Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral, as hydrochloride:
Neuro-K-250 T.D.: 250 mg [corn free, rye free, starch free, sugar free, wheat free]
Solution, Injection, as hydrochloride:
Generic: 100 mg/mL (1 mL)
Tablet, Oral, as hydrochloride:
Neuro-K-50: 50 mg
Neuro-K-500: 500 mg
Neuro-K-250 Vitamin B6: 250 mg
Pyri 500: 500 mg
Generic: 25 mg, 50 mg, 100 mg, 250 mg
Tablet, Oral, as hydrochloride [preservative free]:
Generic: 25 mg, 50 mg, 100 mg [DSC]
Tablet Extended Release, Oral, as hydrochloride:
Generic: 200 mg
Pharmacology
Mechanism of Action
Precursor to pyridoxal, which functions in the metabolism of proteins, carbohydrates, and fats; pyridoxal also aids in the release of liver and muscle-stored glycogen and in the synthesis of GABA (within the central nervous system) and heme
When used for the treatment of ethylene glycol poisoning, pyridoxine is theorized to increase the formation of glycine, a nontoxic metabolite (Barceloux 1999).
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed (IOM 1998)
Metabolism
Hepatic to pyridoxal phosphate and pyridoxamine phosphate (active forms)
Excretion
Urine (as metabolites)
Half-Life Elimination
Biologic: 15 to 20 days
Use: Labeled Indications
Pyridoxine deficiency: Treatment and prevention of pyridoxine (vitamin B6) deficiency.
Use: Off Label
Ethylene glycol poisoningc
The American Academy of Clinical Toxicology guidelines recognize the lack of human clinical data for this use and consider pyridoxine as an adjunctive cofactor therapy in ethylene glycol poisoning without a formal or evidence-based recommendation, especially in patients who may have vitamin deficiencies (eg, patients with alcoholism) Barceloux 1999.
Gyromitrin-containing mushroom (false morel) overdose/toxicity (treatment/prophylaxis)c
Clinical experience suggests the utility of pyridoxine in the treatment of seizures from acute gyromitrin-containing mushroom toxicity Diaz 2005. Additional data may be necessary to further define the role of pyridoxine in this condition.
Nausea and vomiting of pregnancycyes
Clinical experience suggests the utility of pyridoxine in the treatment of nausea and vomiting of pregnancy Neibyl 2010.
Based on the American Society of Obstetricians and Gynecologists and the Society of Obstetricians and Gynaecologists of Canada practice guidelines, pyridoxine alone or in combination with doxylamine is a safe and effective treatment for nausea and vomiting of pregnancy and should be considered a first-line pharmacologic therapy ACOG 189 2018, Campbell [SOGC] 2016.
Neurological toxicities (ie, seizures, coma) associated with isoniazid overdose (prevention)c
Clinical experience suggests the utility of pyridoxine in the prevention of isoniazid-induced neurologic toxicities Hernon 2011. Additional data may be necessary to further define the role of pyridoxine in this condition.
Neurological toxicities (ie, seizures, coma) associated with isoniazid overdose (treatment)c
Data from a single case report suggests that pyridoxine may be beneficial for the treatment of isoniazid-induced seizures and/or coma Morrow 2006. Clinical experience also suggests the utility of pyridoxine in the treatment of isoniazid-induced seizures and/or coma Howland 2011. Additional data may be necessary to further define the role of pyridoxine in this condition.
Peripheral neuropathy associated with isoniazid therapy for Mycobacterium tuberculosis (prevention)yes
Based on the Department of Health and Human Services (DHHS) Guidelines for the Prevention and Treatment of Opportunistic Infections in HIV-Infected Adults and Adolescents, pyridoxine is effective and recommended in the prevention of peripheral neuropathy associated with isoniazid therapy for Mycobacterium tuberculosis.
Contraindications
Hypersensitivity to pyridoxine or any component of the formulation
Dosage and Administration
Dosing: Adult
Pyridoxine deficiency: IM, IV: 10 to 20 mg/day for 3 weeks, followed by daily oral therapy for several weeks. Doses up to 600 mg/day may be needed with pyridoxine dependency syndrome.
Ethylene glycol poisoning (off-label use): Note: Cofactors are adjunctive to antidotal therapy and should never be used alone.
IV: 100 mg per day until the intoxication has resolved (Howland 2015)
Gyromitrin-containing mushroom (false morel) overdose/toxicity (treatment/prophylaxis) (off-label use): IV: 25 mg/kg over 15 to 30 minutes; repeat dose as needed to control seizures (Diaz 2005; Lheureux 2005)
Nausea and vomiting of pregnancy (off-label use): Oral: 10 to 25 mg 3 to 4 times a day. May be given alone or in combination with doxylamine. Adjust dose based on severity of symptoms (ACOG 189 2018).
Neurological toxicities (ie, seizures, coma) associated with isoniazid overdose (prevention) (off-label use): IV: Asymptomatic patients who present within 2 hours of ingesting a potentially toxic amount of isoniazid should receive a prophylactic dose of pyridoxine (Hernon 2015). Dosing recommendations are the same as for the treatment of symptomatic patients.
Neurological toxicities (ie, seizures, coma) associated with isoniazid overdose (treatment) (off-label use): IV:
Acute ingestion of known amount: Initial: A total dose of pyridoxine equal to the amount of isoniazid ingested (maximum dose: 5 g); administer at a rate of 0.5 to 1 g/minute until seizures stop or the maximum initial dose has been administered; may repeat every 5 to 10 minutes as needed to control persistent seizure activity and/or CNS toxicity. If seizures stop prior to the administration of the calculated initial dose, infuse the remaining pyridoxine over 4 to 6 hours (Howland 2015; Morrow 2006).
Acute ingestion of unknown amount: Initial: 5 g; administer at a rate of 0.5 to 1 g/minute; may repeat every 5 to 10 minutes as needed to control persistent seizure activity and/or CNS toxicity (Howland 2015; Morrow 2006).
Peripheral neuropathy associated with isoniazid therapy for Mycobacterium tuberculosis (prevention): Oral: 25 to 50 mg/day (CDC [Kaplan 2009]).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Pyridoxine deficiency; treatment: Oral, IM, IV:
Children: 5 to 25 mg/day for 3 weeks, then 2.5 to 5 mg/day in multivitamin product
Adolescents: 10 to 20 mg/day for 3 weeks, then 2 to 5 mg/day (usual dosage found in multivitamin products)
Pyridoxine-dependent seizures, treatment: Oral, IM, IV: Infants and Children:
Initial: IV preferred: 50 to 100 mg (Rajesh 2003)
Maintenance: Oral preferred: Usual: 50 to 100 mg/day; range: 10 to 200 mg (Rajesh 2003); an observational study in UK described a usual dose of 30 mg/kg/day (Baxter 1999)
Drug-induced deficiency/toxicity (cycloserine, isoniazid, penicillamine); chronic use: Oral, IM, IV:
Isoniazid/Cycloserine:
Prevention: Note: Recommended for patients at risk: Exclusively breast-fed infants, meat- and milk-deficient diet, nutritional deficiency, pregnant adolescents (Red Book [AAP] 2012).
Non-HIV-exposed/-positive:
Infants and Children: 1 mg/kg/day; usual range: 10 to 50 mg/day (Red Book [AAP] 2012)
Adolescents: 30 mg/day
HIV-exposed/-positive:
Infants and Children: 1 to 2 mg/kg once daily; maximum daily dose: 50 mg/day (DHHS [pediatric] 2013)
Adolescents: 25 mg/day (DHHS [adult] 2013)
Treatment:
Infants and Children: Optimal dose not established, higher doses than prophylaxis are necessary for treatment of neuritis (ataxia), some clinicians have suggested the following: 100 mg/day; higher doses (ie, 200 mg/day) may be necessary to alleviate signs/symptoms
Adolescents: Initial: 100 mg/day for 3 weeks followed by 30 mg/day
Penicillamine (in Wilson Disease patients): Limited data available: Children and Adolescents: 25 to 50 mg/day (Roberts 2008)
Acute isoniazid ingestion:
Treatment of isoniazid-induced seizures and/or coma: IV: Children and Adolescents:
Acute ingestion of known amount: Initial: A total dose of pyridoxine equal to the amount of isoniazid ingested (maximum dose: 70 mg/kg up to 5 g); administer at a rate of 0.5 to 1 g/minute until seizures stop or the maximum initial dose has been administered; may repeat every 5 to 10 minutes as needed to control persistent seizure activity and/or CNS toxicity. If seizures stop prior to the administration of the calculated initial dose, infuse the remaining pyridoxine over 4 to 6 hours (Howland 2006; Morrow 2006).
Acute ingestion of unknown amount: Initial: 70 mg/kg (maximum dose: 5 g); administer at a rate of 0.5 to 1 g/minute; may repeat every 5 to 10 minutes as needed to control persistent seizure activity and/or CNS toxicity (Howland 2006; Morrow 2006; Santucci 1999)
Prevention of isoniazid-induced seizures and/or coma: IV: Children: Asymptomatic patients who present within 2 hours of ingesting a potentially toxic amount of isoniazid should receive a prophylactic dose of pyridoxine (Boyer 2006). Dosing recommendations are the same as for the treatment of symptomatic patients.
Acute intoxication; mushroom ingestion (genus Gyromitra): Children and Adolescents: IV: 25 mg/kg/dose; repeat as necessary to a maximum total dose of 15 to 20 g (Lheureaux 2005)
Extemporaneously Prepared
A 1 mg/mL oral solution may be made using pyridoxine injection. Withdraw 100 mg (1 mL of a 100 mg/mL injection) from a vial with a needle and syringe; add to 99 mL simple syrup in an amber bottle. Label "refrigerate". Stable for 30 days refrigerated.
Nahata MC, Pai VB, and Hipple TF, Pediatric Drug Formulations, 5th ed, Cincinnati, OH: Harvey Whitney Books Co, 2004.
Administration
Injection: Administer IM or IV.
Gyromitrin-containing mushroom (false morel) overdose/toxicity (treatment/prophylaxis) (off-label use): Administer dose over 15 to 30 minutes (Lheureux 2005).
Isoniazid toxicity (off-label use): Initial doses should be administered at a rate of 0.5 to 1 g/minute. If the parenteral formulation is not available, anecdotal reports suggest that pyridoxine tablets may be crushed and made into a slurry and given at the same dose orally or via nasogastric (NG) tube (Hernon 2015). Oral administration is not recommended for acutely poisoned patients with seizure activity.
Dietary Considerations
Dietary adequate Intake (AI) (IOM 1998):
1 to 6 months: 0.1 mg/day
7 to 12 months: 0.3 mg/day
Dietary recommended daily allowance (RDA) (IOM 1998):
1 to 3 years: 0.5 mg
4 to 8 years: 0.6 mg
9 to 13 years: 1 mg
14 to 18 years: Females: 1.2 mg; Males: 1.3 mg
19 to 50 years: 1.3 mg
≥51 years: Females: 1.5 mg; Males: 1.7 mg
Pregnancy: 1.9 mg
Lactation: 2 mg
Storage
Injection: Store at 20°C to 25°C (68°F to 77°F). Protect from light.
Oral: Store at room temperature. Avoid excessive heat or moisture.
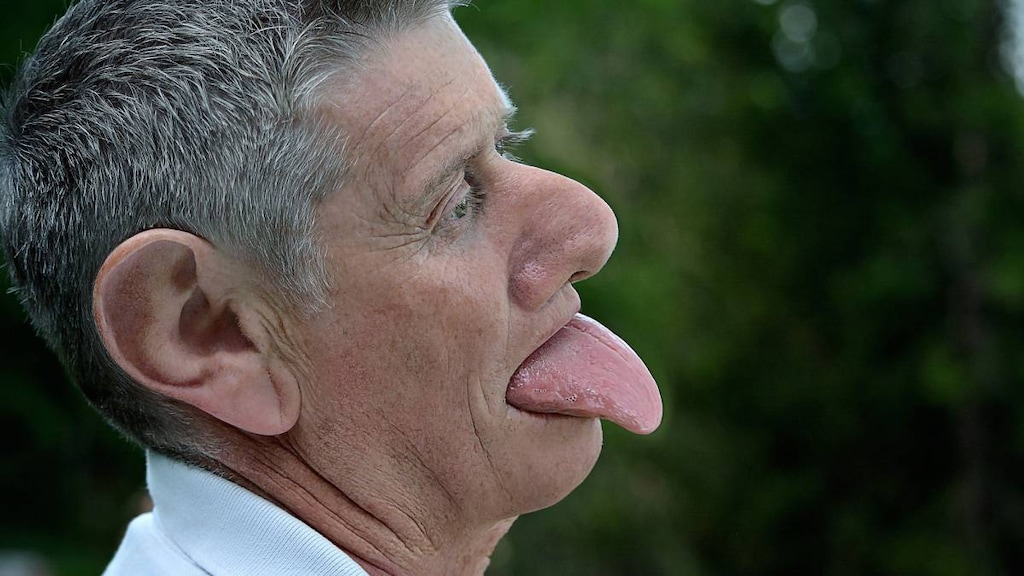
Pyridoxine Images
Drug Interactions
Altretamine: Pyridoxine may diminish the therapeutic effect of Altretamine. Specifically when altretamine is used in combination with Cisplatin the response duration may be diminished. Consider therapy modification
Barbiturates: Pyridoxine may increase the metabolism of Barbiturates. Apparent in high pyridoxine doses (eg, 200 mg/day) Monitor therapy
Fosphenytoin: Pyridoxine may increase the metabolism of Fosphenytoin. This is most apparent in high pyridoxine doses (e.g., 80 mg to 200 mg daily) Monitor therapy
Levodopa-Containing Products: Pyridoxine may diminish the therapeutic effect of Levodopa-Containing Products. Management: The concomitant use of pyridoxine and levodopa (in the absence of a dopa decarboxylase inhibitor (DDI)) should be avoided. Use of a DDI (eg, carbidopa) with levodopa will essentially eliminate the risk of this interaction. Consider therapy modification
Phenytoin: Pyridoxine may increase the metabolism of Phenytoin. This is most apparent in high pyridoxine doses (e.g., 80 mg to 200 mg daily) Monitor therapy
Adverse Reactions
Frequency not defined.
Central nervous system: Ataxia, drowsiness, headache, neuropathy, paresthesia, seizure (following very large IV doses)
Endocrine & metabolic: Acidosis, folate deficiency
Gastrointestinal: Nausea
Hepatic: Increased serum AST
Hypersensitivity: Hypersensitivity reaction
Warnings/Precautions
Concerns related to adverse effects:
- Neuropathy: Severe, permanent peripheral neuropathies have been reported; neurotoxicity is more common with long-term administration of large doses (>2 g/day) (Albin 1987).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Aluminum: The parenteral product may contain aluminum; toxic aluminum concentrations may be seen with high doses, prolonged use, or renal impairment. Premature neonates are at higher risk due to immature renal function and aluminum intake from other parenteral sources. Parenteral aluminum exposure of >4 to 5 mcg/kg/day is associated with CNS and bone toxicity; tissue loading may occur at lower doses (Federal Register 2002). See manufacturer’s labeling.
Other warnings/precautions:
- Dependence/withdrawal: Doses >200 mg/day may cause dependence and withdrawal.
- Pharmacy supply of emergency antidotes: Guidelines suggest that at least 8 to 24 g be stocked. This is enough to treat 1 patient weighing 100 kg for an initial 8- to 24-hour period. In areas where tuberculosis is common and isoniazid toxicity is more likely, hospitals should consider stocking 24 g. This is enough to treat 1 patient for 24 hours (Dart 2018).
- Vitamin deficiency: Single vitamin deficiency is rare; evaluate for other deficiencies.
Monitoring Parameters
For treatment of isoniazid or gyromitrin-containing mushroom toxicity: Anion gap, arterial blood gases, electrolytes, neurological exam, seizure activity
Pregnancy
Pregnancy Risk Factor
A
Pregnancy Considerations
Water soluble vitamins cross the placenta. Maternal pyridoxine plasma concentrations may decrease as pregnancy progresses and requirements may be increased in pregnant women (IOM 1998). Pyridoxine is used to treat nausea and vomiting of pregnancy (ACOG 189 2018; Neibyl 2010; Campbell [SOGC] 2016).
Patient Education
What is this drug used for?
- It is used to treat or prevent low vitamin B6.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Fatigue
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Burning
- Numbness feeling
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.