Boxed Warning
Congestive heart failure:
Thiazolidinediones, including pioglitazone, cause or exacerbate congestive heart failure (CHF) in some patients. After initiation of pioglitazone/glimepiride, observe patients carefully for signs and symptoms of heart failure (including excessive, rapid weight gain, dyspnea, and/or edema). If these signs and symptoms develop, manage the heart failure according to the current standards of care. Furthermore, consider discontinuation of pioglitazone/glimepiride.
Pioglitazone/glimepiride is not recommended in patients with symptomatic heart failure. Initiation of pioglitazone/glimepiride in patients with established New York Heart Association (NYHA) class III or IV heart failure is contraindicated.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
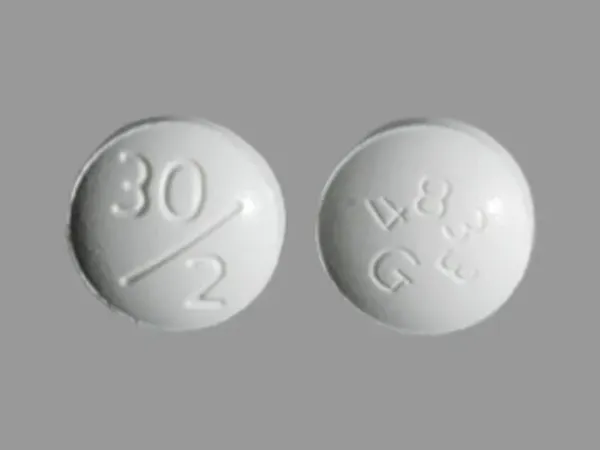
Tablet: 30/2: Pioglitazone 30 mg and glimepiride 2 mg; 30/4: Pioglitazone 30 mg and glimepiride 4 mg
Duetact:
30 mg/2 mg: Pioglitazone 30 mg and glimepiride 2 mg
30 mg/4 mg: Pioglitazone 30 mg and glimepiride 4 mg
Pharmacology
Mechanism of Action
Pioglitazone: A thiazolidinedione that lowers blood glucose by improving target cell response to insulin, without increasing pancreatic insulin secretion. It has a mechanism of action that is dependent on the presence of insulin for activity.
Glimepiride: A sulfonylurea that stimulates insulin release from the pancreatic beta cells; reduces glucose output from the liver; insulin sensitivity is increased at peripheral target sites.
Use: Labeled Indications
Diabetes mellitus, type 2: Management of type 2 diabetes mellitus (noninsulin dependent, NIDDM) as an adjunct to diet and exercise in adult patients already treated with a thiazolidinedione and a sulfonylurea or who have inadequate control on either agent alone
Contraindications
Hypersensitivity to glimepiride, pioglitazone, or any component of the formulation; history of allergic reaction to sulfonamide derivatives; NYHA Class III/IV heart failure (initiation of therapy).
Note: Although the FDA approved product labeling states this medication is contraindicated with other sulfonamide-containing drug classes, the scientific basis of this statement has been challenged. See “Warnings/Precautions” for more detail.
Documentation of allergenic cross-reactivity for thiazolidinediones is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Diabetes mellitus, type 2: Oral: Initial dose should be based on current dose of pioglitazone and/or sulfonylurea.
Patients inadequately controlled on glimepiride alone: Initial dose: Pioglitazone 30 mg/glimepiride 2 mg or pioglitazone 30 mg/glimepiride 4 mg once daily
Patients inadequately controlled on pioglitazone alone: Initial dose: Pioglitazone 30 mg/glimepiride 2 mg once daily
Patients currently on sulfonylurea monotherapy (other than glimepiride) or switching from combination therapy of pioglitazone plus a sulfonylurea (other than glimepiride): Initial: Pioglitazone 30 mg/glimepiride 2 mg once daily. When converting patients from other sulfonylureas with longer half-lives (eg, chlorpropamide) to glimepiride, observe patient carefully for 1 to 2 weeks due to overlapping hypoglycemic effects.
Patients with systolic dysfunction (eg, NYHA Class I and II): Initiate only after patient has been safely titrated to 30 mg of pioglitazone. Initial dose: Pioglitazone 30 mg/glimepiride 2 mg once daily.
Dosage adjustment: Dosage may be increased up to a maximum dose of pioglitazone 45 mg/glimepiride 8 mg once daily based on effectiveness and tolerability. Dosage adjustments in patients with systolic dysfunction should be done carefully and patient monitored for symptoms of worsening heart failure.
Dosage adjustment for hypoglycemia with combination therapy:
With an insulin secretagogue: Decrease the insulin secretagogue dose.
With insulin: Decrease insulin dose by 10% to 25%
Dosing: Geriatric
Initiate and adjust dose conservatively; observe carefully for hypoglycemia. Refer to adult dosing.
Administration
Oral: Administer once daily with the first main meal of the day. To avoid hypoglycemia, patients without oral intake may need to have the dose held.
Storage
Store at 15°C to 30°C (59°F to 86°F). Protect from moisture and humidity.
Pioglitazone and Glimepiride Images
Drug Interactions
Ajmaline: Sulfonamides may enhance the adverse/toxic effect of Ajmaline. Specifically, the risk for cholestasis may be increased. Monitor therapy
Alcohol (Ethyl): Sulfonylureas may enhance the adverse/toxic effect of Alcohol (Ethyl). A flushing reaction may occur. Monitor therapy
Alpelisib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Alpha-Lipoic Acid: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Androgens: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Exceptions: Danazol. Monitor therapy
Antidiabetic Agents: May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Beta-Blockers: May enhance the hypoglycemic effect of Sulfonylureas. Cardioselective beta-blockers (eg, acebutolol, atenolol, metoprolol, and penbutolol) may be safer than nonselective beta-blockers. All beta-blockers appear to mask tachycardia as an initial symptom of hypoglycemia. Ophthalmic beta-blockers are probably associated with lower risk than systemic agents. Exceptions: Levobunolol; Metipranolol. Monitor therapy
Carbocisteine: Sulfonylureas may enhance the adverse/toxic effect of Carbocisteine. Specifically, sulfonylureas may enhance adverse effects of alcohol that is present in liquid formulations of carbocisteine-containing products. Monitor therapy
Chloramphenicol (Systemic): May decrease the metabolism of Sulfonylureas. Monitor therapy
Cimetidine: May increase the serum concentration of Sulfonylureas. Monitor therapy
Colesevelam: May decrease the serum concentration of Glimepiride. Management: Administer glimepiride at least 4 hours prior to colesevelam. Consider therapy modification
Cyclic Antidepressants: May enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
CYP2C8 Inhibitors (Moderate): May increase the serum concentration of Pioglitazone. Monitor therapy
CYP2C8 Inhibitors (Strong): May increase the serum concentration of Pioglitazone. Management: Limit the pioglitazone dose to 15 mg daily and monitor for increased pioglitazone toxicities (eg, hypoglycemia) when used in combination with strong CYP2C8 inhibitors. Consider therapy modification
CYP2C9 Inhibitors (Moderate): May decrease the metabolism of CYP2C9 Substrates (High risk with Inhibitors). Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C9 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dexketoprofen: May enhance the adverse/toxic effect of Sulfonamides. Monitor therapy
Dipeptidyl Peptidase-IV Inhibitors: May enhance the hypoglycemic effect of Sulfonylureas. Management: Consider a decrease in sulfonylurea dose when initiating therapy with a dipeptidyl peptidase-IV inhibitor and monitor patients for hypoglycemia. Consider therapy modification
Direct Acting Antiviral Agents (HCV): May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Elexacaftor, Tezacaftor, and Ivacaftor: May increase the serum concentration of Glimepiride. Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP2C9 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP2C9 substrate should be performed with caution and close monitoring. Consider therapy modification
Fibric Acid Derivatives: May enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Fluconazole: May increase the serum concentration of Sulfonylureas. Management: Seek alternatives when possible. If used together, monitor closely for increased effects of sulfonylureas if fluconazole is initiated/dose increased, or decreased effects if fluconazole is discontinued/dose decreased. Consider therapy modification
Glucagon-Like Peptide-1 Agonists: May enhance the hypoglycemic effect of Sulfonylureas. Management: Consider sulfonylurea dose reductions when used in combination with glucagon-like peptide-1 agonists. Consider therapy modification
Guanethidine: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Herbs (Hypoglycemic Properties): May enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Hyperglycemia-Associated Agents: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Hypoglycemia-Associated Agents: May enhance the hypoglycemic effect of other Hypoglycemia-Associated Agents. Monitor therapy
Hypoglycemia-Associated Agents: Antidiabetic Agents may enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Insulins: Pioglitazone may enhance the adverse/toxic effect of Insulins. Specifically, the risk for hypoglycemia, fluid retention, and heart failure may be increased with this combination. Management: If insulin is combined with pioglitazone, dose reductions should be considered to reduce the risk of hypoglycemia. Monitor patients for fluid retention and signs/symptoms of heart failure. Consider therapy modification
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C8 Substrates (High Risk with Inhibitors or Inducers). Lumacaftor and Ivacaftor may increase the serum concentration of CYP2C8 Substrates (High Risk with Inhibitors or Inducers). Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Lumacaftor and Ivacaftor may increase the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Monitor therapy
Maitake: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Mecamylamine: Sulfonamides may enhance the adverse/toxic effect of Mecamylamine. Avoid combination
Metreleptin: May enhance the hypoglycemic effect of Sulfonylureas. Management: Sulfonylurea dosage adjustments (including potentially large decreases) may be required to minimize the risk for hypoglycemia with concurrent use of metreleptin. Monitor closely. Consider therapy modification
Miconazole (Oral): May enhance the hypoglycemic effect of Sulfonylureas. Miconazole (Oral) may increase the serum concentration of Sulfonylureas. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP2C9 Substrates (High risk with Inhibitors). Management: Use CYP2C9 substrates at the lowest recommended dose, and monitor closely for adverse effects, during and in the 2 weeks following mifepristone treatment. Consider therapy modification
Mitiglinide: May enhance the adverse/toxic effect of Sulfonylureas. Avoid combination
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Pegvisomant: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Pregabalin: May enhance the fluid-retaining effect of Thiazolidinediones. Monitor therapy
Probenecid: May decrease the protein binding of Sulfonylureas. Probenecid may increase the serum concentration of Sulfonylureas. Monitor therapy
Prothionamide: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Quinolones: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
RaNITIdine: May increase the serum concentration of Sulfonylureas. Monitor therapy
RifAMPin: May decrease the serum concentration of Sulfonylureas. Management: Seek alternatives to these combinations when possible. Monitor closely for diminished therapeutic effects of sulfonylureas if rifampin is initiated/dose increased, or enhanced effects if rifampin is discontinued/dose decreased. Consider therapy modification
Rifapentine: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Ritodrine: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Salicylates: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Sodium-Glucose Cotransporter 2 (SGLT2) Inhibitors: May enhance the hypoglycemic effect of Sulfonylureas. Management: Consider a decrease in sulfonylurea dose when initiating therapy with a sodium-glucose cotransporter 2 inhibitor and monitor patients for hypoglycemia. Consider therapy modification
Sulfonamide Antibiotics: May enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Sulfonylureas: Thiazolidinediones may enhance the hypoglycemic effect of Sulfonylureas. Management: Consider sulfonylurea dose adjustments in patients taking thiazolidinediones and monitor for hypoglycemia. Consider therapy modification
Tezacaftor and Ivacaftor: May increase the serum concentration of Glimepiride. Monitor therapy
Thiazide and Thiazide-Like Diuretics: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Thiazolidinediones: May enhance the hypoglycemic effect of Sulfonylureas. Management: Consider sulfonylurea dose adjustments in patients taking thiazolidinediones and monitor for hypoglycemia. Consider therapy modification
Topiramate: May decrease the serum concentration of Pioglitazone. Monitor therapy
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Sulfonylureas may enhance the anticoagulant effect of Vitamin K Antagonists. Vitamin K Antagonists may enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Voriconazole: May increase the serum concentration of Sulfonylureas. Monitor therapy
Adverse Reactions
Also see individual agents.
>10%:
Cardiovascular: Peripheral edema (6% to 12%)
Endocrine & metabolic: Hypoglycemia (13% to 16%), weight gain (9% to 13%)
Respiratory: Upper respiratory tract infection (12% to 15%)
1% to 10%:
Central nervous system: Headache (4% to 7%)
Gastrointestinal: Diarrhea (4% to 6%), nausea (4% to 5%)
Genitourinary: Urinary tract infection (6% to 7%)
Hematologic & oncologic: Anemia (≤2%)
Neuromuscular & skeletal: Limb pain (4% to 5%)
<1%, postmarketing, and/or case reports: Bladder carcinoma (FDA Safety Alert, Dec. 19, 2016)
Warnings/Precautions
Concerns related to adverse effects:
- Bladder cancer: Clinical trial data is inconsistent regarding the risk of bladder cancer in patients exposed to pioglitazone. Given the uncertainty of the findings, the manufacturer recommends to avoid use in patients with active bladder cancer and consider risks vs. benefits prior to initiating therapy in patients with a history of bladder cancer.
- Cardiovascular mortality: Product labeling states oral hypoglycemic drugs may be associated with an increased cardiovascular mortality as compared to treatment with diet alone or diet plus insulin. Data to support this association are limited, and several studies, including a large prospective trial (UKPDS), have not supported an association. In a prospective, active-controlled study comparing linagliptin to glimepiride in patients with high baseline cardiovascular risk, the rates of cardiovascular events were similar over ~6 years (Rosenstock 2019). In patients with established atherosclerotic cardiovascular disease, other agents (eg, with demonstrated cardiovascular risk reduction) are preferred (ADA 2019).
- Edema: Dose-related edema, including new-onset or exacerbation of existing edema, has been reported with pioglitazone; use with caution in patients with edema. Monitor for signs/symptoms of heart failure.
- Fractures: An increased incidence of bone fractures has been observed in females treated with pioglitazone; majority of fractures occurred in the lower limb and distal upper limb. Consider risk of fracture prior to initiation and during use.
- Heart failure/cardiac effects: [US Boxed Warning]: Thiazolidinediones, including pioglitazone, may cause or exacerbate heart failure; closely monitor for signs and symptoms of heart failure (eg, rapid weight gain, dyspnea, edema), particularly after initiation or dose increases; if heart failure develops, treat accordingly and consider dose reduction or discontinuation. Not recommended for use in any patient with symptomatic heart failure; initiation of therapy is contraindicated in patients with NYHA class III or IV heart failure. If used in patients with NYHA class I or II (systolic) heart failure, initiate at lowest dosage and monitor closely.
- Hematologic effects: Pioglitazone may decrease hemoglobin/hematocrit; effects may be related to increased plasma volume.
- Hepatic effects: Hepatic failure, including fatalities, has been reported with pioglitazone use. Monitor for signs/symptoms of liver injury closely during therapy; discontinuation of therapy may be necessary.
- Hypersensitivity reactions: Hypersensitivity reactions to glimepiride (eg, cutaneous eruptions, anaphylaxis, angioedema, Stevens-Johnson syndrome) have occurred. If hypersensitivity reactions occur, discontinue use immediately and institute alternative treatment.
- Hypoglycemia: All sulfonylurea drugs are capable of producing severe hypoglycemia. Hypoglycemia is more likely to occur when caloric intake is deficient, after severe or prolonged exercise, when ethanol is ingested, or when more than one glucose-lowering drug is used. It is also more likely in elderly patients, malnourished patients and in patients with impaired renal or hepatic function; use with caution.
- Macular edema: Has been reported with thiazolidinedione use, including pioglitazone; some patients with macular edema presented with blurred vision or decreased visual acuity, and most had peripheral edema at time of diagnosis. Patients should be seen by an ophthalmologist if any visual symptoms arise during therapy and all diabetic patients should have regular eye exams.
- Sulfonamide (“sulfa”) allergy: The FDA-approved product labeling for many medications containing a sulfonamide chemical group includes a broad contraindication in patients with a prior allergic reaction to sulfonamides. There is a potential for cross-reactivity between members of a specific class (eg, two antibiotic sulfonamides). However, concerns for cross-reactivity have previously extended to all compounds containing the sulfonamide structure (SO2NH2). An expanded understanding of allergic mechanisms indicates cross-reactivity between antibiotic sulfonamides and nonantibiotic sulfonamides may not occur or at the very least this potential is extremely low (Brackett 2004; Johnson 2005; Slatore 2004; Tornero 2004). In particular, mechanisms of cross-reaction due to antibody production (anaphylaxis) are unlikely to occur with nonantibiotic sulfonamides. T-cell-mediated (type IV) reactions (eg, maculopapular rash) are less well understood and it is not possible to completely exclude this potential based on current insights. In cases where prior reactions were severe (Stevens-Johnson syndrome/TEN), some clinicians choose to avoid exposure to these classes.
- Weight gain: Dose-related weight gain observed with pioglitazone use; mechanism unknown but likely associated with fluid retention and fat accumulation.
Disease-related concerns:
- Bariatric surgery:
– Altered absorption: Absorption may be altered given the anatomic and transit changes created by gastric bypass and sleeve gastrectomy surgery (Mechanick 2013; Melissas 2013). Use IR formulations after surgery to minimize the potential effects of bypassing stomach and proximal small bowel with gastric bypass or more rapid gastric emptying and proximal small bowel transit with sleeve gastrectomy (Apovian 2015). ER formulations may have altered release and absorption patterns after gastric bypass or sleeve gastrectomy (but not gastric band). Compared to control, Tmax in a gastric bypass cohort administered tolbutamide was significantly shorter (1.4 ± 1.8 vs 5.1 ± 1.7 hours; P < 0.001) while Cmax and AUC0-∞ were not altered (Tandra 2013).
– Hypoglycemia: Use an antidiabetic agent without the potential for hypoglycemia if possible; hypoglycemia may occur after gastric bypass, sleeve gastrectomy, and gastric band (Mechanick 2013). Insulin secretion and sensitivity may be partially or completely restored after these procedures (gastric bypass is most effective, followed by sleeve and finally band) (Korner 2009; Peterli 2012). First-phase insulin secretion and hepatic insulin sensitivity have been shown to be significantly improved in the immediate days after gastric bypass and sleeve gastrectomy. The restorative effects of these procedures on peripheral insulin sensitivity may occur later in the 3- to 12-month period postsurgery (Mingrone 2016).
– Weight gain: Evaluate risk vs benefit and consider alternative therapy after gastric bypass, sleeve gastrectomy, and gastric banding; weight gain may occur (Apovian 2015).
- Glucose-6-phosphate dehydrogenase (G6PD) deficiency: Patients with G6PD deficiency may be at an increased risk of sulfonylurea-induced hemolytic anemia; however, cases have also been described in patients without G6PD deficiency during postmarketing surveillance. Use with caution and consider a nonsulfonylurea alternative in patients with G6PD deficiency.
- Hepatic impairment: Due to the possible risk of drug-induced liver injury with pioglitazone, serum liver function tests (ALT, AST, alkaline phosphatase, and total bilirubin) should be obtained prior to initiation in all patients. In patients with abnormal hepatic tests, therapy should be initiated with caution. During therapy, if signs/symptoms of liver injury (eg, fatigue, anorexia, jaundice, dark urine, right upper abdominal discomfort) arise, interrupt pioglitazone therapy, obtain liver tests immediately and evaluate alternative etiologies. If an alternative etiology is not identified and serum ALT is >3 times ULN, do not resume therapy. Patients with serum ALT >3 times ULN and serum total bilirubin >2 times ULN are at risk for severe drug-induced liver injury. Risk of hypoglycemia may be increased in patients with hepatic impairment and receiving glimepiride.
- Renal function impairment: Use glimepiride with caution; patients with renal impairment are more likely to develop hypoglycemia.
- Stress-related states: It may be necessary to discontinue therapy and administer insulin if the patient is exposed to stress (fever, trauma, infection, surgery).
Special populations:
- CYP2C9 genotype: Systemic exposure of glimepiride is increased in patients with CYP2C9*3 allele (Niemi 2002).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use: Not for use in patients with diabetic ketoacidosis (DKA) or patients with type 1 diabetes mellitus (insulin-dependent, IDDM).
Monitoring Parameters
Hemoglobin A1c (at least twice yearly in patients who have stable glycemic control and are meeting treatment goals; quarterly in patients not meeting treatment goals or with therapy change [ADA 2019]), serum glucose.
Liver enzymes (ALT, AST, alkaline phosphatase, and total bilirubin) prior to initiation in all patients (with or without liver disease); continue routine periodic monitoring during treatment only in patients with liver disease or suspected liver disease.
Signs and symptoms of heart failure; weight gain; signs/symptoms of bladder cancer (dysuria, macroscopic hematuria, dysuria, urinary urgency); ophthalmic exams.
Pregnancy
Pregnancy Considerations
Refer to individual monographs.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience headache, diarrhea, nausea, muscle pain, common cold symptoms, sinusitis, sore throat, or weight gain. Have patient report immediately to prescriber signs of heart problems (cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out), signs of severe cerebrovascular disease (change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes), signs of liver problems (dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin), vision changes, painful urination, blood in the urine, passing a lot of urine, bone pain, severe loss of strength and energy, severe dizziness, passing out, chest pain, signs of low blood sugar (dizziness, headache, fatigue, feeling weak, shaking, fast heartbeat, confusion, increased hunger, or sweating), or signs of Stevens-Johnson syndrome/toxic epidermal necrolysis (red, swollen, blistered, or peeling skin [with or without fever]; red or irritated eyes; or sores in mouth, throat, nose, or eyes) (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for healthcare professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.