Boxed Warning
Congestive heart failure:
Thiazolidinediones, including pioglitazone, which is a component of pioglitazone/metformin, cause or exacerbate congestive heart failure (CHF) in some patients. After initiation of pioglitazone/metformin and after dose increases, monitor patients carefully for signs and symptoms of heart failure (eg, excessive, rapid weight gain, dyspnea, edema). If heart failure develops, manage the heart failure according to the current standards of care. Furthermore, consider discontinuation or dose reduction of pioglitazone/metformin.
Pioglitazone/metformin is not recommended in patients with symptomatic heart failure. Initiation of pioglitazone/metformin in patients with established New York Heart Association (NYHA) class III or IV heart failure is contraindicated.
Lactic acidosis:
Post-marketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. The onset of metformin-associated lactic acidosis is often subtle, accompanied only by nonspecific symptoms such as malaise, myalgias, respiratory distress, somnolence, and abdominal pain. Metformin-associated lactic acidosis was characterized by elevated blood lactate levels (greater than 5 mmol/L), anion gap acidosis (without evidence of ketonuria or ketonemia), an increased lactate:pyruvate ratio; and metformin plasma levels generally greater than 5 mcg/mL.
Risk factors for metformin-associated lactic acidosis include renal impairment, concomitant use of certain drugs (eg, carbonic anhydrase inhibitors such as topiramate), age 65 years or greater, having a radiological study with contrast, surgery and other procedures, hypoxic states (eg, acute heart failure), excessive alcohol intake, and hepatic impairment.
Steps to reduce the risk of and manage metformin-associated lactic acidosis in these high risk groups are provided in the full prescribing information.
If metformin-associated lactic acidosis is suspected, immediately discontinue pioglitazone/metformin and institute general supportive measures in a hospital setting. Prompt hemodialysis is recommended.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
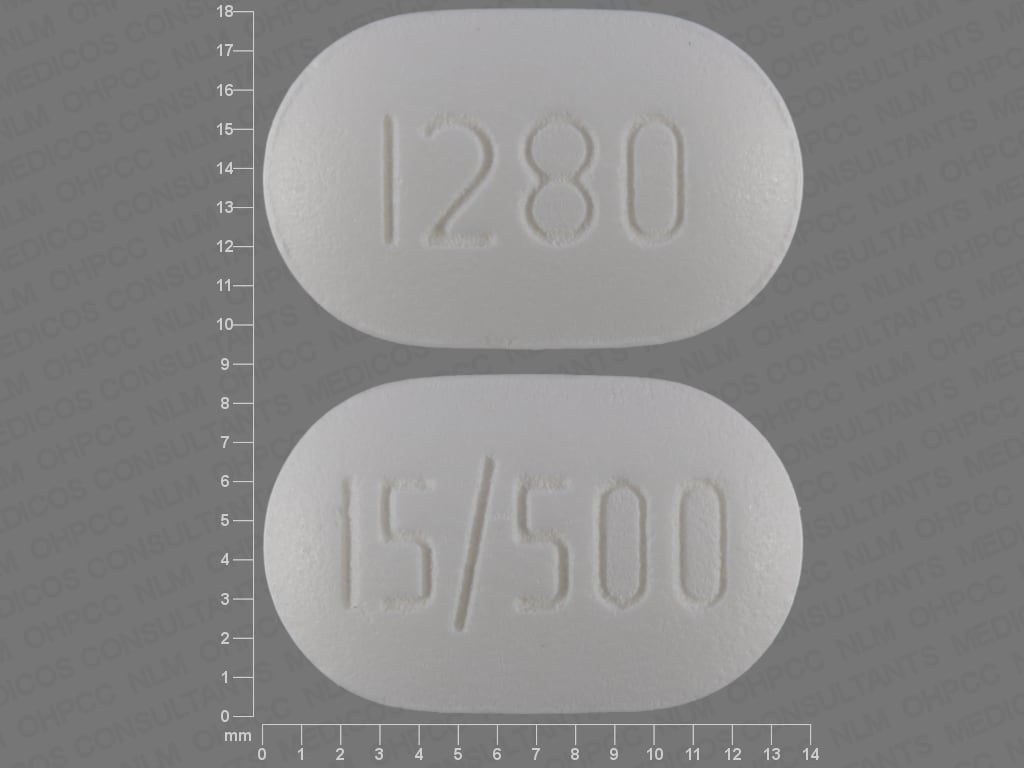
Tablet, oral: 15/500: Pioglitazone 15 mg and metformin hydrochloride 500 mg; 15/850: Pioglitazone 15 mg and metformin hydrochloride 850 mg
Actoplus Met:
15/500: Pioglitazone 15 mg and metformin hydrochloride 500 mg
15/850: Pioglitazone 15 mg and metformin hydrochloride 850 mg
Tablet, variable release, oral:
Actoplus Met XR:
15/1000: Pioglitazone 15 mg [immediate release] and metformin hydrochloride 1000 mg [extended release] [DSC]
30/1000: Pioglitazone 30 mg [immediate release] and metformin hydrochloride 1000 mg [extended release] [DSC]
Pharmacology
Mechanism of Action
Pioglitazone is a thiazolidinedione antidiabetic agent that lowers blood glucose by improving target cell response to insulin, without increasing pancreatic insulin secretion. It has a mechanism of action that is dependent on the presence of insulin for activity.
Metformin decreases hepatic glucose production, decreasing intestinal absorption of glucose, and improves insulin sensitivity (increases peripheral glucose uptake and utilization).
Use: Labeled Indications
Diabetes mellitus, type 2: As an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus when treatment with both pioglitazone and metformin is appropriate.
Contraindications
Hypersensitivity to pioglitazone, metformin, or any component of the formulation; established NYHA class III or IV heart failure, severe renal impairment (eg, eGFR <30 mL/minute/1.73 m2); metabolic acidosis, including diabetic ketoacidosis.
Dosage and Administration
Dosing: Adult
Diabetes mellitus, type 2: Oral:
Immediate-release tablet:
Initial: Pioglitazone 15 mg/metformin 500 mg twice daily or pioglitazone 15 mg/metformin 850 mg tablets once daily
Patients with asymptomatic NYHA class I or II heart failure (HF): Pioglitazone 15 mg/metformin 500 mg once daily or pioglitazone 15 mg/metformin 850 mg once daily. Note: Not recommended in patients with symptomatic HF and contraindicated with stage III or IV HF; the ADA generally recommends avoiding thiazolidinediones in the setting of HF (ADA 2019).
Inadequately controlled on metformin monotherapy: Pioglitazone 15 mg/metformin 500 mg twice daily or pioglitazone 15 mg/metformin 850 mg once or twice daily (depending on the dose of metformin already being taken).
Inadequately controlled on pioglitazone monotherapy: Pioglitazone 15 mg/metformin 500 twice daily or pioglitazone 15 mg/metformin 850 mg once daily.
Dose titration: If necessary, may titrate gradually with careful monitoring of adverse effects (eg, weight gain, edema, signs/symptoms of HF). Maximum daily dose: Pioglitazone 45 mg/metformin 2.55 g; consider limiting pioglitazone dose to ≤30 mg/day if worsening HF is a concern (AACE/ACE [Garber 2019]). Note: Metformin daily doses >2 g may be better tolerated if given 3 times daily.
Extended-release tablet:
Initial (includes patients with asymptomatic NYHA class I or II HF): Pioglitazone 15 to 30 mg/metformin 1 g once daily. Note: Not recommended in patients with symptomatic HF and contraindicated with stage III or IV HF; the ADA generally recommends avoiding thiazolidinediones in the setting of HF (ADA 2019).
Inadequately controlled on metformin or pioglitazone monotherapy: Pioglitazone 15 mg/metformin 1 g twice daily or pioglitazone 30 mg/metformin 1 g once daily.
Dose titration: If necessary, titrate gradually with careful monitoring of adverse effects (eg, weight gain, edema, signs/symptoms of HF). Maximum daily dose: Pioglitazone 45 mg/metformin 2 g; consider limiting pioglitazone dose to ≤30 mg/day if worsening HF is a concern (AACE/ACE [Garber 2019]).
Dosage adjustment for hypoglycemia with combination therapy:
With an insulin secretagogue (eg, sulfonylurea): Decrease the insulin secretagogue dose.
With insulin: Decrease insulin dose by 10% to 25%.
Dosage adjustment with strong CYP2C8 inhibitors (eg, gemfibrozil): Maximum recommended dose: Pioglitazone 15 mg and metformin 850 mg daily (immediate release) or pioglitazone 15 mg/metformin 1 g daily (extended release).
Dosing: Geriatric
Immediate-release or extended-release tablet: Refer to adult dosing. The initial and maintenance dosing of metformin should be conservative, due to the potential for decreased renal function (monitor).
Administration
Oral: Administer with meals. Extended release tablets should be swallowed whole; do not crush, split, or chew.
Dietary Considerations
Avoid ethanol. Individualized medical nutrition therapy is an integral part of therapy. Monitor for signs and symptoms of vitamin B12 and/or folic acid deficiency; supplementation may be required.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from moisture and humidity
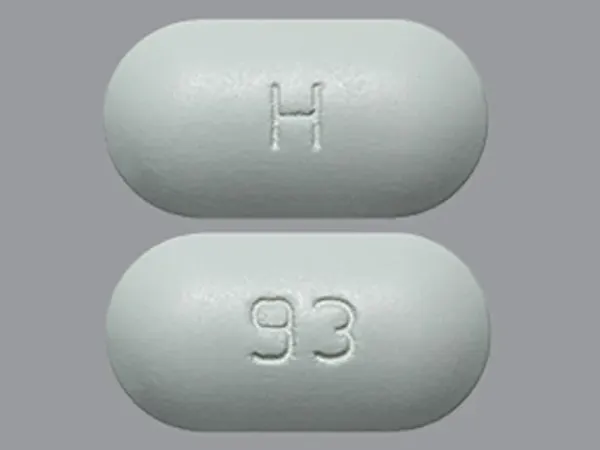
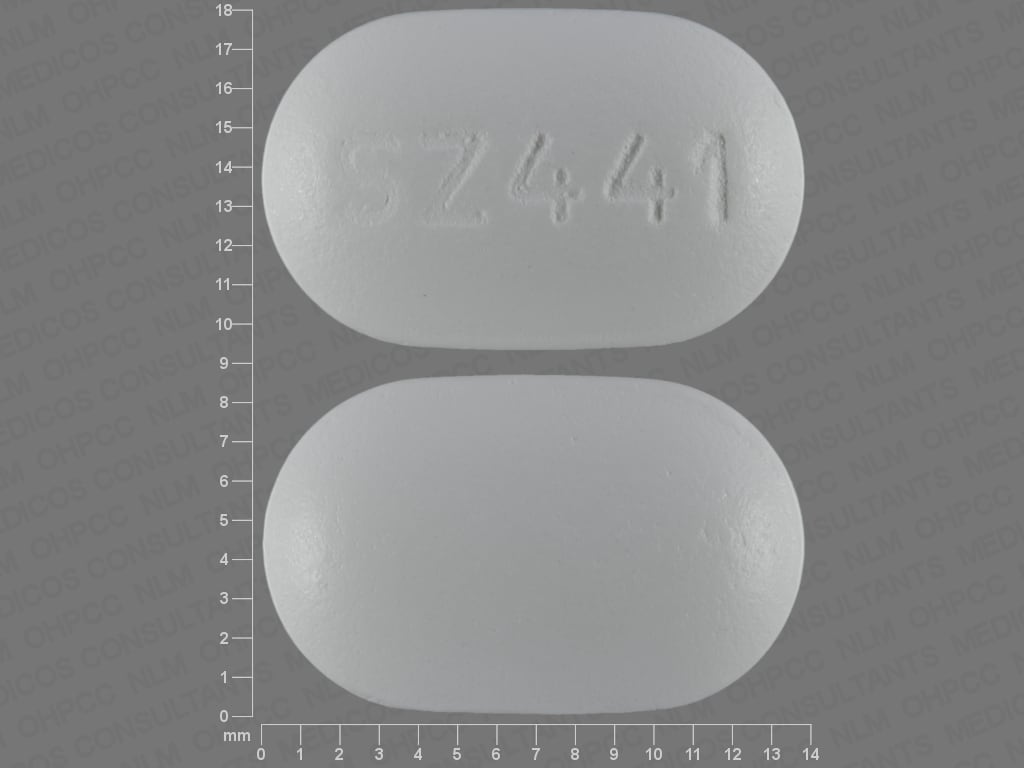
Pioglitazone and Metformin Images
Drug Interactions
Abemaciclib: May increase the serum concentration of MetFORMIN. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of MetFORMIN. Specifically, alcohol may potentiate the risk of lactic acidosis Avoid combination
Alpha-Lipoic Acid: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Androgens: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Exceptions: Danazol. Monitor therapy
Bictegravir: May increase the serum concentration of MetFORMIN. Monitor therapy
Carbonic Anhydrase Inhibitors: May enhance the adverse/toxic effect of MetFORMIN. Specifically, the risk of developing lactic acidosis may be increased. Exceptions: Brinzolamide; Dorzolamide. Monitor therapy
Cephalexin: May increase the serum concentration of MetFORMIN. Monitor therapy
Cimetidine: May increase the serum concentration of MetFORMIN. Management: Consider alternatives to cimetidine in patients receiving metformin due to a potential for increased metformin concentrations and toxicity (including lactic acidosis). Consider therapy modification
CYP2C8 Inducers (Moderate): May decrease the serum concentration of Pioglitazone. Monitor therapy
CYP2C8 Inhibitors (Moderate): May increase the serum concentration of Pioglitazone. Monitor therapy
CYP2C8 Inhibitors (Strong): May increase the serum concentration of Pioglitazone. Management: Limit the pioglitazone dose to 15 mg daily and monitor for increased pioglitazone toxicities (eg, hypoglycemia) when used in combination with strong CYP2C8 inhibitors. Consider therapy modification
Dalfampridine: MetFORMIN may increase the serum concentration of Dalfampridine. Dalfampridine may increase the serum concentration of MetFORMIN. Monitor therapy
Direct Acting Antiviral Agents (HCV): May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Dofetilide: MetFORMIN may increase the serum concentration of Dofetilide. Monitor therapy
Dolutegravir: May increase the serum concentration of MetFORMIN. Management: Consider the risks and benefits of this combination. If combined, limit the daily metformin dose to 1,000 mg when used with dolutegravir. Monitor for increased metformin effects/toxicities (including lactic acidosis) during concomitant use. Consider therapy modification
Erdafitinib: May increase the serum concentration of OCT2 Substrates. Monitor therapy
Glycopyrrolate (Systemic): May increase the serum concentration of MetFORMIN. Monitor therapy
Guanethidine: May enhance the hypoglycemic effect of Antidiabetic Agents. Monitor therapy
Hyperglycemia-Associated Agents: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Hypoglycemia-Associated Agents: Antidiabetic Agents may enhance the hypoglycemic effect of Hypoglycemia-Associated Agents. Monitor therapy
Insulins: Pioglitazone may enhance the adverse/toxic effect of Insulins. Specifically, the risk for hypoglycemia, fluid retention, and heart failure may be increased with this combination. Management: If insulin is combined with pioglitazone, dose reductions should be considered to reduce the risk of hypoglycemia. Monitor patients for fluid retention and signs/symptoms of heart failure. Consider therapy modification
Iodinated Contrast Agents: May enhance the adverse/toxic effect of MetFORMIN. Renal dysfunction that may be caused by iodinated contrast agents may lead to metformin-associated lactic acidosis. Management: Management advice varies. Refer to the full drug interaction monograph content for details. Exceptions: Diatrizoate Meglumine; Diatrizoate Sodium; Ethiodized Oil. Consider therapy modification
Isavuconazonium Sulfate: May increase the serum concentration of MetFORMIN. Monitor therapy
LamoTRIgine: May increase the serum concentration of MetFORMIN. Management: The lamotrigine Canadian product monograph states that coadministration of these drugs is not recommended. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C8 Substrates (High Risk with Inhibitors or Inducers). Lumacaftor and Ivacaftor may increase the serum concentration of CYP2C8 Substrates (High Risk with Inhibitors or Inducers). Monitor therapy
Maitake: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Monoamine Oxidase Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May enhance the adverse/toxic effect of MetFORMIN. Monitor therapy
Ombitasvir, Paritaprevir, and Ritonavir: May enhance the adverse/toxic effect of MetFORMIN. Specifically, the risk for lactic acidosis may be increased. Monitor therapy
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: May enhance the adverse/toxic effect of MetFORMIN. Specifically, the risk for lactic acidosis may be increased. Monitor therapy
Ondansetron: May increase the serum concentration of MetFORMIN. Monitor therapy
Patiromer: May decrease the serum concentration of MetFORMIN. Management: Administer metformin at least 3 hours before or 3 hours after patiromer. Consider therapy modification
Pegvisomant: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Pregabalin: May enhance the fluid-retaining effect of Thiazolidinediones. Monitor therapy
Prothionamide: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Quinolones: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Quinolones may diminish the therapeutic effect of Blood Glucose Lowering Agents. Specifically, if an agent is being used to treat diabetes, loss of blood sugar control may occur with quinolone use. Monitor therapy
Ranolazine: May increase the serum concentration of MetFORMIN. Management: Limit the metformin dose to a maximum of 1,700 mg per day when used together with ranolazine 1,000 mg twice daily. Monitor patients for metformin toxicities, including lactic acidosis and carefully weigh the risks and benefits of this combination. Consider therapy modification
Ritodrine: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Salicylates: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the hypoglycemic effect of Blood Glucose Lowering Agents. Monitor therapy
Sulfonylureas: Thiazolidinediones may enhance the hypoglycemic effect of Sulfonylureas. Management: Consider sulfonylurea dose adjustments in patients taking thiazolidinediones and monitor for hypoglycemia. Consider therapy modification
Tafenoquine: May increase the serum concentration of MATE1 Substrates. Management: Avoid use of MATE substrates with tafenoquine, and if the combination cannot be avoided, monitor closely for evidence of toxicity of the MATE substrate and consider a reduced dose of the MATE substrate according to that substrate's labeling. Consider therapy modification
Tafenoquine: May increase the serum concentration of OCT2 Substrates. Management: Avoid use of OCT2 substrates with tafenoquine, and if the combination cannot be avoided, monitor closely for evidence of toxicity of the OCT2 substrate and consider a reduced dose of the OCT2 substrate according to that substrate's labeling. Consider therapy modification
Thiazide and Thiazide-Like Diuretics: May diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Topiramate: May enhance the adverse/toxic effect of MetFORMIN. Monitor therapy
Topiramate: May decrease the serum concentration of Pioglitazone. Monitor therapy
Trimethoprim: May increase the serum concentration of MetFORMIN. Monitor therapy
Trospium: MetFORMIN may decrease the serum concentration of Trospium. Monitor therapy
Vandetanib: May increase the serum concentration of MetFORMIN. Monitor therapy
Verapamil: May diminish the therapeutic effect of MetFORMIN. Monitor therapy
Adverse Reactions
Percentages of adverse effects as reported with the combination product. Also see individual agents.
>10%:
Cardiovascular: Lower extremity edema (3% to 11%)
Respiratory: Upper respiratory tract infection (12% to 16%)
1% to 10%:
Central nervous system: Headache (2% to 6%), dizziness (5%)
Endocrine & metabolic: Weight gain (3% to 7%)
Gastrointestinal: Diarrhea (5% to 6%), nausea (4% to 6%)
Genitourinary: Urinary tract infection (5% to 6%)
Hematologic & oncologic: Anemia (≤2%)
Respiratory: Sinusitis (4% to 5%)
<1%, postmarketing, and/or case reports: Bladder carcinoma (FDA Safety Alert, Dec. 19, 2016)
Warnings/Precautions
Concerns related to adverse effects:
- Bladder cancer: Clinical trial data is inconsistent regarding the risk of bladder cancer in patients exposed to pioglitazone. Given the uncertainty of the findings, the manufacturer recommends to avoid use in patients with active bladder cancer and consider risks vs. benefits prior to initiating therapy in patients with a history of bladder cancer.
- Edema: Dose-related edema, including new-onset or exacerbation of existing edema, has been reported with pioglitazone; use with caution in patients with edema. Monitor for signs/symptoms of heart failure.
- Fractures: An increased incidence of bone fractures in females treated with pioglitazone has been observed; majority of fractures occurred in the lower limb and distal upper limb. Consider risk of fracture prior to initiation and during use.
- Heart failure/cardiac effects: [US Boxed Warning]: Thiazolidinediones, including pioglitazone, may cause or exacerbate heart failure; closely monitor for signs and symptoms of heart failure (eg, rapid weight gain, dyspnea, edema), particularly after initiation or dose increases; if HF develops, treat accordingly and consider dose reduction or discontinuation. Not recommended for use in any patient with symptomatic heart failure; initiation of therapy is contraindicated in patients with NYHA class III or IV heart failure. If used in patients with NYHA class I or II (systolic) HF, initiate at lowest dosage and monitor closely. Metformin may be used in patients with stable heart failure; avoid use in unstable or hospitalized patients with heart failure (ADA 2019). Risk of lactic acidosis may be increased secondary to hypoperfusion. In a scientific statement from the American Heart Association, metformin has been determined to be an agent that may exacerbate underlying myocardial dysfunction (magnitude: major) (AHA [Page 2016]). Use of metformin in patients with HF may be associated with reduced mortality and reduction in hospital readmission for heart failure (Crowley 2017; Eurich 2013).
- Hematologic effects: Pioglitazone may decrease hemoglobin/hematocrit; effects may be related to increased plasma volume.
- Hepatic effects: Hepatic failure, including fatalities, has been reported with pioglitazone. Monitor for signs/symptoms of liver injury closely during therapy; discontinuation of therapy may be necessary.
- Hypoglycemia: The risk of hypoglycemia is increased when pioglitazone is combined with insulin or other diabetic medications; dosage adjustment of concomitant hypoglycemic agents may be necessary.
- Lactic acidosis: [US Boxed Warning]: Postmarketing cases of metformin-associated lactic acidosis have resulted in death, hypothermia, hypotension, and resistant bradyarrhythmias. The onset is often subtle, accompanied by nonspecific symptoms (eg, malaise, myalgias, respiratory distress, somnolence, abdominal pain); elevated blood lactate levels (>5 mmol/L); anion gap acidosis (without evidence of ketonuria or ketonemia); increased lactate:pyruvate ratio; metformin plasma levels generally >5 mcg/mL. Risk factors for lactic acidosis include patients with renal impairment, concomitant use of certain drugs (eg, carbonic anhydrase inhibitors such as topiramate), ≥65 years of age, having a radiologic study with contrast, surgery and other procedures, hypoxic states (eg, acute heart failure), excessive alcohol intake, and hepatic impairment. Discontinue immediately if lactic acidosis is suspected; prompt hemodialysis is recommended. Lactic acidosis should be suspected in any patient with diabetes receiving metformin with evidence of acidosis but without evidence of ketoacidosis. Discontinue use in patients with conditions associated with dehydration, hypoperfusion, sepsis, or hypoxemia. Temporarily discontinue therapy in patients with restricted food and fluid intake. The risk of accumulation and lactic acidosis increases with the degree of impairment of renal function.
- Macular edema: Has been reported with thiazolidinedione use, including pioglitazone; some patients with macular edema presented with blurred vision or decreased visual acuity, and most had peripheral edema at time of diagnosis. Patients should be seen by an ophthalmologist if any visual symptoms arise during therapy and all diabetic patients should have regular eye exams.
- Vitamin B12 concentrations: Long-term metformin use is associated with vitamin B12 deficiency; monitor vitamin B12 serum concentrations periodically with long-term therapy. Monitoring of B12 serum concentrations should be considered in all patients receiving metformin and in particular those with peripheral neuropathy or anemia (ADA 2019).
- Weight gain: Dose-related weight gain observed with pioglitazone use; mechanism unknown but likely associated with fluid retention and fat accumulation.
Disease-related concerns:
- Bariatric surgery:
– Altered absorption: Use IR tablets after surgery. Absorption may be altered given the anatomic and transit changes created by gastric bypass and sleeve gastrectomy surgery. ER tablets may have a reduced effect after gastric bypass or sleeve gastrectomy due to the direct bypass of the stomach and proximal small bowel with gastric bypass or a more rapid gastric emptying and proximal small bowel transit with sleeve gastrectomy (Mechanick 2013; Melissas 2013). After gastric bypass (Roux-en-Y gastric bypass [RYGB]), administration of IR tablets led to increased absorption (AUC0-∞ increased by 21%) and bioavailability (increased by 50%) (Padwal 2011). Lactate levels decrease after gastric bypass (RYGB)-induced weight loss irrespective of the use of metformin. Routinely lowering metformin dose after gastric bypass is not necessary as long as normal renal function is preserved (Deden 2018).
– Weight gain: Evaluate risk vs benefit and consider alternative therapy after gastric bypass, sleeve gastrectomy, and gastric banding; weight gain may occur (Apovian 2015).
- Hepatic impairment: The manufacturer recommends to generally avoid use of metformin in patients with hepatic impairment or with clinical or laboratory evidence of hepatic disease due to potential for lactic acidosis. However, continued use of metformin in patients with diabetes with liver dysfunction, including cirrhosis, may be associated with a survival benefit in carefully selected patients (Brackett 2010; Crowley 2017; Zhang 2014). Due to the possible risk of drug-induced liver injury with pioglitazone, serum liver function tests (ALT, AST, alkaline phosphatase, and total bilirubin) should be obtained prior to initiation in all patients. In patients with abnormal hepatic tests, therapy should be initiated with caution. During therapy, if signs/symptoms of liver injury (eg, fatigue, anorexia, jaundice, dark urine, right upper abdominal discomfort) arise, interrupt pioglitazone therapy, obtain liver tests immediately and evaluate alternative etiologies. If an alternative etiology is not identified and serum ALT is >3 times ULN, do not resume therapy. Patients with serum ALT >3 times ULN and serum total bilirubin >2 times ULN are at risk for severe drug-induced liver injury.
- Renal impairment: Metformin is substantially excreted by the kidney; assess renal function prior to initiation of therapy and periodically thereafter using eGFR; the risk of metformin accumulation and lactic acidosis increases with degree of renal impairment. Use is contraindicated in patients with eGFR <30 mL/minute/1.73 m2. Assess benefits/risks of metformin use in patients with eGFR 30 to 45 mL/minute/1.73 m2; if used, dosage reduction is recommended (ADA [Lipska 2011]; Inzucchi 2014). Use of concomitant medications that may affect renal function (ie, affect tubular secretion) may also affect metformin disposition. Metformin should be withheld in patients with dehydration and/or prerenal azotemia.
- Stress-related states: It may be necessary to discontinue metformin and administer insulin if the patient is exposed to stress (fever, trauma, infection, surgery).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution; risk of metformin associated lactic acidosis increases with age.
Dosage form specific issues:
- Extended-release tablet: Insoluble tablet shell may remain intact and be visible in the stool.
Other warnings/precautions:
- Appropriate use: Not for use in patients with diabetic ketoacidosis (DKA) or patients with type 1 diabetes mellitus.
- Ethanol use: Instruct patients to avoid excessive acute or chronic ethanol use; ethanol may potentiate metformin's effect on lactate metabolism and increase risk of lactic acidosis.
- Iodinated contrast: According to the manufacturer, it is recommended to temporarily discontinue metformin at the time of or before iodinated contrast imaging procedures in patients with an eGFR 30 to 60 mL/minute/1.73 m2; or with a history of hepatic disease, alcoholism, or heart failure; or in patients who will receive intra-arterial iodinated contrast. Reevaluate eGFR 48 hours after imaging procedure; restart if renal function is stable. Alternatively, the American College of Radiology (ACR) guidelines recommend that metformin may be used prior to or following administration of iodinated contrast media in patients with no evidence of acute kidney injury (AKI) and with an eGFR ≥30 mL/minute/1.73 m2; ACR guidelines recommend temporary discontinuation of metformin in patients with known AKI or severe chronic kidney disease ([stage IV or V [ie, eGFR <30 mL/minute/1.73 m2]) or who are undergoing arterial catheter studies (ACR 2017).
- Patient education: Diabetes self-management education is essential to maximize the effectiveness of therapy.
- Surgical procedures: Metformin should be withheld the day of surgery (all other oral hypoglycemic agents should be withheld the morning of surgery or procedure) (ADA 2019). Restart only after normal oral intake resumed and normal renal function is verified.
Monitoring Parameters
Hemoglobin A1c (at least twice yearly in patients who have stable glycemic control and are meeting treatment goals; quarterly in patients not meeting treatment goals or with therapy change [ADA 2019]), plasma glucose; initial and periodic monitoring of hematologic parameters (eg, hemoglobin/hematocrit and red blood cell indices); vitamin B12 serum concentrations periodically with long-term therapy and folate if anemia is present
Liver enzymes (ALT, AST, alkaline phosphatase, and total bilirubin) prior to initiation in all patients and during treatment if signs/symptoms of liver dysfunction arise. Initial and periodic monitoring of hematologic parameters (eg, hemoglobin/hematocrit and red blood cell indices); renal function (eGFR) should be performed prior to initiation of therapy and at least annually (more often in patients at risk of developing renal impairment; every 3 to 6 months if eGFR 45 to <60 mL/minute/1.73 m2; every 3 months if eGFR 30 to <45 mL/minute/1.73 m2 [Lipska 2011]).
Signs and symptoms of edema or heart failure; weight gain; signs/symptoms of bladder cancer (dysuria, macroscopic hematuria, dysuria, urinary urgency); ophthalmic exams.
Pregnancy
Pregnancy Considerations
Metformin crosses the placenta (ADA 2020). Refer to individual monographs for additional information.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience nausea, vomiting, diarrhea, passing gas, or headache. Have patient report immediately to prescriber signs of heart problems (cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out), signs of too much lactic acid in the blood (lactic acidosis; fast breathing, fast heartbeat, abnormal heartbeat, vomiting, drowsiness, shortness of breath, feeling very tired or weak, severe dizziness, feeling cold, or muscle pain or cramps), signs of liver problems (dark urine, feeling tired, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes), bone pain, loss of strength and energy, vision changes, pain with urination, blood in urine, passing a lot of urine, or signs of low blood sugar (dizziness, headache, fatigue, feeling weak, shaking, a fast heartbeat, confusion, hunger, or sweating) (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for healthcare professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience and judgment in diagnosing, treating and advising patients.