Boxed Warning
Cardiovascular risk associated with rapid infusion (injection):
The rate of intravenous phenytoin administration should not exceed 50 mg/minute in adults and 1 to 3 mg/kg/minute (or 50 mg/minute, whichever is slower) in pediatric patients because of the risk of severe hypotension and cardiac arrhythmias. Careful cardiac monitoring is needed during and after administering intravenous phenytoin. Although the risk of cardiovascular toxicity increases with infusion rates above the recommended infusion rate, these events have also been reported at or below the recommended infusion rate. Reduction in rate of administration or discontinuation of dosing may be needed.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral, as sodium:
Dilantin: 30 mg [contains fd&c yellow #10 (quinoline yellow)]
Dilantin: 100 mg
Phenytek: 200 mg, 300 mg [contains brilliant blue fcf (fd&c blue #1), fd&c blue #1 aluminum lake, fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #10 aluminum lake]
Generic: 100 mg, 200 mg, 300 mg
Solution, Injection, as sodium:
Generic: 50 mg/mL (2 mL, 5 mL)
Suspension, Oral:
Dilantin: 125 mg/5 mL (237 mL) [orange-vanilla flavor]
Generic: 125 mg/5 mL (4 mL, 237 mL)
Tablet Chewable, Oral:
Dilantin Infatabs: 50 mg [scored]
Phenytoin Infatabs: 50 mg [scored; contains fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake, saccharin sodium]
Generic: 50 mg
Pharmacology
Mechanism of Action
Stabilizes neuronal membranes and decreases seizure activity by increasing efflux or decreasing influx of sodium ions across cell membranes in the motor cortex during generation of nerve impulses; prolongs effective refractory period and suppresses ventricular pacemaker automaticity, shortens action potential in the heart
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Slow, variable; dependent on product formulation; decreased in neonates
Distribution
Vd:
Neonates: Premature: 1 to 1.2 L/kg; Full-term: 0.8 to 0.9 L/kg
Infants: 0.7 to 0.8 L/kg
Children: 0.7 L/kg
Adults: 0.52 to 0.78 L/kg (Cranford 1978; Lund 1974)
Metabolism
Follows dose-dependent (Michaelis-Menten) pharmacokinetics; "apparent" or calculated half-life is dependent upon serum concentration, therefore, metabolism is best described in terms of Vmax (metabolic capacity) and Km (constant equal to the concentration at which the rate of metabolism is 1/2 of Vmax); Vmax is increased in infants >6 months and children compared to adults; major metabolite (via oxidation) HPPA undergoes enterohepatic recycling and elimination in urine as glucuronides
Excretion
Urine (<5% as unchanged drug); as glucuronides.
Clearance: Highly variable, dependent upon intrinsic hepatic function and dose administered; increased clearance and decreased serum concentrations with febrile illness. Note: In newborns (PNA <7 days), clearance is low but rapidly accelerates to older infant levels by 4 or 5 weeks of life (Patsalos 2008).
Onset of Action
IV: ~0.5 to 1 hour
Time to Peak
Serum (formulation dependent): Oral: Extended-release capsule: 4 to 12 hours; Immediate-release preparation: 1.5 to 3 hours
Half-Life Elimination
Note: Elimination is not first-order (ie, follows Michaelis-Menten pharmacokinetics); half-life increases with increasing phenytoin concentrations; best described using parameters such as Vmax and Km (Patsalos 2008).
IV: 10 to 12 hours.
Oral:
Capsule, oral suspension: Average 22 hours (range: 7 to 42 hours).
Chewable tablet: Average 14 hours (range: 7 to 29 hours).
Protein Binding
Neonates: ≥80% (≤20% free)
Infants: ≥85% (≤15% free)
Adults: 87.8% to 91.9% (Richens 1979)
Others: Decreased protein binding
Disease states resulting in a decrease in serum albumin concentration: Burns, hepatic cirrhosis, nephrotic syndrome, pregnancy, cystic fibrosis
Disease states resulting in an apparent decrease in affinity of phenytoin for serum albumin: Renal failure, jaundice (severe), other drugs (displacers), hyperbilirubinemia (total bilirubin >15 mg/dL), CrCl <25 mL/minute (unbound fraction is increased two- to threefold in uremia)
Use in Specific Populations
Special Populations: Renal Function Impairment
Increased fraction of unbound phenytoin may occur.
Special Populations: Hepatic Function Impairment
Increased fraction of unbound phenytoin may occur.
Special Populations: Elderly
Clearance decreases ~20% in patients >70 years of age.
Use: Labeled Indications
Focal (partial) onset seizures and generalized onset seizures: Treatment of patients with focal and generalized onset seizures and prevention of seizures following craniotomy. May be used off-label for other seizure types.
Status epilepticus: Treatment of patients with convulsive and nonconvulsive status epilepticus.
Use: Off Label
Seizures, posttraumatic (prevention)ayes
Data from a randomized, double-blind, placebo-controlled trial in patients with serious head trauma support the use of phenytoin to prevent posttraumatic seizures (PTSs) in patients who recently (within 1 week) experienced a traumatic brain injury (TBI). Phenytoin did not reduce the incidence of late (day 8 or later) PTS Temkin 1990. Similarly, a meta-analysis that included this controlled trial as well as several retrospective cohort studies also found a decrease in early PTS with phenytoin Wilson 2018.
Based on the Brain Trauma Foundation's guidelines for the management of severe traumatic brain injury and the American Academy of Neurology's practice parameter for antiepileptic drug prophylaxis in severe traumatic brain injury, phenytoin is effective and recommended to decrease the risk of PTS occurring within the first 7 days of TBI AAN [Chang 2003], BTF [Carney 2017].
Contraindications
Hypersensitivity to phenytoin, other hydantoins, or any component of the formulation; concurrent use of delavirdine; history of prior acute hepatotoxicity attributable to phenytoin
Injection: Additional contraindications: Sinus bradycardia, sinoatrial block, second- and third-degree heart block, Adams-Stokes syndrome
Canadian labeling (oral formulation): Additional contraindications (not in US labeling): Sick sinus syndrome, sinus bradycardia, sinoatrial block, second- and third-degree heart block; QT interval prolongation; Adams-Stokes syndrome; or other heart rhythm disorders
Dosage and Administration
Dosing: Adult
Note: Safety: Before prescribing, consider testing for HLA-B*1502 allele in patients at increased risk of developing serious cutaneous adverse reactions (ie, those of Asian ancestry, including South Asian Indians) (Locharernkul 2008; Löscher 2009). IV administration: Due to risk of cardiovascular adverse effects and local tissue injury, the maximum rate of administration is 50 mg/minute under continuous cardiac, blood pressure, and respiratory monitoring; when rapid IV administration is necessary, use of fosphenytoin is generally preferred (AES [Glauser 2016]; Drislane 2019; Meek 1999). Refer to institutional protocol for specific monitoring requirements. Dosage forms: Doses for capsules (extended release) and injection are expressed as phenytoin sodium salt. Doses for oral suspension and chewable tablets are expressed as phenytoin base (see Dosage form conversions for equivalence). To ensure optimal absorption, individual oral doses should not exceed 400 mg (Jung 1980).
Seizures:
Craniotomy, seizure prophylaxis (alternative agent):
Loading dose: IV: 15 mg/kg at a rate of ≤50 mg/minute prior to incision; maximum dose: 2 g (Inaba 2013; Lee 1989; Paisansathan 2019).
Postoperative prophylaxis: IV, Oral: 5 to 6 mg/kg/day in 2 to 3 divided doses; usual daily dose: 300 to 400 mg; adjust dose based on response and serum concentrations (Lee 1989; Schachter 2019a). Note: Duration individualized based on underlying intracranial pathology and other clinical considerations (AAN [Glantz 2000]; Drappatz 2019; Iuchi 2015; Merli 2019).
Focal (partial) onset seizures and generalized onset seizures: Note: FDA approved for generalized tonic-clonic and complex partial seizures; may be used off-label for other seizure types. Use of a loading dose is suggested for patients who require rapid attainment of a therapeutic serum level; in the absence of a loading dose, full effect is typically achieved after 1 to 3 weeks (ie, when steady-state serum concentrations are reached).
Fixed (nonweight-based) dosing (manufacturer's labeling):
Loading dose (optional) (phenytoin naive): Oral (capsule [extended release]): 1 g divided into 3 doses (eg, 400 mg, 300 mg, 300 mg) administered at 2-hour intervals; begin maintenance dose 24 hours after first loading dose.
Maintenance dose: Oral (capsule [extended release]): Initial: 100 mg 3 to 4 times daily; adjust dose based on response and serum concentrations.
Weight-based dosing (off-label): Note: May be used to individualize loading dose and estimate initial maintenance dose requirements according to body weight.
Loading dose (optional) (phenytoin naive): IV, Oral: 15 mg/kg given in 1 to 3 divided doses over 24 hours; usual total loading dose is 1 to 1.5 g (AES [Glauser 2016]; Gaspard 2019; Osborn 1987); begin maintenance dose 8 to 12 hours after loading dose.
Maintenance dose: IV, Oral: Initial: 4 to 7 mg/kg/day (usual 300 to 400 mg/day) given in 2 to 4 divided doses; adjust dose based on response and serum concentrations (Murphy 2016). Some experts recommend initiating maintenance therapy with 5 mg/kg/day in 2 divided doses (Schachter 2019a). A maximum dose has not been established; caution should be used in prescribing maintenance doses >600 mg/day.
Traumatic brain injury, prevention of early posttraumatic seizure (alternative agent) (off-label use): Note: For use in select patients at elevated risk of early seizures with concerns for secondary complications. Dosing may be center specific; refer to institutional protocols.
Loading dose: IV: 17 to 20 mg/kg at a rate of ≤50 mg/minute; maximum dose: 2 g (Debenham 2011; Inaba 2013); begin maintenance dose 8 to 12 hours after loading dose.
Maintenance dose: IV, Oral: 100 mg every 8 hours (Debenham 2011) or 5 mg/kg/day (round to the nearest 100 mg) divided every 8 hours (Inaba 2013). Note: Duration of prophylaxis varies, generally short-term use (eg, ~7 days) (BTF [Carney 2017]; Inaba 2013).
Status epilepticus (convulsive and nonconvulsive) (alternative agent): Note: If available, fosphenytoin is preferred because it is better tolerated and can be administered more rapidly than phenytoin (AES [Glauser 2016]; DeToledo 2000). Generally administered as part of initial therapy with or immediately after a benzodiazepine (eg, lorazepam IV) (Drislane 2019; Gaspard 2019; NCS [Brophy 2012]).
Loading dose (phenytoin naive): IV: 20 mg/kg at a rate of 25 to 50 mg/minute in combination with a parenteral benzodiazepine (eg, lorazepam) under continuous cardiac and blood pressure monitoring; reduce infusion rate if significant adverse events occur; if necessary, may give an additional dose of 5 to 10 mg/kg 10 minutes after the loading dose; maximum total loading dose: 30 mg/kg (Drislane 2019; NCS [Brophy 2012]). Begin maintenance dose 8 to 12 hours after loading dose.
Maintenance dose: IV, Oral: Initial: 4 to 7 mg/kg/day (usual 300 to 400 mg/day) given in 2 to 4 divided doses; adjust dose based on response and serum concentrations (Murphy 2016). Some experts recommend initiating maintenance therapy with 5 mg/kg/day in 2 divided doses (Schachter 2019a). A maximum dose has not been established; caution should be used in prescribing maintenance doses >600 mg/day. (See Focal (partial) onset seizures and generalized onset seizures for nonweight-based maintenance dose).
Discontinuation of therapy: In chronic therapy, phenytoin should be withdrawn gradually over 2 to 6 months or gradually transitioned to another antiepileptic agent to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal (Schachter 2019b).
Dosage form conversions:
Between IV and oral capsule formulations: Convert using the same total daily dose. Oral capsules are ~10% less bioavailable than injectable formulation; dosage adjustments and closer serum monitoring may be necessary.
Between phenytoin base (oral suspension, chewable tablets) and phenytoin sodium (capsule): Dosage adjustments and closer serum monitoring may be necessary when switching between formulations.
Conversion: Phenytoin base ~92 mg is equivalent to phenytoin sodium 100 mg.
Dosing: Geriatric
Refer to adult dosing; clearance is decreased in geriatric patients; lower doses or less frequent dosing may be required.
Dosing: Pediatric
Note: Dosage should be individualized based upon clinical response and serum concentrations; maintenance therapy dosage adjustments are typically not made more frequently than every 7 days. Phenytoin base (eg, oral suspension, chewable tablets) contains ~8% more drug than phenytoin sodium (~92 mg base is equivalent to 100 mg phenytoin sodium). Dosage adjustments and closer serum monitoring may be necessary when switching dosage forms.
Status epilepticus: Infants, Children, and Adolescents:
Manufacturer labeling: Loading dose: IV: 15 to 20 mg/kg in a single or divided dose; then begin maintenance therapy usually 12 hours after dose
Alternate dosing: AAP, NCS recommendations: Loading dose: IV: 20 mg/kg in a single or divided doses; maximum dose: 1000 mg; then begin maintenance therapy usually 12 hours after dose (Brophy 2012; Hegenbarth 2008). An additional load of 5 to 10 mg/kg if status epilepticus is not resolved has been used; however, some experts recommend trying another agent once a total loading dose of 20 mg/kg has been given (Brophy 2012).
Seizures: Infants, Children, and Adolescents:
Loading dose (if not previously on phenytoin): IV, Oral: 15 to 20 mg/kg; if currently on phenytoin, reloading dose should be based upon serum concentrations and recent dosing history; an oral loading dose should be divided into 3 doses and administered every 2-4 hours to decrease GI adverse effects and to ensure complete oral absorption
Maintenance therapy: IV, Oral: Initial: 5 mg/kg/day in divided doses (based upon dosage form, see below); usual range: 4 to 8 mg/kg/day; maximum daily dose: 300 mg/day. Some experts suggest higher maintenance doses (8 to 10 mg/kg/day) may be necessary in infants and young children (Guerrini 2006). Dosing should be based upon ideal body weight (IBW).
Usual dosing range (Bauer 1983; Chiba 1980; Suzuki 1994):
6 months to 3 years: 8 to 10 mg/kg/day
4 to 6 years: 7.5 to 9 mg/kg/day
7 to 9 years: 7 to 8 mg/kg/day
10 to 16 years: 6 to 7 mg/kg/day
Dosing interval (product specific):
Immediate release preparations (including injection, suspension, and chewable tablets): Divide daily dose into 2 to 3 doses per day
Extended release preparations: In most pediatric patients, usually dosed every 12 hours; however, in adolescent patients with sufficiently long half-life, may be dosed every 24 hours
Seizure prophylaxis, traumatic brain injury: Limited data available; efficacy results variable: Infants, Children, and Adolescents: IV: Initial: 18 mg/kg over 20 minutes; followed by 6 mg/kg/day divided every 8 hours for 48 hours was used in a double-blind, placebo-controlled trial of 102 pediatric patients (n=46 treatment group; median age: 6.4 years) and showed no significance difference in seizure frequency between groups; however, the trial was stopped early due to a very low seizure frequency among both study groups (Young 2004). In a retrospective trial, reduced seizure frequency with prophylactic phenytoin use was described (Lewis 1993). Note: Current guidelines suggest that prophylactic phenytoin may be considered to reduce the incidence of early post-traumatic seizures in pediatric patients with severe traumatic brain injuries but it does not reduce the risk of long-term seizures or improve neurologic outcome (Kochanek 2012).
Dosing: Obesity
Adults: Evidence from one small study in adult patients (N=24) with obesity (range: 71 to 197 kg) demonstrated that the volume of distribution (Vd) was 0.68 ± 0.03 L/kg (range: 0.53 to 0.85 L/kg) and distribution into weight in excess of IBW is disproportionately greater (by a factor of 1.33) (Abernethy 1985). Based on this evidence, the following dosing strategies have been suggested:
Loading dose:
14 mg/kg (IBW) + 19 mg/kg (weight in excess of IBW); maximum dose: 2 g (Abernethy 1985; Erstad 2004)
For example: For a patient with a total body weight (TBW) of 300 lb (136 kg) and an IBW of 73 kg
Loading dose = 14 mg/kg (73 kg) + 19 mg/kg (136 kg minus 73 kg) = 2,219 mg; administer the maximum dose of 2,000 mg
OR
May also target a specific concentration (eg, 15 to 20 mg/L) by using the Vd obtained from patients with obesity (Abernethy 1985; Burton 2006). Therefore, the concentration desired (in mg/L) may be multiplied by this Vd (obesity) (in L) which is determined using the patient's total and ideal body weights.
Vd (obesity) = 0.65 L/kg [(IBW) + 1.33 (TBW – IBW)]
Loading dose = Calculated Vd (obesity) (target concentration)
For example: For a patient with a total body weight (TBW) of 300 lb (136 kg) and an IBW of 73 kg
Vd (obesity) = 0.65 L/kg [(73 kg) + 1.33 (136 kg – 73 kg)] = 101.9 L; then,
Loading dose = 101.9 L x 15 mg/L = 1,529 mg
Maintenance dose: Base on ideal body weight if using weight-based regimens or use conventional daily doses with adjustments based upon therapeutic drug monitoring and clinical effectiveness. (Abernethy 1985; Erstad 2002; Erstad 2004)
Note: Additional data are necessary to further define dosing strategies in the obese patient.
Reconstitution
IV: May be further diluted in NS to a final concentration ≥5 mg/mL; infusion must be completed within 4 hours after preparation. Do not refrigerate.
Administration
Oral:
Immediate release: Divide daily dose into 2 to 3 doses per day; if the daily dosage cannot be divided equally, take the larger dose before retiring.
Chewable tablets: May chew thoroughly before swallowing or swallow whole.
Suspension: Shake well prior to use; measure and administer dose using a calibrated oral dosing syringe (or other accurate dose-measuring device). Absorption is impaired when phenytoin suspension is given concurrently to patients who are receiving continuous nasogastric feedings. A method to resolve this interaction is to divide the daily dose of phenytoin and withhold the administration of nutritional supplements for 1 to 2 hours before and after each phenytoin dose. The manufacturer recommends not to administer concomitantly with an enteral feeding preparation.
Extended release: Usually dosed every 12 hours; however, in patients with sufficiently long half-life, may be dosed every 24 hours.
IM: Avoid IM administration due to severe risk of local tissue destruction and necrosis; use fosphenytoin if IM administration necessary (Boucher 1996; Meek 1999). The manufacturer's labeling includes IM administration; however, in general the IM route should be avoided and should NOT be used for status epilepticus.
IV: For patients who are in status epilepticus, hemodynamically unstable, or develop hypotension/bradycardia with IV administration of phenytoin, consider the use of fosphenytoin when loading instead. Although phenytoin may be administered by direct IV injection, it is preferable that phenytoin be administered via infusion pump either undiluted or diluted in NS as an IV piggyback (IVPB) to prevent exceeding the maximum infusion rate (monitor closely for extravasation during infusion). Administer directly into a large peripheral or central vein through a large-gauge catheter. Infusion must be completed within 4 hours after dilution in NS. The maximum rate of IV administration is 50 mg/minute. Highly sensitive patients (eg, elderly patients, patients with preexisting cardiovascular conditions) should receive phenytoin more slowly (eg, 20 mg/minute) (Meek 1999). When using IV route for oral replacement, administer at slower rate as either a loading dose or by intermittent infusion. An in-line 0.22- to 0.55-micron filter is recommended for IVPB solutions due to the potential for precipitation of the solution. Following IV administration, NS should be injected through the same needle or IV catheter to prevent irritation.
SubQ: SubQ administration is not recommended because of the possibility of local tissue damage (due to high pH).
Vesicant; ensure proper needle or catheter placement prior to and during IV infusion. Avoid extravasation.
Extravasation management: If extravasation occurs, stop infusion immediately and disconnect (leave needle/cannula in place); gently aspirate extravasated solution (do NOT flush the line); remove needle/cannula; elevate extremity and apply dry heat; closely monitor for tissue sloughing or compartment syndrome (Reynolds 2014). There is conflicting information regarding an antidote; some sources recommend not to use an antidote (Montgomery 1999 [pediatric reference]) or to use hyaluronidase in refractory cases (Reynolds 2014), while other sources recommend hyaluronidase.
Hyaluronidase (if appropriate): SubQ: Administer four separate 0.2 mL injections of a 15 units/mL solution (using a 25-gauge needle) into area of extravasation (Sokol 1998).
Dietary Considerations
Folic acid: Phenytoin may decrease mucosal uptake of folic acid; to avoid folic acid deficiency and megaloblastic anemia, some clinicians recommend giving patients on anticonvulsants prophylactic doses of folic acid and cyanocobalamin (Belcastro 2012). Folic acid 0.5 mg/day has been shown to reduce the incidence of phenytoin-induced gingival overgrowth in children (Arya 2011). However, folate supplementation may increase seizures in some patients (dose dependent). Discuss with health care provider prior to using any supplements.
Calcium: Hypocalcemia has been reported in patients taking prolonged high-dose therapy with an anticonvulsant. Some clinicians have given an additional 4,000 units/week of vitamin D (especially in those receiving poor nutrition and getting no sun exposure) to prevent hypocalcemia.
Vitamin B: Phenytoin use has been associated with low serum concentrations of vitamin B2 (riboflavin), B6 (pyridoxine) and B12 (cyanocobalamin), which may contribute to hyperhomocysteinemia. Hyperhomocysteinemia may contribute to cardiovascular disease, venous thromboembolic disease, dementia, neuropsychiatric symptoms and poor seizure control. Some clinicians recommend administering riboflavin, pyridoxine and cyanocobalamin supplements in patients taking phenytoin (Apeland 2003; Apeland 2008; Belcastro 2012; Bochyńska 2012).
Vitamin D: Phenytoin interferes with vitamin D metabolism and osteomalacia may result; may need to supplement with vitamin D
Tube feedings: Tube feedings decrease phenytoin absorption. To avoid decreased serum levels with continuous NG feeds, hold feedings for 1 to 2 hours prior to and 1 to 2 hours after phenytoin administration, if possible. The manufacturer recommends not to administer concomitantly with an enteral feeding preparation. There is a variety of opinions on how to administer phenytoin with enteral feedings. Be consistent throughout therapy.
Injection may contain sodium.
Storage
Capsule, tablet: Store at 20°C to 25°C (68°F to 77°F). Protect capsules from light. Protect capsules and tablets from moisture.
Oral suspension: Store at 20°C to 25°C (68°F to 77°F); do not freeze. Protect from light.
Solution for injection: Store at 15°C to 30°C (59°F to 86°F). Use only clear solutions free of precipitate and haziness; slightly yellow solutions may be used. Precipitation may occur if solution is refrigerated and may dissolve at room temperature. Discard any unused product.
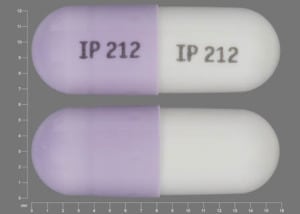
Phenytoin Images
Drug Interactions
Abemaciclib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Abemaciclib. Avoid combination
Abiraterone Acetate: CYP3A4 Inducers (Strong) may decrease the serum concentration of Abiraterone Acetate. Management: Avoid whenever possible. If such a combination cannot be avoided, increase abiraterone acetate dosing frequency from once daily to twice daily during concomitant use. Consider therapy modification
Acalabrutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Acalabrutinib. Management: Avoid co-administration of strong CYP3A inducers in patients taking acalabrutinib. If strong CYP3A inducers cannot be avoided, increase the dose of acalabrutinib to 200 mg twice daily. Consider therapy modification
Acemetacin: May increase the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
Acetaminophen: Fosphenytoin-Phenytoin may decrease the serum concentration of Acetaminophen. Specifically, serum concentrations of acetaminophen may be decreased (leading to decreased efficacy), but the formation of the toxic N-acetyl-p-benzoquinone imine (NAPQI) metabolite may be increased (leading to increased hepatotoxicity). Monitor therapy
Afatinib: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Afatinib. Management: Per US labeling: if requiring chronic use of P-gp inducers, increase afatinib dose by 10 mg as tolerated; reduce to original afatinib dose 2-3 days after stopping P-gp inducers. Per Canadian labeling: avoid combination if possible. Consider therapy modification
Albendazole: Phenytoin may decrease serum concentrations of the active metabolite(s) of Albendazole. Monitor therapy
Alcohol (Ethyl): May enhance the CNS depressant effect of Phenytoin. Alcohol (Ethyl) may increase the serum concentration of Phenytoin. This may be particularly applicable with acute, heavy alcohol consumption. Alcohol (Ethyl) may decrease the serum concentration of Phenytoin. This may be particularly applicable with chronic, heavy alcohol consumption. Monitor therapy
Alpelisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Alpelisib. Avoid combination
Amiodarone: Phenytoin may decrease the serum concentration of Amiodarone. Amiodarone may increase the serum concentration of Phenytoin. Monitor therapy
Amphetamines: May decrease the serum concentration of Phenytoin. Monitor therapy
Antifungal Agents (Azole Derivatives, Systemic): May increase the serum concentration of Phenytoin. Applicable Isavuconazonium considerations are addressed in separate monographs. Phenytoin may decrease the serum concentration of Antifungal Agents (Azole Derivatives, Systemic). Management: Concomitant therapy with itraconazole, voriconazole, or ketoconazole and phenytoin should probably be avoided, as antifungal failure is likely. Consider selecting alternative antifungal therapy. Exceptions: Isavuconazonium Sulfate. Consider therapy modification
Antihepaciviral Combination Products: CYP3A4 Inducers (Strong) may decrease the serum concentration of Antihepaciviral Combination Products. Avoid combination
Apixaban: Inducers of CYP3A4 (Strong) and P-glycoprotein may decrease the serum concentration of Apixaban. Avoid combination
Apremilast: CYP3A4 Inducers (Strong) may decrease the serum concentration of Apremilast. Avoid combination
Aprepitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Aprepitant. Avoid combination
ARIPiprazole: CYP3A4 Inducers (Strong) may decrease the serum concentration of ARIPiprazole. Management: Double the oral aripiprazole dose and closely monitor. Reduce oral aripiprazole dose to 10-15 mg/day (for adults) if the inducer is discontinued. Avoid use of strong CYP3A4 inducers for more than 14 days with extended-release injectable aripiprazole. Consider therapy modification
ARIPiprazole Lauroxil: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of ARIPiprazole Lauroxil. Management: Patients taking the 441 mg dose of aripiprazole lauroxil increase their dose to 662 mg if used with a strong CYP3A4 inducer for more than 14 days. No dose adjustment is necessary for patients using the higher doses of aripiprazole lauroxil. Consider therapy modification
Artemether: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Artemether. Specifically, dihydroartemisinin concentrations may be reduced. CYP3A4 Inducers (Strong) may decrease the serum concentration of Artemether. Avoid combination
Asunaprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Asunaprevir. Avoid combination
Avapritinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Avapritinib. Avoid combination
Axitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Axitinib. Avoid combination
Bazedoxifene: Phenytoin may decrease the serum concentration of Bazedoxifene. This may lead to loss of efficacy or, if bazedoxifene is combined with estrogen therapy, an increased risk of endometrial hyperplasia. Monitor therapy
Bedaquiline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Bedaquiline. Avoid combination
Benperidol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Benperidol. Monitor therapy
Benzhydrocodone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Benzhydrocodone. Specifically, the serum concentrations of hydrocodone may be reduced. Monitor therapy
Benzodiazepines: May increase the serum concentration of Phenytoin. Short-term exposure to benzodiazepines may not present as much risk as chronic therapy. Exceptions: ALPRAZolam. Monitor therapy
Betrixaban: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Betrixaban. Avoid combination
Bictegravir: Fosphenytoin-Phenytoin may decrease the serum concentration of Bictegravir. Management: When possible consider using an alternative anticonvulsant with concurrent bictegravir, emtricitabine, and tenofovir alafenamide. If the combination must be used, monitor closely for evidence of reduced antiviral effectiveness. Consider therapy modification
Bleomycin: May decrease the serum concentration of Phenytoin. Monitor therapy
Bortezomib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Bortezomib. Avoid combination
Bosutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Bosutinib. Avoid combination
Brentuximab Vedotin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be decreased. Monitor therapy
Brentuximab Vedotin: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Brentuximab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be decreased. Monitor therapy
Brexpiprazole: CYP3A4 Inducers (Strong) may decrease the serum concentration of Brexpiprazole. Management: If brexpiprazole is used together with a strong CYP3A4 inducer, the brexpiprazole dose should gradually be doubled over the course of 1 to 2 weeks. Consider therapy modification
Brigatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Brigatinib. Avoid combination
Brivaracetam: Phenytoin may decrease the serum concentration of Brivaracetam. Brivaracetam may increase the serum concentration of Phenytoin. Monitor therapy
Buprenorphine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Buprenorphine. Monitor therapy
BusPIRone: CYP3A4 Inducers (Strong) may decrease the serum concentration of BusPIRone. Management: Consider alternatives to this combination. If coadministration of these agents is deemed necessary, monitor patients for reduced buspirone effects and increase buspirone doses as needed. Consider therapy modification
Busulfan: Phenytoin may decrease the serum concentration of Busulfan. Monitor therapy
Cabozantinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cabozantinib. Management: Avoid use of strong CYP3A4 inducers with cabozantinib if possible. If combined, cabozantinib dose adjustments are recommended and vary based on the cabozantinib product used and the indication for use. See monograph for details. Consider therapy modification
Calcifediol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Calcifediol. Monitor therapy
Calcium Channel Blockers: May increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Calcium Channel Blockers. Management: Avoid use of nimodipine or nifedipine with phenytoin. Monitor for phenytoin toxicity and/or decreased calcium channel blocker effects with any concurrent use. Exceptions: Clevidipine. Consider therapy modification
Canagliflozin: Phenytoin may decrease the serum concentration of Canagliflozin. Management: Consider increasing canagliflozin dose to 200 mg/day in patients tolerating 100 mg/day. A further increase to 300 mg/day can be considered in patients with an estimated glomerular filtration rate (GFR) of 60 mL/min/1.73 m2 or greater. Consider therapy modification
Cannabidiol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cannabidiol. Monitor therapy
Cannabis: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cannabis. More specifically, tetrahydrocannabinol and cannabidiol serum concentrations may be decreased. Monitor therapy
CarBAMazepine: May decrease the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of CarBAMazepine. CarBAMazepine may increase the serum concentration of Phenytoin. Possibly by competitive inhibition at sites of metabolism. Consider therapy modification
Carbonic Anhydrase Inhibitors: May enhance the adverse/toxic effect of Fosphenytoin-Phenytoin. Specifically, the risk for osteomalacia or rickets may be increased. Exceptions: Brinzolamide; Dorzolamide. Monitor therapy
Cariprazine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cariprazine. Avoid combination
Caspofungin: Inducers of Drug Clearance may decrease the serum concentration of Caspofungin. Management: Consider using an increased caspofungin dose of 70 mg daily in adults (or 70 mg/m2, up to a maximum of 70 mg, daily in pediatric patients) when coadministered with known inducers of drug clearance. Consider therapy modification
CeFAZolin: May decrease the protein binding of Phenytoin. Monitor therapy
Celiprolol: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Celiprolol. Monitor therapy
Cenobamate: Fosphenytoin-Phenytoin may decrease the serum concentration of Cenobamate. Cenobamate may increase the serum concentration of Fosphenytoin-Phenytoin. Management: Gradually reduce the dose of fosphenytoin/phenytoin by up to 50% as the dose of cenobamate is being titrated up. Monitor phenytoin levels closely. Consider therapy modification
Ceritinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ceritinib. Avoid combination
Chloramphenicol (Systemic): Phenytoin may decrease the serum concentration of Chloramphenicol (Systemic). Phenytoin may increase the serum concentration of Chloramphenicol (Systemic). Chloramphenicol (Systemic) may increase the serum concentration of Phenytoin. Monitor therapy
Chlorpheniramine: May increase the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
ChlorproPAMIDE: CYP3A4 Inducers (Strong) may decrease the serum concentration of ChlorproPAMIDE. Monitor therapy
Cimetidine: May enhance the adverse/toxic effect of Fosphenytoin-Phenytoin. Cimetidine may increase the serum concentration of Fosphenytoin-Phenytoin. Management: Consider using an alternative H2-antagonist to avoid this interaction. Monitor for toxic effects of hydantoin anticonvulsants if cimetidine is initiated/dose increased. Consider therapy modification
Ciprofloxacin (Systemic): May diminish the therapeutic effect of Phenytoin. Ciprofloxacin (Systemic) may decrease the serum concentration of Phenytoin. Monitor therapy
Cladribine: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Cladribine. Monitor therapy
Clarithromycin: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Clarithromycin. Clarithromycin may increase the serum concentration of CYP3A4 Inducers (Strong). CYP3A4 Inducers (Strong) may decrease the serum concentration of Clarithromycin. Management: Consider alternative antimicrobial therapy for patients receiving a CYP3A inducer. Drugs that enhance the metabolism of clarithromycin into 14-hydroxyclarithromycin may alter the clinical activity of clarithromycin and may impair clarithromycin efficacy. Consider therapy modification
Clindamycin (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Clindamycin (Systemic). Refer to the specific clindamycin (systemic) - rifampin drug interaction monograph for information concerning that combination. Monitor therapy
ClonazePAM: Phenytoin may decrease the serum concentration of ClonazePAM. Clonazepam may also alter concentrations of Phenytoin. Monitor therapy
CloZAPine: CYP3A4 Inducers (Strong) may decrease the serum concentration of CloZAPine. Avoid combination
Cobicistat: Fosphenytoin-Phenytoin may decrease the serum concentration of Cobicistat. Avoid combination
Cobimetinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Cobimetinib. Avoid combination
Codeine: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Codeine. Monitor therapy
Colesevelam: May decrease the serum concentration of Phenytoin. Management: Administer phenytoin at least 4 hours prior to colesevelam. Consider therapy modification
Copanlisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Copanlisib. Avoid combination
Corticosteroids (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Corticosteroids (Systemic). Exceptions: Hydrocortisone (Systemic); PrednisoLONE (Systemic); PredniSONE. Monitor therapy
Cosyntropin: May enhance the hepatotoxic effect of Phenytoin. Monitor therapy
Crizotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Crizotinib. Avoid combination
CycloSPORINE (Systemic): Phenytoin may increase the metabolism of CycloSPORINE (Systemic). Consider therapy modification
CYP2C19 Inducers (Moderate): May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Monitor therapy
CYP2C19 Inducers (Strong): May increase the metabolism of CYP2C19 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Consider therapy modification
CYP2C19 Inhibitors (Moderate): May decrease the metabolism of CYP2C19 Substrates (High risk with Inhibitors). Monitor therapy
CYP2C9 Inhibitors (Moderate): May decrease the metabolism of CYP2C9 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Substrates (High risk with Inducers): CYP3A4 Inducers (Strong) may increase the metabolism of CYP3A4 Substrates (High risk with Inducers). Management: Consider an alternative for one of the interacting drugs. Some combinations may be specifically contraindicated. Consult appropriate manufacturer labeling. Exceptions: Benzhydrocodone; Buprenorphine; CarBAMazepine; Etizolam; HYDROcodone; Mirtazapine; TraMADol; Zolpidem. Consider therapy modification
Dabigatran Etexilate: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Dabigatran Etexilate. Management: Avoid concurrent use of dabigatran with P-glycoprotein inducers whenever possible. Avoid combination
Dabrafenib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C9 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2C19 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C19 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Daclatasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Daclatasvir. Avoid combination
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Darolutamide: Inducers of CYP3A4 (Strong) and P-glycoprotein may decrease the serum concentration of Darolutamide. Avoid combination
Darunavir: May decrease the serum concentration of Phenytoin. Monitor therapy
Dasabuvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dasabuvir. Avoid combination
Dasatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dasatinib. Management: Avoid when possible. If such a combination cannot be avoided, consider increasing dasatinib dose and monitor clinical response and toxicity closely. Consider therapy modification
Deferasirox: Phenytoin may decrease the serum concentration of Deferasirox. Management: Avoid combination when possible; if the combination must be used, consider a 50% increase in initial deferasirox dose, with monitoring of serum ferritin concentrations and clinical responses to guide further dosing. Consider therapy modification
Deflazacort: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Deflazacort. Avoid combination
Delamanid: CYP3A4 Inducers (Strong) may decrease the serum concentration of Delamanid. Avoid combination
Delavirdine: Phenytoin may decrease the serum concentration of Delavirdine. Delavirdine may increase the serum concentration of Phenytoin. Avoid combination
DexAMETHasone (Systemic): Phenytoin may decrease the serum concentration of DexAMETHasone (Systemic). DexAMETHasone (Systemic) may decrease the serum concentration of Phenytoin. DexAMETHasone (Systemic) may increase the serum concentration of Phenytoin. Management: Consider dexamethasone dose increases when combined with phenytoin and monitor closely for reduced steroid efficacy. Monitor phenytoin levels closely when combined with dexamethasone, both increased and decreased phenytoin levels have been reported. Consider therapy modification
Dexketoprofen: May enhance the adverse/toxic effect of Fosphenytoin-Phenytoin. Monitor therapy
Dexmethylphenidate: May increase the serum concentration of Phenytoin. Monitor therapy
Diazoxide: May decrease the serum concentration of Phenytoin. Total phenytoin concentrations may be affected more than free phenytoin concentrations. Monitor therapy
Dienogest: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dienogest. Management: Avoid use of dienogest for contraception when using medications that induce CYP3A4 and for at least 28 days after discontinuation of a CYP3A4 inducer. An alternative form of contraception should be used during this time. Avoid combination
Diethylstilbestrol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Diethylstilbestrol. Monitor therapy
Disopyramide: Phenytoin may decrease the serum concentration of Disopyramide. Monitor therapy
Disulfiram: May increase the serum concentration of Phenytoin. Management: Avoid concomitant use of disulfiram and phenytoin when possible. Phenytoin dose adjustment will likely be necessary when starting and/or stopping concurrent disulfiram. Monitor phenytoin response and concentrations closely. Consider therapy modification
Dolutegravir: Fosphenytoin-Phenytoin may decrease the serum concentration of Dolutegravir. Avoid combination
Doravirine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Doravirine. Avoid combination
Doxercalciferol: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Doxercalciferol. Monitor therapy
Doxofylline: Fosphenytoin-Phenytoin may decrease the serum concentration of Doxofylline. Monitor therapy
DOXOrubicin (Conventional): CYP3A4 Inducers (Strong) may decrease the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to strong CYP3A4 inducers in patients treated with doxorubicin. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
DOXOrubicin (Conventional): P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to P-glycoprotein inducers in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
Doxycycline: Phenytoin may decrease the serum concentration of Doxycycline. Consider therapy modification
Dronabinol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dronabinol. Monitor therapy
Dronedarone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Dronedarone. Avoid combination
Duvelisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Duvelisib. Avoid combination
Edoxaban: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Edoxaban. Monitor therapy
Efavirenz: Phenytoin may decrease the serum concentration of Efavirenz. Efavirenz may increase the serum concentration of Phenytoin. Consider therapy modification
Elagolix: CYP3A4 Inducers (Strong) may decrease the serum concentration of Elagolix. Monitor therapy
Elbasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Elbasvir. Avoid combination
Elexacaftor, Tezacaftor, and Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Elexacaftor, Tezacaftor, and Ivacaftor. Avoid combination
Eliglustat: CYP3A4 Inducers (Strong) may decrease the serum concentration of Eliglustat. Avoid combination
Elvitegravir: Fosphenytoin-Phenytoin may decrease the serum concentration of Elvitegravir. Avoid combination
Encorafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Encorafenib. Avoid combination
Enfortumab Vedotin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Enfortumab Vedotin. Specifically, concentrations of the active monomethyl auristatin E (MMAE) component may be decreased. Monitor therapy
Entrectinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Entrectinib. Avoid combination
Enzalutamide: May decrease the serum concentration of Fosphenytoin-Phenytoin. Avoid combination
Eravacycline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Eravacycline. Management: Increase the eravacycline dose to 1.5 mg/kg every 12 hours when combined with strong CYP3A4 inducers. Consider therapy modification
Erdafitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Erdafitinib. Avoid combination
Erlotinib: May increase the serum concentration of Fosphenytoin-Phenytoin. Fosphenytoin-Phenytoin may decrease the serum concentration of Erlotinib. Management: Avoid use of erlotinib with phenytoin when possible. If required, increase erlotinib dose by 50 mg increments at 2 week intervals, as tolerated, to a max of 450 mg/day. Avoid combination
Eslicarbazepine: Phenytoin may decrease the serum concentration of Eslicarbazepine. Eslicarbazepine may increase the serum concentration of Phenytoin. Monitor therapy
Estriol (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Estriol (Systemic). Monitor therapy
Estriol (Topical): CYP3A4 Inducers (Strong) may decrease the serum concentration of Estriol (Topical). Monitor therapy
Estrogen Derivatives (Contraceptive): Phenytoin may diminish the therapeutic effect of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Use of an alternative, nonhormonal means of contraception is recommended. Consider therapy modification
Ethosuximide: May enhance the CNS depressant effect of Phenytoin. Phenytoin may decrease the serum concentration of Ethosuximide. Ethosuximide may increase the serum concentration of Phenytoin. Monitor therapy
Etizolam: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etizolam. Monitor therapy
Etoposide: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etoposide. Management: When possible, seek alternatives to strong CYP3A4-inducing medications in patients receiving etoposide. If combined, monitor patients closely for diminished etoposide response and need for etoposide dose increases. Consider therapy modification
Etoposide Phosphate: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etoposide Phosphate. Management: When possible, seek alternatives to strong CYP3A4-inducing medications in patients receiving etoposide phosphate. If these combinations cannot be avoided, monitor patients closely for diminished etoposide phosphate response. Consider therapy modification
Etravirine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Etravirine. Avoid combination
Everolimus: CYP3A4 Inducers (Strong) may decrease the serum concentration of Everolimus. Management: Avoid concurrent use of strong CYP3A4 inducers if possible. If coadministration cannot be avoided, double the daily dose of everolimus using increments of 5 mg or less. Monitor everolimus serum concentrations closely when indicated. Consider therapy modification
Evogliptin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Evogliptin. Monitor therapy
Exemestane: CYP3A4 Inducers (Strong) may decrease the serum concentration of Exemestane. Management: Exemestane U.S. product labeling recommends using an increased dose (50 mg/day) in patients receiving concurrent strong CYP3A4 inducers. The Canadian product labeling does not recommend a dose adjustment with concurrent use of strong CYP3A4 inducers. Consider therapy modification
Ezogabine: Fosphenytoin-Phenytoin may decrease the serum concentration of Ezogabine. Management: Consider increasing the ezogabine dose when adding phenytoin. Patients using this combination should be monitored closely for evidence of adequate ezogabine therapy. Consider therapy modification
Fedratinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Fedratinib. Avoid combination
Felbamate: May increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Felbamate. Management: Decreased phenytoin dose will likely be needed when adding felbamate; some reports suggest an empiric 20% decrease in phenytoin dose. Additional reductions may be needed if felbamate dose is increased or as otherwise guided by monitoring. Consider therapy modification
FentaNYL: CYP3A4 Inducers (Strong) may decrease the serum concentration of FentaNYL. Monitor therapy
Fexinidazole [INT]: May increase the serum concentration of Products Containing Propylene Glycol. Avoid combination
Flibanserin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Flibanserin. Avoid combination
Fluconazole: May increase the serum concentration of Phenytoin. Consider therapy modification
Flunarizine: Phenytoin may decrease the serum concentration of Flunarizine. Monitor therapy
Fluorouracil (Topical): May increase the serum concentration of Phenytoin. Monitor therapy
Fluorouracil Products: May increase the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
FLUoxetine: May increase the serum concentration of Phenytoin. Monitor therapy
FluvoxaMINE: May increase the serum concentration of Phenytoin. Monitor therapy
Folic Acid: May decrease the serum concentration of Phenytoin. Monitor therapy
Fosamprenavir: May decrease the serum concentration of Phenytoin. Specifically, fosamprenavir boosted with ritonavir may decrease phenytoin concentrations. Phenytoin may decrease the serum concentration of Fosamprenavir. Specifically, phenytoin may decrease the concentration of the active metabolite amprenavir. Monitor therapy
Fosaprepitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Fosaprepitant. Specifically, CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite aprepitant. Avoid combination
Fosnetupitant: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Fosnetupitant. Avoid combination
Fostamatinib: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Fostamatinib. Avoid combination
Fotemustine: Fosphenytoin-Phenytoin may decrease the serum concentration of Fotemustine. Fotemustine may decrease the serum concentration of Fosphenytoin-Phenytoin. Specifically, fotemustine may decrease concentrations of orally administered phenytoin. Avoid combination
Gefitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Gefitinib. Management: In the absence of severe adverse reactions, increase gefitinib dose to 500 mg daily in patients receiving strong CYP3A4 inducers; resume 250 mg dose 7 days after discontinuation of the strong inducer. Carefully monitor clinical response. Consider therapy modification
Gemigliptin: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Gemigliptin. CYP3A4 Inducers (Strong) may decrease the serum concentration of Gemigliptin. Avoid combination
Gestrinone: Fosphenytoin-Phenytoin may decrease the serum concentration of Gestrinone. Monitor therapy
Gilteritinib: Combined Inducers of CYP3A4 and P-glycoprotein may decrease the serum concentration of Gilteritinib. Avoid combination
Glasdegib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Glasdegib. Avoid combination
Glecaprevir and Pibrentasvir: Fosphenytoin-Phenytoin may decrease the serum concentration of Glecaprevir and Pibrentasvir. Avoid combination
Grazoprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Grazoprevir. Avoid combination
GuanFACINE: CYP3A4 Inducers (Strong) may decrease the serum concentration of GuanFACINE. Management: Increase the guanfacine dose by up to double when initiating guanfacine in a patient taking a strong CYP3A4 inducer. Increase guanfacine dose gradually over 1 to 2 weeks if initiating strong CYP3A4 inducer therapy in a patient already taking guanfacine. Consider therapy modification
Halothane: May increase the serum concentration of Phenytoin. Monitor therapy
HMG-CoA Reductase Inhibitors (Statins): Phenytoin may decrease the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Exceptions: Pitavastatin; Rosuvastatin. Consider therapy modification
HYDROcodone: CYP3A4 Inducers (Strong) may decrease the serum concentration of HYDROcodone. Monitor therapy
Hydrocortisone (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of Hydrocortisone (Systemic). Monitor therapy
Ibrutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ibrutinib. Avoid combination
Idelalisib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Idelalisib. Avoid combination
Ifosfamide: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Ifosfamide. CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Ifosfamide. Monitor therapy
Imatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Imatinib. Management: Avoid concurrent use of imatinib with strong CYP3A4 inducers when possible. If such a combination must be used, increase imatinib dose by at least 50% and monitor the patient's clinical response closely. Consider therapy modification
Irinotecan Products: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Irinotecan Products. Specifically, serum concentrations of SN-38 may be reduced. CYP3A4 Inducers (Strong) may decrease the serum concentration of Irinotecan Products. Avoid combination
Isavuconazonium Sulfate: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Isavuconazonium Sulfate. Specifically, CYP3A4 Inducers (Strong) may decrease isavuconazole serum concentrations. Avoid combination
Isoniazid: May increase the serum concentration of Phenytoin. Management: Consider alternatives. If concomitant therapy cannot be avoided, monitor for increased phenytoin concentrations/effects with isoniazid initiation/dose increase, or decreased concentrations/effects with isoniazid discontinuation/dose decrease. Consider therapy modification
Istradefylline: CYP3A4 Inducers (Strong) may decrease the serum concentration of Istradefylline. Avoid combination
Itraconazole: CYP3A4 Inducers (Strong) may decrease the serum concentration of Itraconazole. Avoid combination
Ivabradine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ivabradine. Avoid combination
Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ivacaftor. Avoid combination
Ivosidenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ivosidenib. Avoid combination
Ixabepilone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ixabepilone. Management: Avoid this combination whenever possible. If this combination must be used, a gradual increase in ixabepilone dose from 40 mg/m2 to 60 mg/m2 (given as a 4-hour infusion), as tolerated, should be considered. Consider therapy modification
Ixazomib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ixazomib. Avoid combination
Lacosamide: Antiepileptic Agents (Sodium Channel Blockers) may enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
LamoTRIgine: Phenytoin may decrease the serum concentration of LamoTRIgine. Consider therapy modification
Lapatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lapatinib. Management: If therapy overlap cannot be avoided, consider titrating lapatinib gradually from 1,250 mg/day up to 4,500 mg/day (HER2 positive metastatic breast cancer) or 1,500 mg/day up to 5,500 mg/day (hormone receptor/HER2 positive breast cancer) as tolerated. Avoid combination
Larotrectinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Larotrectinib. Management: Avoid use of strong CYP3A4 inducers with larotrectinib. If this combination cannot be avoided, double the larotrectinib dose. Reduced to previous dose after stopping the inducer after a period of 3 to 5 times the inducer half-life. Consider therapy modification
Ledipasvir: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Ledipasvir. Avoid combination
Lefamulin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin with strong CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Lefamulin. Management: Avoid concomitant use of lefamulin with P-glycoprotein/ABCB1 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin (Intravenous): CYP3A4 Inducers (Strong) may decrease the serum concentration of Lefamulin (Intravenous). Management: Avoid concomitant use of lefamulin intravenous infusion with strong CYP3A4 inducers unless the benefits outweigh the risks. Consider therapy modification
Lefamulin (Intravenous): P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Lefamulin (Intravenous). Management: Avoid concomitant use of lefamulin (intravenous) with P-glycoprotein/ABCB1 inducers unless the benefits outweigh the risks. Consider therapy modification
Lemborexant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lemborexant. Avoid combination
Letermovir: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Letermovir. Avoid combination
Letermovir: May increase the serum concentration of UGT1A1 Inducers. Avoid combination
Leucovorin Calcium-Levoleucovorin: May decrease the serum concentration of Phenytoin. Monitor therapy
LevETIRAcetam: Fosphenytoin-Phenytoin may decrease the serum concentration of LevETIRAcetam. Monitor therapy
Levodopa-Containing Products: Fosphenytoin-Phenytoin may diminish the therapeutic effect of Levodopa-Containing Products. Monitor therapy
Levomefolate: May decrease the serum concentration of Phenytoin. Monitor therapy
Levomethadone: Phenytoin may decrease the serum concentration of Levomethadone. Monitor therapy
LinaGLIPtin: CYP3A4 Inducers (Strong) may decrease the serum concentration of LinaGLIPtin. Management: Strongly consider using an alternative to any strong CYP3A4 inducer in patients who are being treated with linagliptin. If this combination is used, monitor patients closely for evidence of reduced linagliptin effectiveness. Consider therapy modification
LinaGLIPtin: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of LinaGLIPtin. Management: Strongly consider using an alternative to any strong P-glycoprotein inducer in patients who are being treated with linagliptin. If this combination is used, monitor patients closely for evidence of reduced linagliptin effectiveness. Consider therapy modification
Lithium: Phenytoin may enhance the adverse/toxic effect of Lithium. Monitor therapy
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Loop Diuretics: Phenytoin may diminish the diuretic effect of Loop Diuretics. Monitor therapy
Lopinavir: Phenytoin may decrease the serum concentration of Lopinavir. Lopinavir may decrease the serum concentration of Phenytoin. Management: The manufacturer of lopinavir/ritonavir recommends avoiding once-daily administration if used together with phenytoin. Consider therapy modification
Lorlatinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lorlatinib. Avoid combination
Lumacaftor and Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lumacaftor and Ivacaftor. Specifically, the serum concentration of ivacaftor may be decreased. Avoid combination
Lumateperone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lumateperone. Avoid combination
Lumefantrine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lumefantrine. Avoid combination
Lurasidone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Lurasidone. Avoid combination
Macimorelin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Macimorelin. Avoid combination
Macitentan: CYP3A4 Inducers (Strong) may decrease the serum concentration of Macitentan. Avoid combination
Manidipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Manidipine. Management: Consider avoiding concomitant use of manidipine and strong CYP3A4 inducers. If combined, monitor closely for decreased manidipine effects and loss of efficacy. Increased manidipine doses may be required. Consider therapy modification
Maraviroc: CYP3A4 Inducers (Strong) may decrease the serum concentration of Maraviroc. Management: Increase maraviroc adult dose to 600 mg twice daily when used with strong CYP3A4 inducers. This does not apply to patients also receiving strong CYP3A4 inhibitors. Do not use maraviroc with strong CYP3A4 inducers in patients with CrCl less than 30 mL/min. Consider therapy modification
Mebendazole: Phenytoin may decrease the serum concentration of Mebendazole. Monitor therapy
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Meperidine: Phenytoin may decrease the serum concentration of Meperidine. Monitor therapy
Methadone: Phenytoin may decrease the serum concentration of Methadone. Monitor therapy
Methotrexate: May decrease the serum concentration of Fosphenytoin-Phenytoin. Fosphenytoin-Phenytoin may increase the serum concentration of Methotrexate. Specifically, fosphenytoin-phenytoin may displace methotrexate from serum proteins, increasing the concentration of free, unbound drug. Monitor therapy
Methylfolate: May decrease the serum concentration of Phenytoin. Monitor therapy
Methylphenidate: May increase the serum concentration of Phenytoin. Monitor therapy
MethylPREDNISolone: CYP3A4 Inducers (Strong) may decrease the serum concentration of MethylPREDNISolone. Management: Consider methylprednisolone dose increases in patients receiving strong CYP3A4 inducers and monitor closely for reduced steroid efficacy. Consider therapy modification
MetroNIDAZOLE (Systemic): Phenytoin may decrease the serum concentration of MetroNIDAZOLE (Systemic). MetroNIDAZOLE (Systemic) may increase the serum concentration of Phenytoin. Monitor therapy
MetyraPONE: Phenytoin may decrease the serum concentration of MetyraPONE. The oral metyrapone test would thus be unreliable unless the metapyrone dosage was substantially increased (e.g., 750 mg every 2 hours). Consider therapy modification
Mexiletine: Phenytoin may decrease the serum concentration of Mexiletine. Monitor therapy
Mianserin: May diminish the therapeutic effect of Phenytoin. Phenytoin may decrease the serum concentration of Mianserin. Monitor therapy
Miconazole (Oral): May increase the serum concentration of Phenytoin. Monitor therapy
Midostaurin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Midostaurin. Avoid combination
MiFEPRIStone: CYP3A4 Inducers (Strong) may decrease the serum concentration of MiFEPRIStone. Avoid combination
Mirodenafil: CYP3A4 Inducers (Strong) may decrease the serum concentration of Mirodenafil. Management: Consider avoiding the concomitant use of mirodenafil and strong CYP3A4 inducers. If combined, monitor for decreased mirodenafil effects. Mirodenafil dose increases may be required to achieve desired effects. Consider therapy modification
Mirtazapine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Mirtazapine. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May decrease the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
Naldemedine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Naldemedine. Avoid combination
Naloxegol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Naloxegol. Avoid combination
Nelfinavir: May decrease the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Nelfinavir. Monitor therapy
Neratinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Neratinib. Avoid combination
Netupitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Netupitant. Avoid combination
Neuromuscular-Blocking Agents (Nondepolarizing): Fosphenytoin-Phenytoin may diminish the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). Fosphenytoin-Phenytoin may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). Fosphenytoin-Phenytoin may decrease the serum concentration of Neuromuscular-Blocking Agents (Nondepolarizing). Monitor therapy
NIFEdipine: May increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of NIFEdipine. Avoid combination
Nilotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Nilotinib. Avoid combination
NiMODipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of NiMODipine. Avoid combination
Nintedanib: Combined Inducers of CYP3A4 and P-glycoprotein may decrease the serum concentration of Nintedanib. Avoid combination
Nisoldipine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Nisoldipine. Avoid combination
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
OLANZapine: CYP1A2 Inducers (Weak) may decrease the serum concentration of OLANZapine. Monitor therapy
Olaparib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Olaparib. Avoid combination
Omeprazole: Phenytoin may decrease the serum concentration of Omeprazole. Omeprazole may increase the serum concentration of Phenytoin. Monitor therapy
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
Osimertinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Osimertinib. Consider therapy modification
OXcarbazepine: Fosphenytoin-Phenytoin may decrease serum concentrations of the active metabolite(s) of OXcarbazepine. Specifically, concentrations of the major active 10-monohydroxy metabolite may be reduced. OXcarbazepine may increase the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
Palbociclib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Palbociclib. Avoid combination
Paliperidone: Inducers of CYP3A4 (Strong) and P-glycoprotein may decrease the serum concentration of Paliperidone. Management: Avoid using the 3-month extended-release injectable suspension (Invega Trinza) with inducers of both CYP3A4 and P-glycoprotein during the 3-month dosing interval if possible. If combination is necessary, consider using extended-release tablets. Consider therapy modification
Panobinostat: CYP3A4 Inducers (Strong) may decrease the serum concentration of Panobinostat. Avoid combination
PAZOPanib: CYP3A4 Inducers (Strong) may decrease the serum concentration of PAZOPanib. Avoid combination
Perampanel: Phenytoin may decrease the serum concentration of Perampanel. Management: Increase the perampanel starting dose to 4 mg/day when perampanel is used with phenytoin/fosphenytoin. Patients receiving this combination should be followed closely for response, especially with any changes to phenytoin/fosphenytoin therapy. Consider therapy modification
Pexidartinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pexidartinib. Avoid combination
P-glycoprotein/ABCB1 Substrates: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Exceptions: Betrixaban; Edoxaban. Monitor therapy
PHENobarbital: Phenytoin may enhance the CNS depressant effect of PHENobarbital. PHENobarbital may decrease the serum concentration of Phenytoin. Phenytoin may increase the serum concentration of PHENobarbital. Monitor therapy
Phenylbutazone: May increase the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
Pimavanserin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pimavanserin. Avoid combination
Piperaquine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Piperaquine. Avoid combination
Pitolisant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pitolisant. Management: For patients who are stable on pitolisant doses of 8.9 mg or 17.8 mg/day and who are also taking a strong CYP3A4 inducer, increase the pitolisant dose over 7 days to double the original dose (ie, to either 17.8 mg/day or 35.6 mg/day, respectively). Consider therapy modification
Platinum Derivatives: May decrease the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
Polatuzumab Vedotin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Polatuzumab Vedotin. Exposure to unconjugated MMAE, the cytotoxic small molecule component of polatuzumab vedotin, may be decreased. Monitor therapy
PONATinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of PONATinib. Avoid combination
Praziquantel: CYP3A4 Inducers (Strong) may decrease the serum concentration of Praziquantel. Management: Use of praziquantel with strong CYP3A4 inducers is contraindicated. Discontinue rifampin 4 weeks prior to initiation of praziquantel therapy. Rifampin may be resumed the day following praziquantel completion. Avoid combination
PrednisoLONE (Systemic): CYP3A4 Inducers (Strong) may decrease the serum concentration of PrednisoLONE (Systemic). Monitor therapy
PredniSONE: CYP3A4 Inducers (Strong) may decrease the serum concentration of PredniSONE. Monitor therapy
Pretomanid: CYP3A4 Inducers (Strong) may decrease the serum concentration of Pretomanid. Avoid combination
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Primidone: Phenytoin may increase the metabolism of Primidone. The ratio of primidone:phenobarbital is thus changed. Monitor therapy
Progestins (Contraceptive): Phenytoin may diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Contraceptive failure is possible. Use of an alternative, nonhormonal contraceptive is recommended. Consider therapy modification
Propacetamol: Fosphenytoin-Phenytoin may decrease serum concentrations of the active metabolite(s) of Propacetamol. Specifically, serum concentrations of acetaminophen may be decreased (leading to decreased efficacy), but the formation of its toxic N-acetyl-p-benzoquinone imine (NAPQI) metabolite may be increased (leading to increased hepatotoxicity). Monitor therapy
Propafenone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Propafenone. Monitor therapy
Pyridoxine: May increase the metabolism of Phenytoin. This is most apparent in high pyridoxine doses (e.g., 80 mg to 200 mg daily) Monitor therapy
QUEtiapine: CYP3A4 Inducers (Strong) may decrease the serum concentration of QUEtiapine. Management: An increase in quetiapine dose (as much as 5 times the regular dose) may be required to maintain therapeutic benefit. Reduce the quetiapine dose back to the previous/regular dose within 7-14 days of discontinuing the inducer. Consider therapy modification
QuiNIDine: Phenytoin may decrease the serum concentration of QuiNIDine. Monitor therapy
QuiNINE: Phenytoin may decrease the serum concentration of QuiNINE. Consider therapy modification
Radotinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Radotinib. Management: Consider alternatives to this combination when possible as the risk of radotinib treatment failure may be increased. Consider therapy modification
Ramelteon: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ramelteon. Monitor therapy
Ranolazine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ranolazine. Avoid combination
Reboxetine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Reboxetine. Monitor therapy
Regorafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Regorafenib. Avoid combination
Ribociclib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ribociclib. Avoid combination
RifAMPin: May decrease the serum concentration of Phenytoin. Management: Seek alternatives when possible. If used together, monitor closely for decreased serum phenytoin concentrations following rifampin initiation/dose increase, or increased concentrations and toxic effects following rifampin discontinuation/dose decrease. Consider therapy modification
Rifapentine: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Rilpivirine: Phenytoin may decrease the serum concentration of Rilpivirine. Avoid combination
RisperiDONE: CYP3A4 Inducers (Strong) may decrease the serum concentration of RisperiDONE. Management: Consider increasing the dose of oral risperidone (to no more than double the original dose) if a strong CYP3A4 inducer is initiated. For patients on IM risperidone, consider an increased IM dose or supplemental doses of oral risperidone. Consider therapy modification
Ritonavir: Phenytoin may decrease the serum concentration of Ritonavir. Ritonavir may decrease the serum concentration of Phenytoin. Consider therapy modification
Rivaroxaban: CYP3A4 Inducers (Strong) may decrease the serum concentration of Rivaroxaban. Avoid combination
Roflumilast: CYP3A4 Inducers (Strong) may decrease the serum concentration of Roflumilast. Management: Roflumilast U.S. prescribing information recommends against combining strong CYP3A4 inducers with roflumilast. The Canadian product monograph makes no such recommendation but notes that such agents may reduce roflumilast therapeutic effects. Avoid combination
Rolapitant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Rolapitant. Management: Avoid rolapitant use in patients requiring chronic administration of strong CYP3A4 inducers. Monitor for reduced rolapitant response and the need for alternative or additional antiemetic therapy even with shorter-term use of such inducers. Consider therapy modification
RomiDEPsin: CYP3A4 Inducers (Strong) may decrease the serum concentration of RomiDEPsin. Avoid combination
Rufinamide: May increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Rufinamide. Monitor therapy
Ruxolitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ruxolitinib. Monitor therapy
SAXagliptin: CYP3A4 Inducers (Strong) may decrease the serum concentration of SAXagliptin. Monitor therapy
Sertraline: May increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Sertraline. Monitor therapy
Simeprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Simeprevir. Avoid combination
Sirolimus: CYP3A4 Inducers (Strong) may decrease the serum concentration of Sirolimus. Management: Avoid concomitant use of strong CYP3A4 inducers and sirolimus if possible. If combined, monitor for reduced serum sirolimus concentrations. Sirolimus dose increases will likely be necessary to prevent subtherapeutic sirolimus levels. Consider therapy modification
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Sofosbuvir: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Sofosbuvir. Avoid combination
Sonidegib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Sonidegib. Avoid combination
SORAfenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of SORAfenib. Avoid combination
Stiripentol: May decrease the serum concentration of Phenytoin. Avoid combination
SUFentanil: CYP3A4 Inducers (Strong) may decrease the serum concentration of SUFentanil. Monitor therapy
SulfADIAZINE: May increase the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
Sulfamethoxazole: May increase the serum concentration of Phenytoin. Consider therapy modification
Sulfinpyrazone: May increase the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
Sulthiame: May increase the serum concentration of Fosphenytoin-Phenytoin. Monitor therapy
SUNItinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of SUNItinib. Management: Avoid when possible. If such a combination cannot be avoided, sunitinib dose increases are recommended, and vary by indication. See full monograph for details. Consider therapy modification
Tacrolimus (Systemic): Phenytoin may decrease the serum concentration of Tacrolimus (Systemic). Tacrolimus (Systemic) may increase the serum concentration of Phenytoin. Monitor therapy
Tadalafil: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tadalafil. Management: Erectile dysfunction: monitor for decreased effectiveness - no standard dose adjustments recommended. Avoid use of tadalafil for pulmonary arterial hypertension in patients receiving a strong CYP3A4 inducer. Consider therapy modification
Tamoxifen: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Tamoxifen. CYP3A4 Inducers (Strong) may decrease the serum concentration of Tamoxifen. Management: Consider alternatives to concomitant use of strong CYP3A4 inducers and tamoxifen. If the combination cannot be avoided, monitor for reduced therapeutic effects of tamoxifen. Consider therapy modification
Tasimelteon: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tasimelteon. Avoid combination
Tazemetostat: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tazemetostat. Avoid combination
Telithromycin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Telithromycin. Avoid combination
Temsirolimus: Phenytoin may decrease the serum concentration of Temsirolimus. Concentrations of the active metabolite, sirolimus, are also likely to be decreased (and maybe to an even greater degree). Management: Temsirolimus prescribing information recommends against coadministration with strong CYP3A4 inducers such as phenytoin; however, if concurrent therapy is necessary, an increase in temsirolimus adult dose to 50 mg/week should be considered. Consider therapy modification
Teniposide: Phenytoin may decrease the serum concentration of Teniposide. Management: Consider alternatives to combined treatment with phenytoin and teniposide due to the potential for decreased teniposide concentrations. If the combination cannot be avoided, monitor teniposide response closely. Consider therapy modification
Tenofovir Alafenamide: Fosphenytoin-Phenytoin may decrease the serum concentration of Tenofovir Alafenamide. Avoid combination
Tetrahydrocannabinol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tetrahydrocannabinol. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tetrahydrocannabinol and Cannabidiol. Monitor therapy
Tezacaftor and Ivacaftor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tezacaftor and Ivacaftor. Avoid combination
Theophylline Derivatives: Phenytoin may decrease the serum concentration of Theophylline Derivatives. Theophylline Derivatives may decrease the serum concentration of Phenytoin. Management: Seek alternatives when possible. If used together, monitor for decreased concentrations/effects of phenytoin or theophylline if the other agent is initiated/dose increased, or increased concentrations/effects if the other is discontinued/dose decreased. Exceptions: Dyphylline. Consider therapy modification
Thiotepa: CYP3A4 Inducers (Strong) may increase serum concentrations of the active metabolite(s) of Thiotepa. CYP3A4 Inducers (Strong) may decrease the serum concentration of Thiotepa. Management: Thiotepa prescribing information recommends avoiding concomitant use of thiotepa and strong CYP3A4 inducers. If concomitant use is unavoidable, monitor for adverse effects. Consider therapy modification
Thiothixene: Fosphenytoin-Phenytoin may decrease the serum concentration of Thiothixene. Monitor therapy
Thyroid Products: Phenytoin may decrease the serum concentration of Thyroid Products. Phenytoin may also displace thyroid hormones from protein binding sites. Monitor therapy
TiaGABine: CYP3A4 Inducers (Strong) may decrease the serum concentration of TiaGABine. Management: Approximately 2-fold higher tiagabine doses and a more rapid dose titration will likely be required in patients concomitantly taking a strong CYP3A4 inducer. Consider therapy modification
Ticagrelor: CYP3A4 Inducers (Strong) may decrease serum concentrations of the active metabolite(s) of Ticagrelor. CYP3A4 Inducers (Strong) may decrease the serum concentration of Ticagrelor. Avoid combination
Ticlopidine: May increase the serum concentration of Phenytoin. Monitor therapy
Tipranavir: Phenytoin may decrease the serum concentration of Tipranavir. Tipranavir may decrease the serum concentration of Phenytoin. Consider therapy modification
Tofacitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tofacitinib. Avoid combination
TOLBUTamide: May decrease the protein binding of Fosphenytoin-Phenytoin. Specifically concentrations of free phenytoin may be increased. Monitor therapy
Tolvaptan: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tolvaptan. Management: If concurrent use is necessary, increased doses of tolvaptan (with close monitoring for toxicity and clinical response) may be needed. Avoid combination
Topiramate: May increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Topiramate. Monitor therapy
Topotecan: Fosphenytoin-Phenytoin may decrease the serum concentration of Topotecan. Management: Monitor topotecan response closely, and consider alternatives to phenytoin when possible. No specific guidelines for topotecan dose adjustment are available. Consider therapy modification
Toremifene: CYP3A4 Inducers (Strong) may decrease the serum concentration of Toremifene. Avoid combination
Trabectedin: CYP3A4 Inducers (Strong) may decrease the serum concentration of Trabectedin. Avoid combination
TraMADol: CYP3A4 Inducers (Strong) may decrease the serum concentration of TraMADol. Monitor therapy
TraZODone: Phenytoin may decrease the serum concentration of TraZODone. TraZODone may increase the serum concentration of Phenytoin. Monitor therapy
Trimethoprim: May increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Trimethoprim. Management: Consider alternatives to this combination when possible, to avoid potential decreased trimethoprim efficacy and increased phenytoin concentrations/effects. Monitor patients receiving this combination closely for both of these possible effects. Consider therapy modification
Tropisetron: CYP3A4 Inducers (Strong) may decrease the serum concentration of Tropisetron. Monitor therapy
Ubrogepant: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ubrogepant. Avoid combination
Udenafil: CYP3A4 Inducers (Strong) may decrease the serum concentration of Udenafil. Monitor therapy
Ulipristal: CYP3A4 Inducers (Strong) may decrease the serum concentration of Ulipristal. Avoid combination
Upadacitinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Upadacitinib. Avoid combination
Valbenazine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Valbenazine. Avoid combination
Valproate Products: May decrease the protein binding of Fosphenytoin-Phenytoin. This appears to lead to an initial increase in the percentage of unbound (free) phenytoin and to a decrease in total phenytoin concentrations. Whether concentrations of free phenytoin are increased is unclear. With long-term concurrent use, total phenytoin concentrations may increase. Fosphenytoin-Phenytoin may decrease the serum concentration of Valproate Products. Monitor therapy
Vandetanib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vandetanib. Avoid combination
Velpatasvir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Velpatasvir. Avoid combination
Velpatasvir: P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of Velpatasvir. Avoid combination
Vemurafenib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vemurafenib. Management: Avoid concurrent use of vemurafenib with a strong CYP3A4 inducer and replace with another agent when possible. If a strong CYP3A4 inducer is indicated and unavoidable, the dose of vemurafenib may be increased by 240 mg (1 tablet) as tolerated. Consider therapy modification
Venetoclax: CYP3A4 Inducers (Strong) may decrease the serum concentration of Venetoclax. Avoid combination
Vigabatrin: May decrease the serum concentration of Phenytoin. Monitor therapy
Vilazodone: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vilazodone. Management: Consider increasing vilazodone dose by as much as 2-fold (do not exceed 80 mg/day), based on response, in patients receiving strong CYP3A4 inducers for > 14 days. Reduce to the original vilazodone dose over 1-2 weeks after inducer discontinuation. Consider therapy modification
VinCRIStine: Phenytoin may decrease the serum concentration of VinCRIStine. VinCRIStine may decrease the serum concentration of Phenytoin. Management: . Monitor therapy
VinCRIStine (Liposomal): CYP3A4 Inducers (Strong) may decrease the serum concentration of VinCRIStine (Liposomal). Avoid combination
VinCRIStine (Liposomal): P-glycoprotein/ABCB1 Inducers may decrease the serum concentration of VinCRIStine (Liposomal). Avoid combination
Vindesine: May decrease the serum concentration of Phenytoin. Monitor therapy
Vinflunine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vinflunine. Avoid combination
Vitamin K Antagonists (eg, warfarin): Phenytoin may enhance the anticoagulant effect of Vitamin K Antagonists. Vitamin K Antagonists may increase the serum concentration of Phenytoin. Management: Anticoagulant dose adjustment will likely be necessary when phenytoin is initiated or discontinued. Monitor patients extra closely (INR and signs/symptoms of bleeding) when using this combination. Consider therapy modification
Vorapaxar: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vorapaxar. Avoid combination
Vortioxetine: CYP3A4 Inducers (Strong) may decrease the serum concentration of Vortioxetine. Management: Consider increasing the vortioxetine dose to no more than 3 times the original dose when used with a strong drug metabolism inducer for more than 14 days. The vortioxetine dose should be returned to normal within 14 days of stopping the strong inducer. Consider therapy modification
Voxelotor: CYP3A4 Inducers (Strong) may decrease the serum concentration of Voxelotor. Management: Avoid concomitant use of voxelotor and strong CYP3A4 inducers. If concomitant use is unavoidable, increase the voxelotor dose to 2,500 mg once daily. Consider therapy modification
Voxilaprevir: CYP3A4 Inducers (Strong) may decrease the serum concentration of Voxilaprevir. Avoid combination
Zaleplon: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zaleplon. Management: Consider the use of an alternative hypnotic that is not metabolized by CYP3A4 in patients receiving strong CYP3A4 inducers. If zalephon is combined with a strong CYP3A4 inducer, monitor for decreased effectiveness of zaleplon. Consider therapy modification
Zanubrutinib: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zanubrutinib. Avoid combination
Zolpidem: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zolpidem. Monitor therapy
Zonisamide: Phenytoin may decrease the serum concentration of Zonisamide. Monitor therapy
Zuclopenthixol: CYP3A4 Inducers (Strong) may decrease the serum concentration of Zuclopenthixol. Monitor therapy
Test Interactions
Falsely high plasma phenytoin concentrations may occur when measured by immunoanalytical techniques (eg, TDX, TDXFLX, Emit 2000). Phenytoin may produce falsely low results for serum concentrations of T4 and T3, and dexamethasone or metyrapone tests. Phenytoin may cause increased serum levels of thyroid-stimulating hormone (TSH; usually in the absence of clinical hypothyroidism).
Adverse Reactions
Frequency not defined:
Cardiovascular: Cardiac arrhythmia, cardiac conduction disturbance (depression), circulatory shock, hypotension, ventricular fibrillation
Central nervous system: Ataxia, cerebral atrophy (elevated serum levels and/or long-term use), cerebral dysfunction (elevated serum levels and/or long-term use), confusion, dizziness, drowsiness, headache, insomnia, nervousness, paresthesia, peripheral neuropathy (associated with chronic treatment), slurred speech, suicidal ideation, suicidal tendencies, twitching, vertigo
Dermatologic: Bullous dermatitis, exfoliative dermatitis, morbilliform rash, scarlatiniform rash, skin or other tissue necrosis, skin rash
Endocrine & metabolic: Decreased T4, increased gamma-glutamyl transferase, vitamin D deficiency (associated with chronic treatment)
Gastrointestinal: Constipation, dysgeusia, gingival hyperplasia, nausea, swelling of lips, vomiting
Genitourinary: Peyronie's disease
Hematologic & oncologic: Macrocytosis, megaloblastic anemia, pseudolymphoma, purpuric dermatitis
Hepatic: Acute hepatic failure, hepatic injury, hepatitis, increased serum alkaline phosphatase, toxic hepatitis
Local: Injection site reaction ("purple glove syndrome;" edema, discoloration, and pain distal to injection site), local inflammation, local irritation, localized tenderness, local tissue necrosis
Neuromuscular & skeletal: Osteomalacia
Ophthalmic: Nystagmus
Miscellaneous: Fever, tissue sloughing
<1%, postmarketing, and/or case reports: Acute generalized exanthematous pustulosis, agranulocytosis, anaphylaxis, angioedema, asterixis, bone fracture, bone marrow depression, bradycardia, chorea, decreased bone mineral density, DRESS syndrome, dyskinesia, dystonia, enlargement of facial features, granulocytopenia, hepatotoxicity, Hodgkin lymphoma, hyperglycemia, hypertrichosis, immunoglobulin abnormality, leukopenia, lymphadenopathy, malignant lymphoma, osteoporosis, pancytopenia, polyarteritis nodosa, Stevens-Johnson syndrome, systemic lupus erythematosus, thrombocytopenia, toxic epidermal necrolysis, tremor, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Blood dyscrasias: A spectrum of hematologic effects have been reported (eg, agranulocytosis, leukopenia, granulocytopenia, thrombocytopenia, and pancytopenia with or without bone marrow suppression) and may be fatal; patients with a previous history of adverse hematologic reaction to any drug may be at increased risk. Early detection of hematologic change is important; advise patients of early signs and symptoms including fever, sore throat, mouth ulcers, infections, easy bruising, petechial or purpuric hemorrhage.
- Bone effects: Chronic use of phenytoin has been associated with decreased bone mineral density (osteopenia, osteoporosis, and osteomalacia) and bone fractures. Chronic use may result in decreased vitamin D concentrations due to hepatic enzyme induction and may lead to vitamin D deficiency, hypocalcemia, and hypophosphatemia; monitor as appropriate and consider implementing vitamin D and calcium supplementation.
- Cardiovascular events: [US Boxed Warning]: Phenytoin must be administered slowly. Intravenous administration should not exceed 50 mg/minute in adult patients. In pediatric patients, intravenous administration rate should not exceed 1 to 3 mg/kg/minute or 50 mg/minute whichever is slower. Hypotension and severe cardiac arrhythmias (eg, heart block, ventricular tachycardia, ventricular fibrillation) may occur with rapid administration; adverse cardiac events have been reported at or below the recommended infusion rate. Cardiac monitoring is necessary during and after administration of intravenous phenytoin; reduction in rate of administration or discontinuation of infusion may be necessary. For nonemergency use, intravenous phenytoin should be administered more slowly; the use of oral phenytoin should be used whenever possible. Bradycardia and cardiac arrest have been reported with oral phenytoin administration, usually in patients with underlying cardiac disease, and have occurred at recommended doses and levels and associated with toxicity.
- Dermatologic reactions: Severe cutaneous adverse reactions (some fatal), including acute generalized exanthematous pustulosis (AGEP), toxic epidermal necrolysis (TEN), and Stevens-Johnson syndrome have been reported; the onset of symptoms is usually within 28 days of treatment but can occur later. Discontinue phenytoin if there are any signs of rash or other signs or symptoms indicative of a severe cutaneous reaction. Data suggests a genetic susceptibility for serious skin reactions in patients of Asian descent (see "Special populations" below).
- Extravasation: Vesicant (intravenous administration); ensure proper catheter or needle position prior to and during infusion. Avoid extravasation. IV formulation may cause soft tissue irritation and inflammation, and skin necrosis at IV site; avoid IV administration in small veins. The "purple glove syndrome" (ie, discoloration with edema and pain of distal limb) may occur following peripheral IV administration of phenytoin. This syndrome may or may not be associated with drug extravasation. Symptoms may resolve spontaneously; however, skin necrosis and limb ischemia may occur; interventions such as fasciotomies, skin grafts, and amputation (rare) may be required. To decrease the risk of this syndrome, inject phenytoin slowly and directly into a large vein through a large gauge needle or IV catheter; follow with NS flushes through the same needle or IV catheter.
- Hepatotoxicity: Cases of acute hepatotoxicity, including infrequent cases of acute hepatic failure, have been reported. Other manifestations include jaundice, hepatomegaly, elevated serum transaminase levels, leukocytosis, and eosinophilia. The clinical course of acute phenytoin hepatotoxicity ranges from prompt recovery to fatal outcomes. Immediately discontinue phenytoin in patients who develop acute hepatotoxicity and do not readminister.
- Hypersensitivity: Hypersensitivity, including angioedema, has been reported; discontinue immediately if hypersensitivity reaction occurs. Consider alternative therapy in patients who have experienced hypersensitivity to structurally similar drugs such as carboxamides (eg, carbamazepine), barbiturates, succinimides, and oxazolidinediones (eg, trimethadione).
- Lymphadenopathy: May occur (local or generalized), including benign lymph node hyperplasia, pseudolymphoma, lymphoma, and Hodgkin disease; cause and effect relationship has not been established.
- Multiorgan hypersensitivity reactions: Potentially serious, sometimes fatal multiorgan hypersensitivity reactions (also known as drug reaction with eosinophilia and systemic symptoms [DRESS]) have been reported with some antiepileptic drugs; including phenytoin; monitor for signs and symptoms of possible manifestations associated with lymphatic, hepatic, renal, and/or hematologic organ systems; gradual discontinuation and conversion to alternate therapy may be required.
- Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; notify healthcare provider immediately if symptoms occur.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with underlying cardiac disease; IV use is contraindicated in patients with sinus bradycardia, sinoatrial block, or second and third degree heart block.
- Diabetes: Use with caution in patients with diabetes mellitus; phenytoin may inhibit insulin release and increase serum glucose in patients with diabetes.
- Hepatic impairment: Use with caution in patients with hepatic impairment; use free (unbound) serum concentrations to monitor.
- Hypoalbuminemia: Use with caution in patients with any condition associated with low serum albumin levels, which will increase the free fraction of phenytoin in the serum and, therefore, the pharmacologic response. Use free (unbound) serum concentrations to monitor.
- Hypothyroidism: Use with caution in patients with hypothyroidism; phenytoin may alter thyroid hormone serum concentrations (with chronic administration).
- Porphyria: May cause exacerbation of porphyria; use with caution in patients with porphyria.
- Renal impairment: Use with caution in patients with renal impairment; use free (unbound) serum concentrations to monitor.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Asian ancestry: Asian patients with the variant HLA-B*1502 may be at an increased risk of developing Stevens-Johnson syndrome and/or TEN. Note: Carbamazepine, another antiepileptic with a chemical structure similar to phenytoin, includes in the manufacturer labeling a recommendation to screen patients of Asian descent for the HLA-B*1502 allele prior to initiating therapy; this is not a current recommendation in the phenytoin manufacturer labeling. Patients with a positive result should avoid phenytoin.
- Critically-ill patients: Use with caution in critically ill patients.
- Debilitated patients: Use with caution in patients who are debilitated.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer's labeling.
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures and respiratory depression; use caution (AAP 1997; Zar 2007).
Other warnings/precautions:
- Appropriate use: Not indicated for the treatment of absence seizures or seizures due to hypoglycemia or other metabolic causes.
- Sustained serum concentrations: Plasma concentrations of phenytoin sustained above the optimal range may produce confusional states referred to as delirium, psychosis, or encephalopathy, or rarely, irreversible cerebellar dysfunction and/or cerebellar atrophy. Measure plasma phenytoin concentrations at the first sign of acute toxicity; dosage reduction is indicated if phenytoin concentrations are excessive; if symptoms persist, discontinue administration.
- Withdrawal: Anticonvulsants should not be discontinued abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal.
Monitoring Parameters
CBC, liver function; vitamin D status (chronic use); suicidality (eg, suicidal thoughts, depression, behavioral changes); plasma phenytoin concentrations (if available, free phenytoin concentrations should be obtained in patients with renal impairment and/or hypoalbuminemia; if free phenytoin concentrations are unavailable, the adjusted total concentration may be determined based upon equations in adult patients). Trough concentrations are generally recommended for routine monitoring.
Additional monitoring with IV use: Continuous cardiac monitoring (rate, rhythm, blood pressure) and observation during administration recommended; blood pressure and pulse should be monitored every 15 minutes for 1 hour after administration (Meek, 1999); infusion site reactions
Consult individual institutional policies and procedures.
Pregnancy
Pregnancy Considerations
Phenytoin crosses the placenta (Harden 2009a). An increased risk of congenital malformations and adverse outcomes may occur following in utero phenytoin exposure. Reported malformations include orofacial clefts, cardiac defects, dysmorphic facial features, nail/digit hypoplasia, growth abnormalities including microcephaly, and mental deficiency. Isolated cases of malignancies (including neuroblastoma) and coagulation defects in the neonate (may be life threatening) following delivery have also been reported. Maternal use of phenytoin should be avoided when possible to decrease the risk of cleft palate and poor cognitive outcomes. Polytherapy may also increase the risk of congenital malformations; monotherapy is recommended (Harden 2009b). The maternal use of folic acid throughout pregnancy is recommended to reduce the risk of major congenital malformations (Harden 2009a). Potentially life-threatening bleeding disorders in the newborn may also occur due to decreased concentrations of vitamin K-dependent clotting factors following phenytoin exposure in utero; vitamin K administration to the mother prior to delivery and the newborn after birth is recommended.
Total plasma concentrations of phenytoin are decreased in the mother during pregnancy; unbound plasma (free) concentrations are also decreased and plasma clearance is increased. Due to pregnancy-induced physiologic changes, women who are pregnant may require dose adjustments of phenytoin in order to maintain clinical response; monitoring during pregnancy should be considered (Harden 2009a). For women with epilepsy who are planning a pregnancy in advance, baseline serum concentrations should be measured once or twice prior to pregnancy during a period when seizure control is optimal. Monitoring can then be continued once each trimester during pregnancy and postpartum; more frequent monitoring may be needed in some patients. Monitoring of unbound plasma concentrations is recommended (Patsalos 2008; Patsalos 2018). Effective contraception is recommended for females of reproductive potential who are not planning a pregnancy. Phenytoin may decrease the efficacy of hormonal contraceptives; consult drug interactions database for more detailed information.
Patients exposed to phenytoin during pregnancy are encouraged to enroll themselves in the North American Antiepileptic Drug Pregnancy Registry by calling 1-888-233-2334. Additional information is available at http://aedpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used to help control certain kinds of seizures.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Fatigue
- Headache
- Anxiety
- Trouble sleeping
- Constipation
- Vomiting
- Change in taste
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Depression like thoughts of suicide, anxiety, emotional instability, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Change in balance
- Abnormal gait
- Confusion
- Slurred speech
- Gingival pain or swelling
- Severe muscle pain
- Abnormal movements
- Twitching
- Trouble swallowing
- Trouble speaking
- Severe loss of strength and energy
- Seizures
- Burning or numbness feeling
- Bruising
- Bleeding
- Bone pain
- Involuntary eye movements
- Tremors
- Swollen glands
- Fever
- Rash
- Chest pain
- Unable to pass urine
- Change in amount of urine passed
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Fast heartbeat
- Slow heartbeat
- Abnormal heartbeat
- Severe dizziness
- Passing out
- Severe injection site redness, swelling, pain, or irritation
- Skin discoloration
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.