/kg
PENTobarbital Infusion Rate 3 to 4 mg/kg/hour; PHENobarbital IV Loading Dose 20 mg/kg
Extemporaneously Prepared
An alcohol-free 10 mg/mL phenobarbital oral suspension may be made from tablets and one of two different vehicles (a 1:1 mixture of Ora-Plus and Ora-Sweet or a 1:1 mixture of Ora-Plus and Ora-Sweet SF). Crush ten phenobarbital 60 mg tablets in a glass mortar and reduce to a fine powder. Mix 30 mL of Ora-Plus and 30 mL of either Ora-Sweet or Ora-Sweet SF; stir vigorously. Add 15 mL of the vehicle to the powder and mix to a uniform paste. Transfer the mixture to a 2 ounce amber plastic prescription bottle. Rinse mortar and pestle with 15 mL of the vehicle; transfer to bottle. Repeat, then add quantity of vehicle sufficient to make 60 mL. Label "shake well." May mix dose with chocolate syrup (1:1 volume) immediately before administration to mask the bitter aftertaste. Stable for 115 days when stored in amber plastic prescription bottles at room temperature.
Cober M and Johnson CE, “Stability of an Extemporaneously Prepared Alcohol-Free Phenobarbital Suspension,” Am J Health Syst Pharm, 2007, 64(6):644-6.17353574
Administration
May be administered IV, IM, or orally.
According to the manufacturer, rapid IV administration >60 mg/minute should be avoided. In the setting of status epilepticus, the Neurocritical Care Society recommends administration at a rate of 50 to 100 mg/minute (NCS [Brophy 2012]). Avoid extravasation. Intra-arterial injection is contraindicated. Avoid subcutaneous administration.
For IM administration, inject deep into muscle. Do not exceed 5 mL per injection site due to potential for tissue irritation
Dietary Considerations
Folate and vitamin B: Phenobarbital use has been associated with low serum concentrations of folate, vitamin B2 (riboflavin), B6 (pyridoxine) and B12 (cyanocobalamin), which may contribute to hyperhomocysteinemia. Hyperhomocysteinemia may contribute to cardiovascular disease, venous thromboembolic disease, dementia, neuropsychiatric symptoms and poor seizure control. Some clinicians recommend administering folic acid, riboflavin, pyridoxine and cyanocobalamin supplements in patients taking phenobarbital (Apeland 2003; Apeland 2008; Belcastro 2012; Bochyńska 2012).
Vitamin D and calcium: Phenobarbital increases the hepatic metabolism of vitamin D to inactive compounds and reduces calcium absorption (Gough 1986); increase intake of foods rich in vitamin D. Supplementation of vitamin D and/or calcium may be necessary.
Injection may contain sodium.
Storage
Oral: Store between 20°C and 25°C (68°F and 77°F). Protect from light.
Injection: Store between 20°C and 25°C (68°F and 77°F); excursions are permitted to 15°C to 30°C (59°F to 86°F).
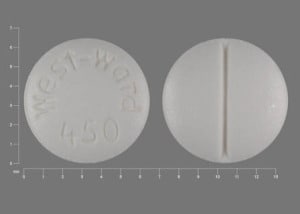
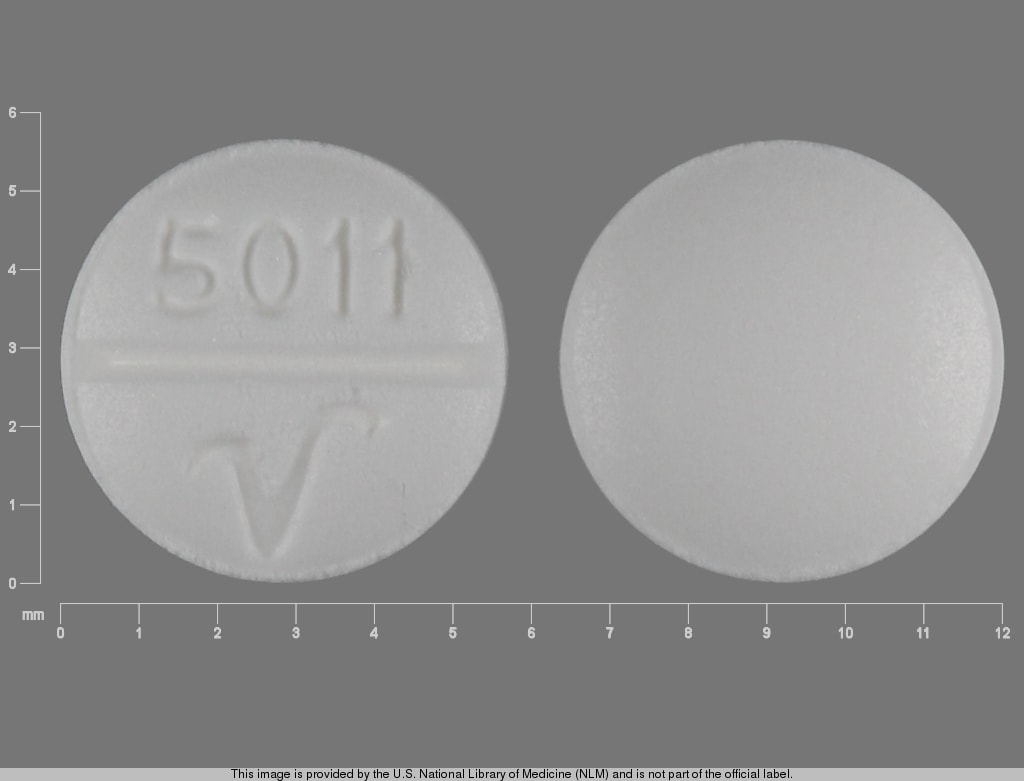
PHENobarbital Images
Drug Interactions
Abemaciclib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Abemaciclib. Avoid combination
Abiraterone Acetate: CYP3A4 Inducers (Strong) may decrease the serum concentration of Abiraterone Acetate. Management: Avoid whenever possible. If such a combination cannot be avoided, increase abiraterone acetate dosing frequency from once daily to twice daily during concomitant use. Consider therapy modification
Acalabrutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Acalabrutinib. Management: Avoid co-administration of strong CYP3A inducers in patients taking acalabrutinib. If strong CYP3A inducers cannot be avoided, increase the dose of acalabrutinib to 200 mg twice daily. Consider therapy modification
Acetaminophen: Barbiturates may increase the metabolism of Acetaminophen. This may 1) diminish the effect of acetaminophen; and 2) increase the risk of liver damage. Monitor therapy
Afatinib: PHENobarbital may decrease the serum concentration of Afatinib. Management: Per US labeling: if requiring chronic use of phenobarbital, increase afatinib dose by 10 mg as tolerated; reduce to original afatinib dose 2-3 days after stopping phenobarbital. Per Canadian labeling: avoid combination if possible. Consider therapy modification
Albendazole: PHENobarbital may decrease serum concentrations of the active metabolite(s) of Albendazole. Monitor therapy
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Alpelisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Alpelisib. Avoid combination
Amphetamines: May decrease the serum concentration of PHENobarbital. Monitor therapy
Antihepaciviral Combination Products: CYP3A4 Inducers (Strong) may decrease the serum concentration of Antihepaciviral Combination Products. Avoid combination
Apixaban: CYP3A4 Inducers (Strong) may decrease the serum concentration of Apixaban. Management: Avoid concurrent use of apixaban with strong CYP3A4 inducers whenever possible. Use of a strong CYP3A4 inducer with apixaban should be strictly avoided in any patient who is using an agent (either the CYP3A4 inducer or a third drug) that induces P-gp. Consider therapy modification
Apremilast: CYP3A4 Inducers (Strong) may decrease the serum concentration of Apremilast. Avoid combination
Aprepitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Aprepitant. Avoid combination
ARIPiprazole: CYP3A4 Inducers (Strong) may decrease the serum concentration of ARIPiprazole. Management: Double the oral aripiprazole dose and closely monitor. Reduce oral aripiprazole dose to 10-15 mg/day (for adults) if the inducer is discontinued. Avoid use of strong CYP3A4 inducers for more than 14 days with extended-release injectable aripiprazole. Consider therapy modification
ARIPiprazole Lauroxil: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of ARIPiprazole Lauroxil. Management: Patients taking the 441 mg dose of aripiprazole lauroxil increase their dose to 662 mg if used with a strong CYP3A4 inducer for more than 14 days. No dose adjustment is necessary for patients using the higher doses of aripiprazole lauroxil. Consider therapy modification
Artemether: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Artemether. Specifically, dihydroartemisinin concentrations may be reduced. CYP3A4 Inducers (Strong) may decrease the serum concentration of Artemether. Avoid combination
Asunaprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Asunaprevir. Avoid combination
Avapritinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Avapritinib. Avoid combination
Axitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Axitinib. Avoid combination
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Bazedoxifene: PHENobarbital may decrease the serum concentration of Bazedoxifene. This may lead to loss of efficacy or, if bazedoxifene is combined with estrogen therapy, an increased risk of endometrial hyperplasia. Monitor therapy
Bedaquiline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Bedaquiline. Avoid combination
Benperidol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Benperidol. Monitor therapy
Benzhydrocodone: PHENobarbital may enhance the CNS depressant effect of Benzhydrocodone. PHENobarbital may decrease serum concentrations of the active metabolite(s) of Benzhydrocodone. Specifically, phenobarbital may decrease serum concentrations of hydrocodone. Management: Avoid use of benzhydrocodone and phenobarbital when possible. Monitor for respiratory depression/sedation. Because phenobarbital is also a strong CYP3A4 inducer, monitor for decreased benzhydrocodone efficacy and withdrawal if combined. Consider therapy modification
Beta-Blockers: Barbiturates may decrease the serum concentration of Beta-Blockers. Exceptions: Atenolol; Levobunolol; Metipranolol; Nadolol. Monitor therapy
Bictegravir: PHENobarbital may decrease the serum concentration of Bictegravir. Management: When possible consider using an alternative anticonvulsant with concurrent bictegravir, emtricitabine, and tenofovir alafenamide. If the combination must be used, monitor closely for evidence of reduced antiviral effectiveness. Consider therapy modification
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Blood Pressure Lowering Agents: Barbiturates may enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bortezomib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Bortezomib. Avoid combination
Bosutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Bosutinib. Avoid combination
Brentuximab Vedotin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be decreased. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brexpiprazole: CYP3A4 Inducers (Strong) may decrease the serum concentration of Brexpiprazole. Management: If brexpiprazole is used together with a strong CYP3A4 inducer, the brexpiprazole dose should gradually be doubled over the course of 1 to 2 weeks. Consider therapy modification
Brigatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Brigatinib. Avoid combination
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: PHENobarbital may enhance the CNS depressant effect of Buprenorphine. PHENobarbital may decrease the serum concentration of Buprenorphine. Management: Avoid use of buprenorphine and phenobarbital when possible. Monitor for respiratory depression/sedation. Because phenobarbital is also a strong CYP3A4 inducer, monitor for decreased buprenorphine efficacy and withdrawal if combined. Consider therapy modification
BusPIRone: CYP3A4 Inducers (Strong) may decrease the serum concentration of BusPIRone. Management: Consider alternatives to this combination. If coadministration of these agents is deemed necessary, monitor patients for reduced buspirone effects and increase buspirone doses as needed. Consider therapy modification
Cabozantinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cabozantinib. Management: Avoid use of strong CYP3A4 inducers with cabozantinib if possible. If combined, cabozantinib dose adjustments are recommended and vary based on the cabozantinib product used and the indication for use. See monograph for details. Consider therapy modification
Calcifediol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Calcifediol. Monitor therapy
Calcium Channel Blockers: Barbiturates may increase the metabolism of Calcium Channel Blockers. Management: Monitor for decreased therapeutic effects of calcium channel blockers with concomitant barbiturate therapy. Calcium channel blocker dose adjustments may be necessary. Nimodipine Canadian labeling contraindicates concomitant use with phenobarbital. Exceptions: Clevidipine. Monitor therapy
Canagliflozin: PHENobarbital may decrease the serum concentration of Canagliflozin. Management: Consider increasing canagliflozin dose to 200 mg/day in patients tolerating 100 mg/day. A further increase to 300 mg/day can be considered in patients with an estimated glomerular filtration rate (GFR) of 60 mL/min/1.73 m2 or greater. Consider therapy modification
Cannabidiol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cannabidiol. Monitor therapy
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cannabis. More specifically, tetrahydrocannabinol and cannabidiol serum concentrations may be decreased. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
CarBAMazepine: CYP3A4 Inducers (Strong) may decrease the serum concentration of CarBAMazepine. Monitor therapy
Cariprazine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cariprazine. Avoid combination
Cenobamate: May increase the serum concentration of PHENobarbital. Monitor therapy
Ceritinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ceritinib. Avoid combination
Chloramphenicol (Systemic): May decrease the metabolism of Barbiturates. Barbiturates may increase the metabolism of Chloramphenicol (Systemic). Consider therapy modification
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
ChlorproPAMIDE: CYP3A4 Inducers (Strong) may decrease the serum concentration of ChlorproPAMIDE. Monitor therapy
Cholestyramine Resin: May decrease the serum concentration of PHENobarbital. Management: Administer phenobarbital at least 1 hour before or 4-6 hours after administration of cholestyramine in order to minimize the risk for any significant interaction. Consider therapy modification
Clarithromycin: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Clarithromycin. Clarithromycin may increase the serum concentration of CYP3A4 Inducers (Strong). CYP3A4 Inducers (Strong) may decrease the serum concentration of Clarithromycin. Management: Consider alternative antimicrobial therapy for patients receiving a CYP3A inducer. Drugs that enhance the metabolism of clarithromycin into 14-hydroxyclarithromycin may alter the clinical activity of clarithromycin and may impair clarithromycin efficacy. Consider therapy modification
Clindamycin (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Clindamycin (Systemic). Refer to the specific clindamycin (systemic) - rifampin drug interaction monograph for information concerning that combination. Monitor therapy
CloZAPine: CYP3A4 Inducers (Strong) may decrease the serum concentration of CloZAPine. Avoid combination
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Cobicistat: PHENobarbital may decrease the serum concentration of Cobicistat. Avoid combination
Cobimetinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cobimetinib. Avoid combination
Codeine: PHENobarbital may enhance the CNS depressant effect of Codeine. PHENobarbital may decrease the serum concentration of Codeine. Management: Avoid use of codeine and phenobarbital when possible. Monitor for respiratory depression/sedation. Because phenobarbital is also a strong CYP3A4 inducer, monitor for decreased codeine efficacy and withdrawal if combined. Consider therapy modification
Copanlisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Copanlisib. Avoid combination
Corticosteroids (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Corticosteroids (Systemic). Exceptions: Hydrocortisone (Systemic); PrednisoLONE (Systemic); PredniSONE. Monitor therapy
Cosyntropin: May enhance the hepatotoxic effect of PHENobarbital. Monitor therapy
Crizotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Crizotinib. Avoid combination
CycloSPORINE (Systemic): Barbiturates may increase the metabolism of CycloSPORINE (Systemic). Consider therapy modification
CYP2C19 Inducers (Moderate): May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
CYP2C19 Inducers (Strong): May increase the metabolism of CYP2C19 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP2C19 Inhibitors (Moderate): May decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Monitor therapy
CYP2C19 Inhibitors (Strong): May decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Consider therapy modification
CYP3A4 Substrates (High risk with Inducers): CYP3A4 Inducers (Strong) may increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Exceptions: Benzhydrocodone; Buprenorphine; CarBAMazepine; Etizolam; HYDROcodone; Mirtazapine; TraMADol; Zolpidem. Consider therapy modification
Dabigatran Etexilate: PHENobarbital may decrease the serum concentration of Dabigatran Etexilate. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C19 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Daclatasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Daclatasvir. Avoid combination
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Darunavir: May decrease the serum concentration of PHENobarbital. Monitor therapy
Dasabuvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dasabuvir. Avoid combination
Dasatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dasatinib. Management: Avoid when possible. If such a combination cannot be avoided, consider increasing dasatinib dose and monitor clinical response and toxicity closely. Consider therapy modification
Deferasirox: PHENobarbital may decrease the serum concentration of Deferasirox. Management: Avoid combination when possible; if the combination must be used, consider a 50% increase in initial deferasirox dose, with monitoring of serum ferritin concentrations and clinical responses to guide further dosing. Consider therapy modification
Deflazacort: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Deflazacort. Avoid combination
Delamanid: CYP3A4 Inducers (Strong) may decrease the serum concentration of Delamanid. Avoid combination
DexAMETHasone (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of DexAMETHasone (Systemic). Management: Consider dexamethasone dose increases in patients receiving strong CYP3A4 inducers and monitor closely for reduced dexamethasone efficacy. Consider avoiding this combination when treating life threatening conditions (ie, multiple myeloma). Consider therapy modification
Dexmethylphenidate: May increase the serum concentration of PHENobarbital. Monitor therapy
Dienogest: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dienogest. Management: Avoid use of dienogest for contraception when using medications that induce CYP3A4 and for at least 28 days after discontinuation of a CYP3A4 inducer. An alternative form of contraception should be used during this time. Avoid combination
Diethylstilbestrol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Diethylstilbestrol. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Disopyramide: PHENobarbital may decrease the serum concentration of Disopyramide. Monitor therapy
Dolutegravir: PHENobarbital may decrease the serum concentration of Dolutegravir. Avoid combination
Doravirine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Doravirine. Avoid combination
Doxercalciferol: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Doxercalciferol. Monitor therapy
DOXOrubicin (Conventional): CYP3A4 Inducers (Strong) may decrease the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to strong CYP3A4 inducers in patients treated with doxorubicin. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Doxycycline: Barbiturates may decrease the serum concentration of Doxycycline. Consider therapy modification
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dronabinol. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Dronedarone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dronedarone. Avoid combination
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Duvelisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Duvelisib. Avoid combination
Elagolix: CYP3A4 Inducers (Strong) may decrease the serum concentration of Elagolix. Monitor therapy
Elbasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Elbasvir. Avoid combination
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Avoid combination
Eliglustat: CYP3A4 Inducers (Strong) may decrease the serum concentration of Eliglustat. Avoid combination
Elvitegravir: PHENobarbital may decrease the serum concentration of Elvitegravir. Avoid combination
Encorafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Encorafenib. Avoid combination
Enfortumab Vedotin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Enfortumab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be decreased. Monitor therapy
Entrectinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Entrectinib. Avoid combination
Enzalutamide: CYP3A4 Inducers (Strong) may decrease the serum concentration of Enzalutamide. Management: Consider using an alternative agent that has no or minimal CYP3A4 induction potential when possible. If this combination cannot be avoided, increase the dose of enzalutamide from 160 mg daily to 240 mg daily. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Conversely, concentrations of active metabolites may be increased for those drugs activated by CYP2C19. Management: Concurrent use of enzalutamide with CYP2C19 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C19 substrate should be performed with caution and close monitoring. Consider therapy modification
Eravacycline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Eravacycline. Management: Increase the eravacycline dose to 1.5 mg/kg every 12 hours when combined with strong CYP3A4 inducers. Consider therapy modification
Erdafitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Erdafitinib. Avoid combination
Erlotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Erlotinib. Management: Avoid combination if possible. If combination must be used, increase erlotinib dose by 50 mg increments every 2 weeks as tolerated, to a maximum of 450 mg/day. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Eslicarbazepine: PHENobarbital may decrease the serum concentration of Eslicarbazepine. Monitor therapy
Estriol (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Estriol (Systemic). Monitor therapy
Estriol (Topical): CYP3A4 Inducers (Strong) may decrease the serum concentration of Estriol (Topical). Monitor therapy
Estrogen Derivatives (Contraceptive): Barbiturates may diminish the therapeutic effect of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of a non-hormonal contraceptive is recommended. Consider therapy modification
Etizolam: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etizolam. Monitor therapy
Etoposide: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etoposide. Management: When possible, seek alternatives to strong CYP3A4-inducing medications in patients receiving etoposide. If combined, monitor patients closely for diminished etoposide response and need for etoposide dose increases. Consider therapy modification
Etoposide Phosphate: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etoposide Phosphate. Management: When possible, seek alternatives to strong CYP3A4-inducing medications in patients receiving etoposide phosphate. If these combinations cannot be avoided, monitor patients closely for diminished etoposide phosphate response. Consider therapy modification
Etravirine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etravirine. Avoid combination
Everolimus: CYP3A4 Inducers (Strong) may decrease the serum concentration of Everolimus. Management: Avoid concurrent use of strong CYP3A4 inducers if possible. If coadministration cannot be avoided, double the daily dose of everolimus using increments of 5 mg or less. Monitor everolimus serum concentrations closely when indicated. Consider therapy modification
Evogliptin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Evogliptin. Monitor therapy
Exemestane: CYP3A4 Inducers (Strong) may decrease the serum concentration of Exemestane. Management: Exemestane U.S. product labeling recommends using an increased dose (50 mg/day) in patients receiving concurrent strong CYP3A4 inducers. The Canadian product labeling does not recommend a dose adjustment with concurrent use of strong CYP3A4 inducers. Consider therapy modification
Fedratinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Fedratinib. Avoid combination
Felbamate: PHENobarbital may decrease the serum concentration of Felbamate. Felbamate may increase the serum concentration of PHENobarbital. Management: In patients receiving phenobarbital, initiate felbamate at 1200 mg/day in divided doses 3-4 times daily and reduce phenobarbital dose by 20%. Monitor for increased phenobarbital concentrations/effects and decreased felbamate concentrations/effects. Consider therapy modification
FentaNYL: PHENobarbital may enhance the CNS depressant effect of FentaNYL. PHENobarbital may decrease the serum concentration of FentaNYL. Management: Avoid use of fentanyl and phenobarbital when possible. Monitor for respiratory depression/sedation. Because phenobarbital is also a strong CYP3A4 inducer, monitor for decreased fentanyl efficacy and withdrawal if combined. Consider therapy modification
Fexinidazole [INT]: May increase the serum concentration of Products Containing Propylene Glycol. Avoid combination
Flibanserin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Flibanserin. Avoid combination
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Folic Acid: May decrease the serum concentration of PHENobarbital. Monitor therapy
Fosaprepitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Fosaprepitant. Specifically, CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite aprepitant. Avoid combination
Fosnetupitant: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Fosnetupitant. Avoid combination
Fosphenytoin: May enhance the CNS depressant effect of PHENobarbital. Fosphenytoin may increase the serum concentration of PHENobarbital. PHENobarbital may decrease the serum concentration of Fosphenytoin. Monitor therapy
Fostamatinib: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Fostamatinib. Avoid combination
Gefitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Gefitinib. Management: In the absence of severe adverse reactions, increase gefitinib dose to 500 mg daily in patients receiving strong CYP3A4 inducers; resume 250 mg dose 7 days after discontinuation of the strong inducer. Carefully monitor clinical response. Consider therapy modification
Gemigliptin: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Gemigliptin. CYP3A4 Inducers (Strong) may decrease the serum concentration of Gemigliptin. Avoid combination
Gestrinone: PHENobarbital may decrease the serum concentration of Gestrinone. Monitor therapy
Glasdegib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Glasdegib. Avoid combination
Glecaprevir and Pibrentasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Glecaprevir and Pibrentasvir. Monitor therapy
Grazoprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Grazoprevir. Avoid combination
Griseofulvin: Barbiturates may decrease the serum concentration of Griseofulvin. Monitor therapy
GuanFACINE: CYP3A4 Inducers (Strong) may decrease the serum concentration of GuanFACINE. Management: Increase the guanfacine dose by up to double when initiating guanfacine in a patient taking a strong CYP3A4 inducer. Increase guanfacine dose gradually over 1 to 2 weeks if initiating strong CYP3A4 inducer therapy in a patient already taking guanfacine. Consider therapy modification
Hemin: Barbiturates may diminish the therapeutic effect of Hemin. Avoid combination
HYDROcodone: PHENobarbital may enhance the CNS depressant effect of HYDROcodone. PHENobarbital may decrease the serum concentration of HYDROcodone. Management: Avoid use of hydrocodone and phenobarbital when possible. Monitor for respiratory depression/sedation. Because phenobarbital is also a strong CYP3A4 inducer, monitor for decreased hydrocodone efficacy and withdrawal if combined. Consider therapy modification
Hydrocortisone (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Hydrocortisone (Systemic). Monitor therapy
HydrOXYzine: May enhance the CNS depressant effect of Barbiturates. Management: Consider a decrease in the barbiturate dose, as appropriate, when used together with hydroxyzine. With concurrent use, monitor patients closely for excessive response to the combination. Consider therapy modification
Ibrutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ibrutinib. Avoid combination
Idelalisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Idelalisib. Avoid combination
Ifosfamide: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Ifosfamide. CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Imatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Imatinib. Management: Avoid concurrent use of imatinib with strong CYP3A4 inducers when possible. If such a combination must be used, increase imatinib dose by at least 50% and monitor the patient's clinical response closely. Consider therapy modification
Irinotecan Products: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Irinotecan Products. Specifically, serum concentrations of SN-38 may be reduced. CYP3A4 Inducers (Strong) may decrease the serum concentration of Irinotecan Products. Avoid combination
Isavuconazonium Sulfate: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Isavuconazonium Sulfate. Specifically, CYP3A4 Inducers (Strong) may decrease isavuconazole serum concentrations. Avoid combination
Istradefylline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Istradefylline. Avoid combination
Itraconazole: CYP3A4 Inducers (Strong) may decrease the serum concentration of Itraconazole. Avoid combination
Ivabradine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ivabradine. Avoid combination
Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ivacaftor. Avoid combination
Ivosidenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ivosidenib. Avoid combination
Ixabepilone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ixabepilone. Management: Avoid this combination whenever possible. If this combination must be used, a gradual increase in ixabepilone dose from 40 mg/m2 to 60 mg/m2 (given as a 4-hour infusion), as tolerated, should be considered. Consider therapy modification
Ixazomib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ixazomib. Avoid combination
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
LamoTRIgine: Barbiturates may decrease the serum concentration of LamoTRIgine. Management: See lamotrigine prescribing information for specific age-dependent dosing guidelines regarding concurrent use with a barbiturate, as well as for adjusting lamotrigine dosing if concurrent barbiturate therapy is discontinued. Consider therapy modification
Lapatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lapatinib. Management: If therapy overlap cannot be avoided, consider titrating lapatinib gradually from 1,250 mg/day up to 4,500 mg/day (HER2 positive metastatic breast cancer) or 1,500 mg/day up to 5,500 mg/day (hormone receptor/HER2 positive breast cancer) as tolerated. Avoid combination
Larotrectinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Larotrectinib. Management: Avoid use of strong CYP3A4 inducers with larotrectinib. If this combination cannot be avoided, double the larotrectinib dose. Reduced to previous dose after stopping the inducer after a period of 3 to 5 times the inducer half-life. Consider therapy modification
Ledipasvir: PHENobarbital may decrease the serum concentration of Ledipasvir. Avoid combination
Lefamulin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin with strong CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin (Intravenous): CYP3A4 Inducers (Strong) may decrease the serum concentration of Lefamulin (Intravenous). Management: Avoid concomitant use of lefamulin intravenous infusion with strong CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lemborexant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lemborexant. Avoid combination
Letermovir: May increase the serum concentration of UGT1A1 Inducers. Avoid combination
Leucovorin Calcium-Levoleucovorin: May decrease the serum concentration of PHENobarbital. Monitor therapy
LevETIRAcetam: PHENobarbital may decrease the serum concentration of LevETIRAcetam. Monitor therapy
Levomefolate: May decrease the serum concentration of PHENobarbital. Monitor therapy
Levomethadone: PHENobarbital may decrease the serum concentration of Levomethadone. Monitor therapy
LinaGLIPtin: CYP3A4 Inducers (Strong) may decrease the serum concentration of LinaGLIPtin. Management: Strongly consider using an alternative to any strong CYP3A4 inducer in patients who are being treated with linagliptin. If this combination is used, monitor patients closely for evidence of reduced linagliptin effectiveness. Consider therapy modification
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lopinavir: PHENobarbital may decrease the serum concentration of Lopinavir. Management: Increased doses of lopinavir may be necessary when using these agents in combination. Do not use a once daily lopinavir/ritonavir regimen together with phenobarbital. Increase monitoring of therapeutic response in all patients using this combination. Consider therapy modification
Lorlatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lorlatinib. Avoid combination
Lumacaftor and Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lumacaftor and Ivacaftor. Specifically, the serum concentration of ivacaftor may be decreased. Avoid combination
Lumateperone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lumateperone. Avoid combination
Lumefantrine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lumefantrine. Avoid combination
Lurasidone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lurasidone. Avoid combination
Macimorelin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Macimorelin. Avoid combination
Macitentan: CYP3A4 Inducers (Strong) may decrease the serum concentration of Macitentan. Avoid combination
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Manidipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Manidipine. Management: Consider avoiding concomitant use of manidipine and strong CYP3A4 inducers. If combined, monitor closely for decreased manidipine effects and loss of efficacy. Increased manidipine doses may be required. Consider therapy modification
Maraviroc: CYP3A4 Inducers (Strong) may decrease the serum concentration of Maraviroc. Management: Increase maraviroc adult dose to 600 mg twice daily when used with strong CYP3A4 inducers. This does not apply to patients also receiving strong CYP3A4 inhibitors. Do not use maraviroc with strong CYP3A4 inducers in patients with CrCl less than 30 mL/min. Consider therapy modification
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Methadone: PHENobarbital may decrease the serum concentration of Methadone. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methoxyflurane: Barbiturates may enhance the nephrotoxic effect of Methoxyflurane. Barbiturates may increase the metabolism of Methoxyflurane. Avoid combination
Methylfolate: May decrease the serum concentration of PHENobarbital. Monitor therapy
Methylphenidate: May increase the serum concentration of PHENobarbital. Monitor therapy
MethylPREDNISolone: CYP3A4 Inducers (Strong) may decrease the serum concentration of MethylPREDNISolone. Management: Consider methylprednisolone dose increases in patients receiving strong CYP3A4 inducers and monitor closely for reduced steroid efficacy. Consider therapy modification
MetroNIDAZOLE (Systemic): PHENobarbital may decrease the serum concentration of MetroNIDAZOLE (Systemic). Monitor therapy
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May enhance the CNS depressant effect of Barbiturates. Mianserin may diminish the therapeutic effect of Barbiturates. Barbiturates may decrease the serum concentration of Mianserin. Avoid combination
Midostaurin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Midostaurin. Avoid combination
MiFEPRIStone: CYP3A4 Inducers (Strong) may decrease the serum concentration of MiFEPRIStone. Avoid combination
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mirodenafil: CYP3A4 Inducers (Strong) may decrease the serum concentration of Mirodenafil. Management: Consider avoiding the concomitant use of mirodenafil and strong CYP3A4 inducers. If combined, monitor for decreased mirodenafil effects. Mirodenafil dose increases may be required to achieve desired effects. Consider therapy modification
Mirtazapine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Mirtazapine. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May decrease the serum concentration of Barbiturates. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Naldemedine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Naldemedine. Avoid combination
Nalmefene: PHENobarbital may decrease the serum concentration of Nalmefene. Monitor therapy
Naloxegol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Naloxegol. Avoid combination
Neratinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Neratinib. Avoid combination
Netupitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Netupitant. Avoid combination
NIFEdipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of NIFEdipine. Avoid combination
Nilotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Nilotinib. Avoid combination
NiMODipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of NiMODipine. Avoid combination
Nisoldipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Nisoldipine. Avoid combination
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
OLANZapine: CYP1A2 Inducers (Weak) may decrease the serum concentration of OLANZapine. Monitor therapy
Olaparib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Olaparib. Avoid combination
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Osimertinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Osimertinib. Consider therapy modification
OXcarbazepine: CYP3A4 Inducers (Strong) may decrease the serum concentration of OXcarbazepine. Specifically, the concentrations of the 10-monohydroxy active metabolite of oxcarbazepine may be decreased. Monitor therapy
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: PHENobarbital may enhance the CNS depressant effect of OxyCODONE. PHENobarbital may decrease the serum concentration of OxyCODONE. Management: Avoid use of oxycodone and phenobarbital when possible. Monitor for respiratory depression/sedation. Because phenobarbital is also a strong CYP3A4 inducer, monitor for decreased oxycodone efficacy and withdrawal if combined. Consider therapy modification
Palbociclib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Palbociclib. Avoid combination
Panobinostat: CYP3A4 Inducers (Strong) may decrease the serum concentration of Panobinostat. Avoid combination
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
PAZOPanib: CYP3A4 Inducers (Strong) may decrease the serum concentration of PAZOPanib. Avoid combination
Perampanel: CYP3A4 Inducers (Strong) may decrease the serum concentration of Perampanel. Management: Increase the perampanel starting dose to 4 mg/day when perampanel is used concurrently with moderate and strong CYP3A4 inducers. Consider therapy modification
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Pexidartinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pexidartinib. Avoid combination
Phenytoin: May enhance the CNS depressant effect of PHENobarbital. PHENobarbital may decrease the serum concentration of Phenytoin. Phenytoin may increase the serum concentration of PHENobarbital. Monitor therapy
Pimavanserin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pimavanserin. Avoid combination
Piperaquine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Piperaquine. Avoid combination
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pitolisant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pitolisant. Management: For patients who are stable on pitolisant doses of 8.9 mg or 17.8 mg/day and who are also taking a strong CYP3A4 inducer, increase the pitolisant dose over 7 days to double the original dose (ie, to either 17.8 mg/day or 35.6 mg/day, respectively). Consider therapy modification
Polatuzumab Vedotin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Polatuzumab Vedotin. Exposure to unconjugated MMAE, the cytotoxic small molecule component of polatuzumab vedotin, may be decreased. Monitor therapy
PONATinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of PONATinib. Avoid combination
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Praziquantel: CYP3A4 Inducers (Strong) may decrease the serum concentration of Praziquantel. Management: Use of praziquantel with strong CYP3A4 inducers is contraindicated. Discontinue rifampin 4 weeks prior to initiation of praziquantel therapy. Rifampin may be resumed the day following praziquantel completion. Avoid combination
PrednisoLONE (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of PrednisoLONE (Systemic). Monitor therapy
PredniSONE: CYP3A4 Inducers (Strong) may decrease the serum concentration of PredniSONE. Monitor therapy
Pretomanid: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pretomanid. Avoid combination
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Primidone: May enhance the adverse/toxic effect of Barbiturates. Primidone is converted to phenobarbital, and thus becomes additive with existing barbiturate therapy. Monitor therapy
Progestins (Contraceptive): Barbiturates may diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Use of alternative, nonhormonal contraceptives is recommended. Consider therapy modification
Propacetamol: Barbiturates may increase the metabolism of Propacetamol. This may 1) diminish the desired effects of propacetamol; and 2) increase the risk of liver damage. Monitor therapy
Propafenone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Propafenone. Monitor therapy
Pyridoxine: May increase the metabolism of Barbiturates. Apparent in high pyridoxine doses (eg, 200 mg/day) Monitor therapy
QUEtiapine: CYP3A4 Inducers (Strong) may decrease the serum concentration of QUEtiapine. Management: An increase in quetiapine dose (as much as 5 times the regular dose) may be required to maintain therapeutic benefit. Reduce the quetiapine dose back to the previous/regular dose within 7-14 days of discontinuing the inducer. Consider therapy modification
QuiNIDine: PHENobarbital may enhance the hepatotoxic effect of QuiNIDine. PHENobarbital may decrease the serum concentration of QuiNIDine. Monitor therapy
QuiNINE: May increase the serum concentration of PHENobarbital. PHENobarbital may decrease the serum concentration of QuiNINE. Consider therapy modification
Radotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Radotinib. Management: Consider alternatives to this combination when possible as the risk of radotinib treatment failure may be increased. Consider therapy modification
Ramelteon: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ramelteon. Monitor therapy
Ranolazine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ranolazine. Avoid combination
Reboxetine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Reboxetine. Monitor therapy
Regorafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Regorafenib. Avoid combination
Ribociclib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ribociclib. Avoid combination
Rifamycin Derivatives: May increase the metabolism of Barbiturates. Monitor therapy
Rilpivirine: PHENobarbital may decrease the serum concentration of Rilpivirine. Avoid combination
RisperiDONE: CYP3A4 Inducers (Strong) may decrease the serum concentration of RisperiDONE. Management: Consider increasing the dose of oral risperidone (to no more than double the original dose) if a strong CYP3A4 inducer is initiated. For patients on IM risperidone, consider an increased IM dose or supplemental doses of oral risperidone. Consider therapy modification
Rivaroxaban: CYP3A4 Inducers (Strong) may decrease the serum concentration of Rivaroxaban. Avoid combination
Roflumilast: CYP3A4 Inducers (Strong) may decrease the serum concentration of Roflumilast. Management: Roflumilast U.S. prescribing information recommends against combining strong CYP3A4 inducers with roflumilast. The Canadian product monograph makes no such recommendation but notes that such agents may reduce roflumilast therapeutic effects. Avoid combination
Rolapitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Rolapitant. Management: Avoid rolapitant use in patients requiring chronic administration of strong CYP3A4 inducers. Monitor for reduced rolapitant response and the need for alternative or additional antiemetic therapy even with shorter-term use of such inducers. Consider therapy modification
RomiDEPsin: CYP3A4 Inducers (Strong) may decrease the serum concentration of RomiDEPsin. Avoid combination
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May increase the serum concentration of PHENobarbital. PHENobarbital may decrease the serum concentration of Rufinamide. Monitor therapy
Ruxolitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ruxolitinib. Monitor therapy
Sapropterin: PHENobarbital may decrease the serum concentration of Sapropterin. Specifically, phenobarbital may decrease tissue concentrations of tetrahydrobiopterin. Monitor therapy
SAXagliptin: CYP3A4 Inducers (Strong) may decrease the serum concentration of SAXagliptin. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sertraline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Sertraline. Monitor therapy
Simeprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Simeprevir. Avoid combination
Sirolimus: CYP3A4 Inducers (Strong) may decrease the serum concentration of Sirolimus. Management: Avoid concomitant use of strong CYP3A4 inducers and sirolimus if possible. If combined, monitor for reduced serum sirolimus concentrations. Sirolimus dose increases will likely be necessary to prevent subtherapeutic sirolimus levels. Consider therapy modification
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Sofosbuvir: PHENobarbital may decrease the serum concentration of Sofosbuvir. Avoid combination
Somatostatin Acetate: May enhance the adverse/toxic effect of Barbiturates. Specifically, Somatostatin Acetate may enhance or prolong Barbiturate effects, including sedative effects. Avoid combination
Sonidegib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Sonidegib. Avoid combination
SORAfenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of SORAfenib. Avoid combination
Stiripentol: PHENobarbital may decrease the serum concentration of Stiripentol. Avoid combination
SUFentanil: PHENobarbital may enhance the CNS depressant effect of SUFentanil. PHENobarbital may decrease the serum concentration of SUFentanil. Management: Avoid use of sufentanil and phenobarbital when possible. Monitor for respiratory depression/sedation. Because phenobarbital is also a strong CYP3A4 inducer, monitor for decreased sufentanil efficacy and withdrawal if combined. Consider therapy modification
Sulthiame: May enhance the adverse/toxic effect of PHENobarbital. Monitor therapy
SUNItinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of SUNItinib. Management: Avoid when possible. If such a combination cannot be avoided, sunitinib dose increases are recommended, and vary by indication. See full monograph for details. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tadalafil: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tadalafil. Management: Erectile dysfunction: monitor for decreased effectiveness - no standard dose adjustments recommended. Avoid use of tadalafil for pulmonary arterial hypertension in patients receiving a strong CYP3A4 inducer. Consider therapy modification
Tamoxifen: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Tamoxifen. CYP3A4 Inducers (Strong) may decrease the serum concentration of Tamoxifen. Management: Consider alternatives to concomitant use of strong CYP3A4 inducers and tamoxifen. If the combination cannot be avoided, monitor for reduced therapeutic effects of tamoxifen. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tasimelteon: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tasimelteon. Avoid combination
Tazemetostat: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tazemetostat. Avoid combination
Telithromycin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Telithromycin. Avoid combination
Temsirolimus: CYP3A4 Inducers (Strong) may decrease the serum concentration of Temsirolimus. Management: Consider increasing the dose of temsirolimus to 50 mg IV/week (from 25 mg IV/week) if a concomitant CYP3A4 strong inducer is necessary. Consider therapy modification
Teniposide: Barbiturates may decrease the serum concentration of Teniposide. Management: Consider alternatives to combined treatment with barbiturates and teniposide due to the potential for decreased teniposide concentrations. If the combination cannot be avoided, monitor teniposide response closely. Consider therapy modification
Tenofovir Alafenamide: PHENobarbital may decrease the serum concentration of Tenofovir Alafenamide. Avoid combination
Tetrahydrocannabinol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tetrahydrocannabinol. Monitor therapy
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tetrahydrocannabinol and Cannabidiol. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tezacaftor and Ivacaftor. Avoid combination
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Theophylline Derivatives: Barbiturates may decrease the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Thiotepa: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Thiotepa. CYP3A4 Inducers (Strong) may decrease the serum concentration of Thiotepa. Management: Thiotepa prescribing information recommends avoiding concomitant use of thiotepa and strong CYP3A4 inducers. If concomitant use is unavoidable, monitor for adverse effects. Consider therapy modification
Thiothixene: PHENobarbital may decrease the serum concentration of Thiothixene. Monitor therapy
TiaGABine: CYP3A4 Inducers (Strong) may decrease the serum concentration of TiaGABine. Management: Approximately 2-fold higher tiagabine doses and a more rapid dose titration will likely be required in patients concomitantly taking a strong CYP3A4 inducer. Consider therapy modification
Ticagrelor: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Ticagrelor. CYP3A4 Inducers (Strong) may decrease the serum concentration of Ticagrelor. Avoid combination
Tipranavir: PHENobarbital may decrease the serum concentration of Tipranavir. Tipranavir may decrease the serum concentration of PHENobarbital. Consider therapy modification
Tofacitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tofacitinib. Avoid combination
Tolvaptan: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tolvaptan. Management: If concurrent use is necessary, increased doses of tolvaptan (with close monitoring for toxicity and clinical response) may be needed. Avoid combination
Toremifene: CYP3A4 Inducers (Strong) may decrease the serum concentration of Toremifene. Avoid combination
Trabectedin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Trabectedin. Avoid combination
TraMADol: PHENobarbital may enhance the CNS depressant effect of TraMADol. PHENobarbital may decrease the serum concentration of TraMADol. Management: Avoid use of tramadol and phenobarbital when possible. Monitor for respiratory depression/sedation. Because phenobarbital is also a strong CYP3A4 inducer, monitor for decreased tramadol efficacy and withdrawal if combined. Consider therapy modification
Tricyclic Antidepressants: Barbiturates may increase the metabolism of Tricyclic Antidepressants. Consider therapy modification
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tropisetron: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tropisetron. Monitor therapy
Ubrogepant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ubrogepant. Avoid combination
Udenafil: CYP3A4 Inducers (Strong) may decrease the serum concentration of Udenafil. Monitor therapy
Ulipristal: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ulipristal. Avoid combination
Ulipristal: Barbiturates may decrease the serum concentration of Ulipristal. Avoid combination
Upadacitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Upadacitinib. Avoid combination
Valbenazine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Valbenazine. Avoid combination
Valproate Products: May increase the serum concentration of Barbiturates. Barbiturates may decrease the serum concentration of Valproate Products. Monitor therapy
Vandetanib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vandetanib. Avoid combination
Velpatasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Velpatasvir. Avoid combination
Vemurafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vemurafenib. Management: Avoid concurrent use of vemurafenib with a strong CYP3A4 inducer and replace with another agent when possible. If a strong CYP3A4 inducer is indicated and unavoidable, the dose of vemurafenib may be increased by 240 mg (1 tablet) as tolerated. Consider therapy modification
Venetoclax: CYP3A4 Inducers (Strong) may decrease the serum concentration of Venetoclax. Avoid combination
Vilazodone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vilazodone. Management: Consider increasing vilazodone dose by as much as 2-fold (do not exceed 80 mg/day), based on response, in patients receiving strong CYP3A4 inducers for > 14 days. Reduce to the original vilazodone dose over 1-2 weeks after inducer discontinuation. Consider therapy modification
VinCRIStine (Liposomal): CYP3A4 Inducers (Strong) may decrease the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vinflunine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vinflunine. Avoid combination
Vitamin K Antagonists (eg, warfarin): Barbiturates may increase the metabolism of Vitamin K Antagonists. Management: Monitor INR more closely. An anticoagulant dose increase may be needed after a barbiturate is initiated or given at an increased dose. Anticoagulant dose decreases may be needed following barbiturate discontinuation or dose reduction. Consider therapy modification
Vorapaxar: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vorapaxar. Avoid combination
Voriconazole: Barbiturates may decrease the serum concentration of Voriconazole. Avoid combination
Vortioxetine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vortioxetine. Management: Consider increasing the vortioxetine dose to no more than 3 times the original dose when used with a strong drug metabolism inducer for more than 14 days. The vortioxetine dose should be returned to normal within 14 days of stopping the strong inducer. Consider therapy modification
Voxelotor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Voxelotor. Management: Avoid concomitant use of voxelotor and strong CYP3A4 inducers. If concomitant use is unavoidable, increase the voxelotor dose to 2,500 mg once daily. Consider therapy modification
Voxilaprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Voxilaprevir. Avoid combination
Zaleplon: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zaleplon. Management: Consider the use of an alternative hypnotic that is not metabolized by CYP3A4 in patients receiving strong CYP3A4 inducers. If zalephon is combined with a strong CYP3A4 inducer, monitor for decreased effectiveness of zaleplon. Consider therapy modification
Zanubrutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zanubrutinib. Avoid combination
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Zonisamide: PHENobarbital may decrease the serum concentration of Zonisamide. Monitor therapy
Zuclopenthixol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zuclopenthixol. Monitor therapy
Adverse Reactions
Frequency not defined.
Cardiovascular: Bradycardia, hypotension, syncope, thrombophlebitis (IV)
Central nervous system: Agitation, anxiety, ataxia, central nervous system stimulation, central nervous system depression, confusion, dizziness, drowsiness, hallucination, hangover effect, headache, impaired judgement, insomnia, lethargy, nervousness, nightmares
Dermatologic: Exfoliative dermatitis, skin rash, Stevens-Johnson syndrome
Gastrointestinal: Constipation, nausea, vomiting
Genitourinary: Oliguria
Hematologic & oncologic: Agranulocytosis, thrombocytopenia, megaloblastic anemia
Local: Pain at injection site
Neuromuscular & skeletal: Hyperkinesia, laryngospasm
Respiratory: Apnea (especially with rapid IV use), hypoventilation, respiratory depression
Warnings/Precautions
Concern related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Hypersensitivity: Exfoliative dermatitis and Stevens-Johnson syndrome, possibly fatal, may occur; discontinue if dermatological reactions occur.
- Paradoxical stimulatory response: May cause paradoxical responses, including agitation and hyperactivity, particularly in patients with acute or chronic pain and pediatric patients.
- Respiratory depression: May cause respiratory depression particularly when administered intravenously; use with caution patients with respiratory disease, including status asthmaticus.
Disease-related concerns:
- Anemia: Use with caution in patients with severe anemia.
- Cardiac disease: Use with caution in patients with cardiac disease and in hemodynamically unstable patients (hypotension or shock).
- Depression: Use with caution in patients with depression or suicidal tendencies.
- Diabetes: Use with caution in patients with diabetes.
- Drug abuse: Use with caution in patients with a history of drug abuse; potential for drug dependency exists. Tolerance, psychological and physical dependence may occur with prolonged use.
- Hepatic impairment: Use with caution in patients with hepatic impairment. Avoid use in patients showing the premonitory signs of hepatic coma.
- Hyperthyroidism: Use with caution in patients with hyperthyroidism.
- Hypoadrenalism: Use with caution in patients with hypoadrenalism.
- Renal impairment: Use with caution in patients with renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Debilitated patients: Use with caution in patients who are debilitated.
- Fever: Use with caution in patients with a fever.
- Pediatric: Phenobarbital has been associated with cognitive deficits in children receiving therapy for complicated febrile seizures.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension and cardiovascular collapse (AAP 1997; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol with caution in neonates See manufacturer’s labeling.
- Injection: Do not administer intra-arterially or subcutaneously. Avoid perivascular extravasation. Too rapid administration may cause severe respiratory depression, apnea, laryngospasm, hypertension or vasodilation with fall in blood pressure. Phenobarbital IV may require ≥15 minutes before reaching peak concentrations in the brain; injecting phenobarbital until the convulsions stop may lead to severe barbiturate induced depression. Intramuscular (IM) injection should be confined to a total volume of 5 mL and made in a large muscle in order to avoid possible tissue irritation. Discontinue injection in any patient who complains of limb pain.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures and respiratory depression; use caution (AAP 1997; Zar 2007).
Other warnings/precautions:
- Acute pain: Use with caution in patients with acute or chronic pain; paradoxical excitement could be induced or important symptoms could be masked.
- Withdrawal: Anticonvulsants should not be discontinued abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal.
Monitoring Parameters
Phenobarbital serum concentrations (as clinically indicated); CNS status; liver enzymes (periodic); CBC with differential (periodic); renal function (periodic); seizure activity; signs and symptoms of suicidality (eg, anxiety, depression, behavior changes)
IV use: Respiratory rate, heart rate, blood pressure, IV site (stop injection if patient complains of pain in the limb)
Pregnancy
Pregnancy Risk Factor
D
Pregnancy Considerations
Phenobarbital crosses the placenta (Harden 2009b). Barbiturates can be detected in the placenta, fetal liver, and fetal brain. Fetal and maternal blood concentrations may be similar following parenteral administration. An increased incidence of fetal abnormalities may occur following maternal use. When used during the third trimester of pregnancy, withdrawal symptoms may occur in the neonate, including seizures and hyperirritability; symptoms of withdrawal may be delayed in the neonate up to 14 days after birth. Use during labor does not impair uterine activity; however, respiratory depression may occur in the newborn; resuscitation equipment should be available, especially for premature infants. Use for the treatment of epilepsy should be avoided during pregnancy (Harden 2009a).
A registry is available for women exposed to phenobarbital during pregnancy: Pregnant women may enroll themselves into the North American Antiepileptic Drug (AED) Pregnancy Registry (888-233-2334 or http://www.aedpregnancyregistry.org).
Patient Education
What is this drug used for?
- It is used to help control certain kinds of seizures.
- It is used to treat anxiety.
- It is used to treat sleep problems.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Fatigue
- Headache
- Nausea
- Vomiting
- Injection site irritation
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Mood changes
- Behavioral changes
- Shortness of breath
- Confusion
- Severe anxiety
- Agitation
- Bone pain
- Seizures
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.