Boxed Warning
Increased mortality in elderly patients with dementia-related psychosis:
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. Risperidone is not approved for the treatment of patients with dementia-related psychosis and has not been studied in this population.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Prefilled Syringe, Subcutaneous:
Perseris: 90 mg (1 ea); 120 mg (1 ea)
Solution, Oral:
RisperDAL: 1 mg/mL (30 mL) [contains benzoic acid]
Generic: 1 mg/mL (30 mL)
Suspension Reconstituted ER, Intramuscular:
RisperDAL Consta: 12.5 mg (1 ea); 25 mg (1 ea); 37.5 mg (1 ea); 50 mg (1 ea)
Tablet, Oral:
RisperDAL: 0.25 mg [DSC], 0.5 mg, 1 mg [contains corn starch]
RisperDAL: 2 mg [contains corn starch, fd&c yellow #6 aluminum lake]
RisperDAL: 3 mg [contains corn starch, fd&c yellow #10 (quinoline yellow)]
RisperDAL: 4 mg [contains corn starch, fd&c blue #2 aluminum lake, fd&c yellow #10 (quinoline yellow)]
Generic: 0.25 mg, 0.5 mg, 1 mg, 2 mg, 3 mg, 4 mg
Tablet Disintegrating, Oral:
RisperDAL M-TAB: 0.5 mg [DSC], 1 mg [DSC], 2 mg [DSC], 3 mg [DSC], 4 mg [DSC] [contains aspartame, peppermint oil (mentha piperita oil)]
risperiDONE M-TAB: 0.5 mg [DSC], 1 mg [DSC], 2 mg [DSC], 3 mg [DSC], 4 mg [DSC] [contains aspartame]
Generic: 0.25 mg, 0.5 mg, 1 mg, 2 mg, 3 mg, 4 mg
Pharmacology
Mechanism of Action
Risperidone is a benzisoxazole atypical antipsychotic with high 5-HT2 and dopamine-D2 receptor antagonist activity. Alpha1, alpha2 adrenergic, and histaminergic receptors are also antagonized with high affinity. Risperidone has low to moderate affinity for 5-HT1C, 5-HT1D, and 5-HT1A receptors, weak affinity for D1 and no affinity for muscarinics or beta1 and beta2 receptors.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Rapid and well absorbed; food does not affect rate or extent
IM: <1% absorbed initially; main release occurs at ~3 weeks and is maintained from 4 to 6 weeks; release ends by 7 weeks
SubQ: Two absorption peaks; first release occurs immediately after injection and second release occurs around 10 to 14 days; therapeutic levels maintained for 4 weeks after injection.
Distribution
Vd: 1 to 2 L/kg
Metabolism
Extensively hepatic via CYP2D6 to 9-hydroxyrisperidone (similar pharmacological activity as risperidone); N-dealkylation is a second minor pathway; Note: 9-hydroxyrisperidone is the predominant circulating form and is approximately equal to risperidone in receptor binding activity; clinical effects are from combined concentrations of risperidone and 9-hydroxyrisperidone; clinically important differences between CYP2D6 poor and extensive metabolizers are not expected (pharmacokinetics of the sum of risperidone and 9-hydroxyrisperidone were similar in poor and extensive metabolizers)
Excretion
Urine (70%); feces (14%)
Time to Peak
Oral: Risperidone: Within 1 hour; 9-hydroxyrisperidone: Extensive metabolizers: 3 hours; Poor metabolizers: 17 hours
SubQ: Risperidone: First peak: 4 to 6 hours; Second peak: 10 to 14 days
Half-Life Elimination
Active moiety (risperidone and its active metabolite 9-hydroxyrisperidone):
Oral: 20 hours (mean); prolonged in elderly patients
Extensive metabolizers: Risperidone: 3 hours; 9-hydroxyrisperidone: 21 hours
Poor metabolizers: Risperidone: 20 hours; 9-hydroxyrisperidone: 30 hours
IM: 3 to 6 days; related to microsphere erosion and subsequent absorption of risperidone
Risperidone: SubQ: 9 to 11 days
Protein Binding
Plasma: Risperidone 90%; 9-hydroxyrisperidone: 77%; Note: Risperidone free fraction may be increased by ~35% in patients with hepatic impairment due to decreased concentrations of albumin and alpha-1 acid glycoprotein
Use in Specific Populations
Special Populations: Renal Function Impairment
Moderate to severe
Cl of parent drug and active metabolite decreased 60%.
Special Populations: Hepatic Function Impairment
Mean free fraction of risperidone in plasma increased approximately 35%.
Special Populations: Elderly
Oral
Renal clearance of parent drug and active metabolite was decreased.
Use: Labeled Indications
Long-acting IM injection:
Bipolar disorder: As monotherapy or as adjunctive therapy to lithium or valproate for the maintenance treatment of bipolar I disorder.
Schizophrenia: Treatment of schizophrenia.
Oral:
Bipolar mania: As monotherapy or as adjunctive therapy to lithium or valproate for the treatment of acute manic or mixed episodes associated with bipolar disorder in adults or as monotherapy for the treatment of acute manic or mixed episodes associated with bipolar disorder in children and adolescents 10 to 17 years of age.
Irritability associated with autistic disorder: For the treatment of irritability associated with autistic disorder in children and adolescents 5 to 17 years of age, including symptoms of aggression toward others, deliberate self-injuriousness, temper tantrums, and quickly changing moods.
Schizophrenia: For the treatment of schizophrenia in adults and adolescents 13 to 17 years of age.
Use: Off Label
Agitation/Aggression (severe, acute) associated with psychiatric disorders (eg, schizophrenia, bipolar disorder), substance intoxication, or other organic causescyes
Data from a limited number of randomized, open-label trials suggest that oral risperidone may be as effective as other antipsychotics, including IM formulations, as monotherapy or in combination with benzodiazepines for the treatment of acute agitation or aggression in patients with psychiatric disorders Currier 2004, Hsu 2010, Lim 2010.
Based on the World Federation of Societies of Biological Psychiatry (WFSBP) expert consensus on the management of agitation in psychiatry, oral antipsychotics, such as risperidone, are recommended for the management of agitation. The WFSBP guidelines for the biological treatment of schizophrenia recommend antipsychotics as monotherapy or in combination with benzodiazepines for the treatment of acute agitation in patients with schizophrenia.
Agitation/Aggression and psychosis associated with dementia, severe or refractorybyes
Data from randomized, double-blind, placebo-controlled trials support the use of risperidone in the treatment of psychosis/agitation related to dementia Brodaty 2003, Katz 1999, Sultzer 2008.
Based on the American Psychiatric Association (APA) practice guideline on the use of antipsychotics to treat agitation or psychosis in patients with dementia, antipsychotics, such as risperidone, may be considered for the treatment of agitation and psychosis in certain patients; however, evidence for efficacy is modest and use should be limited to patients whose symptoms are dangerous, severe, or cause significant patient distress due to safety risks associated with antipsychotics. Based on the WFSBP guidelines for the biological treatment of Alzheimer disease and other dementias, drug treatment with risperidone for behavioral and psychological aspects (including hyperactivity and psychosis) is recommended at low doses and for short durations, as a last option after addressing causative factors and using psychosocial interventions.
Bipolar disorder, hypomaniacyes
Data from a limited number of open-label clinical studies suggest that risperidone as monotherapy or in combination with a second mood-stabilizing medication may be beneficial in the treatment of hypomania Bahk 2004, Vieta 2001, Vieta 2002.
Based on the WFSBP guidelines for the biological treatment of bipolar disorders update on the treatment of acute mania and the Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders 2018 guidelines for the management of patients with bipolar disorder, limited evidence exists for the treatment of hypomania; however, based on clinical experience, treatment should be the same as mania and clinicians should consider antipsychotics, such as risperidone, and/or antimanic agents.
Delusional disorderc
Data from a retrospective study suggest that risperidone may be beneficial for the treatment of persistent delusional disorder Kulkarni 2017.
Delusional infestation (delusional parasitosis)c
Data from a limited number of patients studied in case reports suggest that risperidone may be beneficial for the treatment of delusional infestation (also called delusional parasitosis)
Huntington disease–associated choreac
Data from one observational study, an open-label, retrospective study, and a small number of patients in case reports suggest that risperidone may be beneficial for the treatment of chorea associated with Huntington disease Cankurtaran 2006, Dallocchio 1999, Duff 2008, Erdemoglu 2002, Parsa 1997, Reveley 1996, Schultz 2018.
Major depressive disorder (unipolar), treatment resistantbyes
Data from 2 meta-analyses of 4 randomized, double-blind, placebo-controlled trials support the use of adjunctive risperidone (in combination with antidepressants) in the treatment of treatment-resistant major depressive disorder (MDD) Komossa 2010, Nelson 2009.
Based on the US Veterans Affairs/Department of Defense clinical practice guideline for the management of MDD, second-generation antipsychotics, such as risperidone, should be considered as an antidepressant augmentation strategy only after other strategies have failed due to tolerability issues. Alternatively, the CANMAT clinical guidelines for the management of adults with MDD recommend antidepressant augmentation with risperidone as a first-line option in patients with a nonresponse or partial response to antidepressant monotherapy.
Obsessive-compulsive disorder, treatment resistantcyes
Data from a limited number of patients studied in randomized, double-blind trials suggest that risperidone may be beneficial for the treatment of obsessive-compulsive disorder (OCD) as an adjunct treatment in patients with a partial response to antidepressants Erzegovesi 2005, Li 2005, McDougle 2000.
Based on the 2006 APA practice guideline for the treatment of patients with OCD, the 2013 APA guideline watch, and the 2014 Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress, and obsessive-compulsive disorders, adjunctive therapy with second-generation antipsychotics such as risperidone is recommended for patients with a moderate response to antidepressants.
Tourette syndromebyes
Data from small, double-blind, randomized, controlled trials support the use of risperidone in the treatment of Tourette syndrome Bruggeman 2001, Dion 2002, Scahill 2003.
Based on the American Academy of Neurology practice guideline recommendations summary for the treatment of tics in people with Tourette syndrome and chronic tic disorders, antipsychotics such as risperidone are recommended for the management of tics when the benefit outweighs the risks of treatment. Based on the European Society for the Study of Tourette Syndrome and the Tourette Syndrome Foundation of Canada guidelines, drug therapy, including risperidone, is effective and recommended for the management of Tourette syndrome to improve quality of life with tics that are painful or distressing, interfere with daily functioning, or cause sustained social or emotional problems. Of the atypical antipsychotics, risperidone has the best evidence of efficacy for Tourette syndrome; however, Canadian guidelines consider risperidone a second-line option due to its adverse effect profile and recommend avoiding use in patients who are overweight at baseline.
Contraindications
Hypersensitivity to risperidone, paliperidone, or any component of the formulation
Dosage and Administration
Dosing: Adult
Note: Although manufacturer's labeling includes a maximum dose of up to 16 mg/day, doses >8 mg/day are generally not recommended (Jibson 2019).
Agitation/Aggression (severe, acute) associated with psychiatric disorders (eg, schizophrenia, bipolar disorder), substance intoxication, or other organic causes (alternative agent) (off-label use):
Note: Antipsychotics are appropriate when psychosis is suspected to be the primary cause of agitation/aggression (WFSBP [Hasan 2012]; Wilson 2012a). Other agents are used preferentially in some intoxications (eg, stimulants) or alcohol withdrawal (Moore 2019; WFSBP [Garriga 2016]; Wilson 2012b). Depending on presentation, may combine with a benzodiazepine.
Oral: Initial: 1 to 2 mg; may repeat every 2 hours to a maximum daily dose of 6 mg (Lim 2010; Moore 2019; Wilson 2012a).
Agitation/Aggression and psychosis associated with dementia, severe or refractory (alternative agent) (off-label use):
Note: For short-term use while addressing underlying causes of severe symptoms (APA [Reus 2016]). In patients without a clinically significant response after an adequate trial (eg, up to 4 weeks), taper and withdraw therapy. Only continue in patients with demonstrated benefit; attempt to taper and withdraw at regular intervals (eg, ≤4 months) (APA [Reus 2016]). In dementia with Lewy bodies, antipsychotics are generally avoided. If use is required, doses >0.5 mg/day are not recommended (Farlow 2019).
Oral: Initial: 0.5 mg/day in 2 divided doses; may increase dose based on response and tolerability in increments of 0.5 mg/day at intervals ≥2 days up to 1 mg/day (APA [Reus 2016]; Brodaty 2003; Katz 1999).
Bipolar disorder:
Acute manic or mixed episodes (labeled use) or acute hypomania (off-label use) (monotherapy or adjunctive therapy):
Oral: Initial: 1 to 3 mg/day in 1 or 2 divided doses; may adjust dose based on response and tolerability in increments of 1 mg/day at intervals ≥24 hours to a usual dose of 4 to 6 mg/day; in general, assess full effect for ≥1 week before further advancing up to 8 mg/day (usual maximum) (CANMAT [Yatham 2018]; Moosavi 2014; Singh 2013).
Maintenance treatment (monotherapy or as adjunct to antimanic therapy):
Oral: Continue dose and combination regimen that was used to achieve control of the acute episode (CANMAT [Yatham 2018]).
IM ER suspension (alternative route):
Note: Establish tolerability using oral risperidone before first injection. Due to delayed onset of the first ER IM injection, an oral antipsychotic at an effective dose is overlapped for the first 3 weeks.
Initial: 25 mg every 2 weeks; in patients with a history of treatment-refractory illness or requiring high doses of antipsychotics, some experts initiate at 37.5 mg (Hawley 2010). If insufficient response, may increase dose in increments of 12.5 mg no sooner than every 4 weeks to a maximum dose of 50 mg every 2 weeks (Hawley 2010; Turner 2004).
Delusional disorder (alternative agent) (off-label use):
Oral: Initial: 1 to 2 mg/day in 1 or 2 divided doses; may increase dose based on response and tolerability in increments of 1 mg/day every 2 weeks; usual dose is ~5 mg/day in 2 divided doses; maximum dose: 8 mg/day (Fear 2002; Kulkarni 2017; Songer 1996; Stroup 2019).
Delusional infestation (delusional parasitosis) (off-label use):
Oral: Initial: 0.5 mg/day in 1 or 2 divided doses; may increase dose based on response and tolerability gradually (ie, weekly) up to 2 to 4 mg/day in 1 or 2 divided doses. Doses up to 8 mg/day may be necessary in some patients (Freudenmann 2008; Kenchaiah 2010; Suh 2019). After achieving adequate response, maintain for at least 1 to 3 months before attempting to taper (Suh 2019).
Huntington disease–associated chorea, moderate to severe (alternative agent) (off-label use):
Oral: Initial: 0.5 to 2 mg/day in 1 or 2 divided doses; may increase dose based on response and tolerability in increments of 1 mg/day every week; some patients may require doses up to 10 mg/day (Parsa 1997; Reveley 1996; Suchowersky 2019).
Major depressive disorder (unipolar), treatment resistant (adjunctive therapy with antidepressant) (off-label use):
Oral: Initial: 0.25 to 0.5 mg/day; may increase dose based on response and tolerability in increments of 0.25 to 1 mg/day every 3 to 7 days up to 3 mg/day. Usual effective dose: 1 to 1.5 mg/day (Keitner 2009; Mahmoud 2007).
Obsessive-compulsive disorder, treatment resistant (augmentation to antidepressants) (off-label use):
Oral: Initial: 0.25 to 0.5 mg/day; may increase dose based on response and tolerability in increments of 0.5 to 1 mg/day every 3 to 7 days; usual dose: 0.5 to 2 mg/day; doses up to 3 mg/day may be needed for optimal response (Erzegovesi 2005; McDougle 2000; Simpson 2013).
Schizophrenia:
Oral: Initial: 1 to 2 mg/day in 1 to 2 divided doses; may increase by 1 to 2 mg/day at intervals ≥24 hours to usual dosage range of 2 to 6 mg/day. In general, assess full effect for ≥1 week before further advancing, if needed, to 6 to 8 mg/day (usual maximum). Note: Doses up to 16 mg/day have been evaluated in clinical trials and are approved according to manufacturer's labeling but are associated with increased adverse effects and generally are not recommended (Robinson 2015; WFSBP [Hasan 2012]).
IM ER suspension:
Note: Establish tolerability using oral risperidone before first injection. Due to delayed onset of the first ER IM injection, an oral antipsychotic at an effective dose is overlapped for the first 3 weeks.
Initial: 25 mg every 2 weeks; may increase dose based on response and tolerability in increments of 12.5 to 25 mg every 4 weeks; maximum dose: 50 mg every 2 weeks (manufacturer's labeling). Dosage adjustments should not be made more frequently than every 4 weeks.
SubQ: Usual dose: 90 or 120 mg once monthly. Do not administer more than one 90 or 120 mg injection per month. Note: Establish tolerability with oral risperidone before starting SubQ injection. Neither a loading dose nor overlap with oral risperidone is needed.
Tourette syndrome, management of tics (off-label use):
Oral: Initial: 0.25 to 0.5 mg/day; may increase gradually based on response and tolerability in increments of ≤1 mg/day every ≥2 days up to 6 mg/day; usual dose: 2.5 to 4 mg/day (Bruggeman 2001; Dion 2002; Roessner 2011; Scahill 2003).
Discontinuation of therapy: Gradual dose reduction is advised to avoid withdrawal symptoms (ie, insomnia, headache, GI symptoms), unless discontinuation is due to significant adverse effects. In general, when discontinuing antipsychotic therapy for a chronic psychiatric disorder (eg, schizophrenia, bipolar disorder), decreasing the dose very gradually over weeks to months (eg, reducing the dose by 10% per month) with close monitoring is suggested to allow for detection of prodromal symptoms of disease recurrence (APA [Lehman 2004]; CPA 2005).
Switching antipsychotics: An optimal universal strategy for switching antipsychotic agents has not been established. Strategies include cross-titration (gradually discontinuing the first antipsychotic while gradually increasing the new antipsychotic) and abrupt change (abruptly discontinuing the first antipsychotic and either increasing the new antipsychotic gradually or starting it at a treatment dose). In patients with schizophrenia at high risk of relapse, the current medication may be maintained at full dose as the new medication is increased (ie, overlap); once the new medication is at therapeutic dose, the first medication is gradually decreased and discontinued over 1 to 2 weeks (Cerovecki 2013; Remington 2005; Takeuchi 2017). Based on clinical experience, some experts generally prefer cross-titration and overlap approaches rather than abrupt change (Post 2019; Stroup 2019).
Conversion between oral and IM extended release: The manufacturer's labeling does not provide dose conversions to IM extended release based on current oral dose. Some experts recommend converting to IM extended release at the usual starting dose and titrating according to response (Lauriello 2019). See indication-specific dosing for schizophrenia and bipolar disorder above for initial dosing and overlap recommendations.
Conversion between oral and SubQ extended release:
Oral dose of 3 mg/day is equivalent to SubQ injection of 90 mg once monthly.
Oral dose of 4 mg/day is equivalent to SubQ injection of 120 mg once monthly.
Dosing: Geriatric
Bipolar mania (monotherapy or as an adjunct to lithium or divalproex):
Oral: Initial: 0.5 mg twice daily; titrate slowly. Note: Limiting initial dose to 1 mg/day (in 2 divided doses) may reduce the risk of orthostatic hypotension/syncope. Additional monitoring of renal function and orthostatic blood pressure may be warranted.
IM: Refer to adult dosing.
Schizophrenia:
Oral: Initial: 0.5 mg twice daily; titrate slowly. Note: Limiting initial dose to 1 mg/day (in 2 divided doses) may reduce the risk of orthostatic hypotension/syncope. Additional monitoring of renal function and orthostatic blood pressure may be warranted.
IM, SubQ: Refer to adult dosing.
Dosing: Pediatric
Autism, associated irritability, including aggression, temper, tantrums, self-injurious behavior, and quickly changing moods:
Children ≥5 years and Adolescents: Note: Individualize dose according to patient response and tolerability:
15 to 20 kg: Oral: Initial: 0.25 mg/day; after ≥4 days, may increase dose to 0.5 mg/day; maintain this dose for ≥14 days. In patients not achieving sufficient clinical response, may increase dose in increments of 0.25 mg/day at ≥2-week intervals. Doses ranging from 0.5 to 3 mg/day have been evaluated; however, therapeutic effect reached plateau at 1 mg/day in clinical trials. Following clinical response, consider gradually decreasing dose to lowest effective dose. May be administered once daily or in divided doses twice daily.
≥20 kg: Oral: Initial: 0.5 mg/day; after ≥4 days, may increase dose to 1 mg/day; maintain this dose for ≥14 days. In patients not achieving sufficient clinical response, may increase dose in increments of 0.5 mg/day at ≥2-week intervals. Doses ranging from 0.5 to 3 mg/day have been evaluated; however, therapeutic effect reached plateau at 2.5 mg/day (3 mg/day in pediatric patients >45 kg) in clinical trials. Following clinical response, consider gradually decreasing to lowest effective dose. May be administered once daily or in divided doses twice daily.
Bipolar mania: Children and Adolescents 10 to 17 years: Oral: Initial: 0.5 mg once daily; dose may be adjusted if needed, in increments of 0.5 to 1 mg/day at intervals ≥24 hours, as tolerated, to a dose of 2.5 mg/day. Doses ranging from 0.5 to 6 mg/day have been evaluated; however, doses >2.5 mg/day do not confer additional benefit and are associated with increased adverse events; doses >6 mg/day have not been studied. Note: May administer 1/2 the daily dose twice daily in patients who experience persistent somnolence.
Delirium: Limited data available; optimal dose not established; experience suggests risperidone be considered for hypoactive or mixed delirium (Karnik 2007; Kishk 2019; Smith 2013) dosing should be individualized to response and decreased as soon as appropriate (Kishk 2019; Schieveld 2007; Simone 2017; Turkel 2012; Turkel 2014):
Infants: Very limited data available: Oral: 0.05 to 0.1 mg once daily at bedtime or twice daily (Turkel 2013). Dosing based on experience with implementation of PICU assessment scales and treatment protocols, small open-label trials which included infants, and case series (Kishk 2019; Schieveld 2007; Turkel 2013).
Children <5 years: Oral: Initial: 0.1 to 0.2 mg once daily at bedtime; doses may be increased based upon response; dosing based on experience with implementation of PICU assessment scales and treatment protocols, small open-label trials, and expert recommendations (Kishk 2019; Schieveld 2007; Simone 2017; Turkel 2012; Turkel 2014).
Children ≥5 years and Adolescents: Oral: Initial: 0.2 to 0.5 mg once daily at bedtime; may titrate to lowest effective dose every 1 to 2 days; usual range: 0.2 to 2.5 mg/day in divided doses 2 to 4 times daily; some have suggested maximum daily dose dependent upon patient weight: <20 kg: 1 mg/day; 20 to 45 kg: 2.5 mg/day; >45 kg: 3 mg/day (Karnik 2007; Kishk 2019; Schieveld 2007; Shin 2016; Silver 2010; Turkel 2012; Turkel 2014).
Disruptive behavior disorders (eg, conduct disorder, oppositional defiant disorder): Limited data available: Children ≥4 years and Adolescents: Oral: Initial: 0.01 mg/kg/dose once daily for 2 days, then 0.02 mg/kg/dose once daily, may further increase on weekly basis as tolerated to 0.06 mg/kg/dose once daily; usual maximum daily dose: 2 mg/day; improvement in target symptoms typically within 1 to 4 weeks (Aman 2002; Findling 2004; Kutcher 2004; Pandina 2006). Note: May administer 1/2 the daily dose twice daily if breakthrough symptoms occur in the afternoon or evening.
Pervasive developmental disorders (eg, disruptive behavior, aggression, irritability): Limited data available: Children ≥5 years and Adolescents: Oral: Initial: 0.01 mg/kg/dose once daily for 2 days, then 0.02 mg/kg/dose once daily; may further increase on weekly basis by ≤0.02 mg/kg/day increments as tolerated to 0.06 mg/kg/dose once daily; reported mean dose: 0.05 mg/kg/day (1.48 mg/day); other trials have reported similar optimal doses: 0.75 to 1.8 mg/day; improvement in target symptoms typically within 2 to 4 weeks (Fisman 1996; McDougle 1997; Shea 2004). Note: May administer 1/2 the daily dose twice daily if breakthrough symptoms occur in the afternoon or evening.
Schizophrenia: Adolescents 13 to 17 years: Oral: Initial: 0.5 mg once daily; dose may be adjusted if needed, in increments of 0.5 to 1 mg/day at intervals ≥24 hours, as tolerated, to a dose of 3 mg/day. Doses ranging from 1 to 6 mg/day have been evaluated; however, doses >3 mg/day do not confer additional benefit and are associated with increased adverse events. Note: May administer 1/2 the daily dose twice daily in patients who experience persistent somnolence.
Tourette syndrome, tics: Limited data available: Children ≥7 years and Adolescents: Oral: Initial: 0.25 to 0.5 mg once daily at night; may gradually titrate every 4 to 5 days in 0.25 to 0.5 mg increments to usual reported therapeutic range: 0.25 to 6 mg/day divided in twice daily doses (Dion 2002; Roessner 2011; Scahill 2003; Singer 2010).
Discontinuation of therapy: Children and Adolescents: American Academy of Child and Adolescent Psychiatry (AACAP), American Psychiatric Association (APA), Canadian Psychiatric Association (CPA), National Institute for Health and Care Excellence (NICE), and World Federation of Societies of Biological Psychiatry (WFSBP) guidelines recommend gradually tapering antipsychotics to avoid withdrawal symptoms and minimize the risk of relapse (AACAP [McClellan 2007]; APA [Lehman 2004]; Cerovecki 2013; CPA 2005; NICE 2013; WFSBP [Hasan 2012]); risk for withdrawal symptoms may be highest with highly anticholinergic or dopaminergic antipsychotics (Cerovecki 2013). When stopping antipsychotic therapy in patients with schizophrenia, the CPA guidelines recommend a gradual taper over 6 to 24 months and the APA guidelines recommend reducing the dose by 10% each month (APA [Lehman 2004]; CPA 2005). Continuing antiparkinsonism agents for a brief period after discontinuation may prevent withdrawal symptoms (Cerovecki 2013). When switching antipsychotics, three strategies have been suggested: Cross-titration (gradually discontinuing the first antipsychotic while gradually increasing the new antipsychotic), overlap and taper (maintaining the dose of the first antipsychotic while gradually increasing the new antipsychotic, then tapering the first antipsychotic), and abrupt change (abruptly discontinuing the first antipsychotic and either increasing the new antipsychotic gradually or starting it at a treatment dose). Evidence supporting ideal switch strategies and taper rates is limited and results are conflicting (Cerovecki 2013; Remington 2005).
Reconstitution
IM: Do not substitute any components of the dose pack. Bring to room temperature for ≥30 minutes prior to reconstitution (do not warm any other way). Reconstitute with provided diluent only. Refer to the manufacturer's labeling for device assembly and reconstitution instructions. Do not store suspension after reconstitution; administer immediately after reconstitution.
SubQ: Reconstitute immediately prior to administration. Bring kit to room temperature ≥15 minutes prior to preparation. Refer to the manufacturer's labeling for reconstitution instructions. Administer immediately after mixing.
Administration
Oral: May be administered without regard to meals.
Oral solution can be administered directly from the provided calibrated pipette or may be mixed with water, coffee, orange juice, or low-fat milk, but is not compatible with cola or tea.
Risperdal M-Tab should not be removed from blister pack until administered. Do not push tablet through foil (tablet may become damaged); peel back foil to expose tablet. Using dry hands, place immediately on tongue. Tablet will dissolve within seconds and may be swallowed with or without liquid. Do not split or chew.
IM: Shake syringe vigorously just before injection. Administer IM into either the deltoid muscle or the upper outer quadrant of the gluteal area. For IM use only; do not administer IV. Avoid inadvertent injection into vasculature. Injection should alternate between the two arms or buttocks. Do not combine two different dosage strengths into one single administration. Do not substitute any components of the dose-pack; administer with needle provided (1-inch needle for deltoid administration or 2-inch needle for gluteal administration). Administer entire contents of the vial to ensure correct dose is provided.
SubQ: Administer SubQ into the abdomen only. Choose an injection site with adequate subcutaneous tissue that is free of skin conditions (eg, bruising, excessive pigment, infection, irritation, lesions, nodules, redness, or scarring). It is recommended that the patient is in the supine position. Rotate injection sites. There may be a lump at the injection site for several weeks; this will decrease in size over time. Do not rub injection site; be aware of the placement of any belts or clothing waistbands.
Dietary Considerations
May be taken without regard to meals. Dispersible tablets contain phenylalanine.
Storage
Injection:
IM: Store at 2°C to 8°C (36°F to 46°F) and protect from light. May be stored at 25°C (77°F) for up to 7 days prior to administration; do not expose unrefrigerated product to temperatures above 77°F (25°C). Following reconstitution, administer immediately (do not store for future use).
SubQ: Store at 2°C to 8°C (36°F to 46°F). Unopened package may be stored at 20°C to 25°C (68°F to 77°F) for up to 7 days prior to administration. Allow kit to come to room temperature for at least 15 minutes prior to mixing.
Oral solution, tablet: Store at 15°C to 25°C (59°F to 77°F). Protect from light and moisture. Keep orally-disintegrating tablets sealed in foil pouch until ready to use. Do not freeze solution.
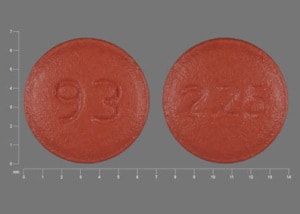
RisperiDONE Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Acetylcholinesterase Inhibitors: May diminish the therapeutic effect of Anticholinergic Agents. Anticholinergic Agents may diminish the therapeutic effect of Acetylcholinesterase Inhibitors. Monitor therapy
Acetylcholinesterase Inhibitors (Central): May enhance the neurotoxic (central) effect of Antipsychotic Agents. Severe extrapyramidal symptoms have occurred in some patients. Monitor therapy
Aclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Amisulpride: Antipsychotic Agents may enhance the adverse/toxic effect of Amisulpride. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Avoid combination
Amisulpride: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Avoid combination
Amphetamines: Antipsychotic Agents may diminish the stimulatory effect of Amphetamines. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of other Anticholinergic Agents. Monitor therapy
Antidiabetic Agents: Hyperglycemia-Associated Agents may diminish the therapeutic effect of Antidiabetic Agents. Monitor therapy
Anti-Parkinson Agents (Dopamine Agonist): Antipsychotic Agents (Second Generation [Atypical]) may diminish the therapeutic effect of Anti-Parkinson Agents (Dopamine Agonist). Management: Consider using an alternative antipsychotic agent when possible in patients with Parkinson disease. If an atypical antipsychotic is necessary, consider using clozapine or quetiapine, which may convey the lowest interaction risk. Consider therapy modification
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Blood Pressure Lowering Agents: May enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Botulinum Toxin-Containing Products: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the adverse/toxic effect of Antipsychotic Agents. Avoid combination
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Ceritinib: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Chloral Betaine: May enhance the adverse/toxic effect of Anticholinergic Agents. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Cimetropium: Anticholinergic Agents may enhance the anticholinergic effect of Cimetropium. Avoid combination
Clarithromycin: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Clarithromycin. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CloZAPine: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of CloZAPine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Strong): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
CYP3A4 Inducers (Strong): May decrease the serum concentration of RisperiDONE. Management: Consider increasing the dose of oral risperidone (to no more than double the original dose) if a strong CYP3A4 inducer is initiated. For patients on IM risperidone, consider an increased IM dose or supplemental doses of oral risperidone. Consider therapy modification
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Darunavir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Deutetrabenazine: May enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, the risk for akathisia, parkinsonism, or neuroleptic malignant syndrome may be increased. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Domperidone: QT-prolonging Agents (Moderate Risk) may enhance the QTc-prolonging effect of Domperidone. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Droperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Eluxadoline: Anticholinergic Agents may enhance the constipating effect of Eluxadoline. Avoid combination
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Fexinidazole [INT]: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Flupentixol: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Flupentixol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Gastrointestinal Agents (Prokinetic): Anticholinergic Agents may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
Glucagon: Anticholinergic Agents may enhance the adverse/toxic effect of Glucagon. Specifically, the risk of gastrointestinal adverse effects may be increased. Monitor therapy
Glycopyrrolate (Oral Inhalation): Anticholinergic Agents may enhance the anticholinergic effect of Glycopyrrolate (Oral Inhalation). Avoid combination
Glycopyrronium (Topical): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Guanethidine: Antipsychotic Agents may diminish the therapeutic effect of Guanethidine. Monitor therapy
Haloperidol: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Haloperidol. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Ipratropium (Oral Inhalation): May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Itopride: Anticholinergic Agents may diminish the therapeutic effect of Itopride. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Levosulpiride: Anticholinergic Agents may diminish the therapeutic effect of Levosulpiride. Avoid combination
Lithium: May enhance the neurotoxic effect of Antipsychotic Agents. Lithium may decrease the serum concentration of Antipsychotic Agents. Specifically noted with chlorpromazine. Monitor therapy
Loop Diuretics: May enhance the adverse/toxic effect of RisperiDONE. Monitor therapy
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mequitazine: Antipsychotic Agents may enhance the arrhythmogenic effect of Mequitazine. Management: Consider alternatives to one of these agents when possible. While this combination is not specifically contraindicated, mequitazine labeling describes this combination as discouraged. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methylphenidate: Antipsychotic Agents may enhance the adverse/toxic effect of Methylphenidate. Methylphenidate may enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Metoclopramide: May enhance the adverse/toxic effect of Antipsychotic Agents. Avoid combination
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
MetyroSINE: May enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Mianserin: May enhance the anticholinergic effect of Anticholinergic Agents. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mirabegron: Anticholinergic Agents may enhance the adverse/toxic effect of Mirabegron. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nitroglycerin: Anticholinergic Agents may decrease the absorption of Nitroglycerin. Specifically, anticholinergic agents may decrease the dissolution of sublingual nitroglycerin tablets, possibly impairing or slowing nitroglycerin absorption. Monitor therapy
OLANZapine: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of OLANZapine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Ondansetron: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxatomide: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paliperidone: RisperiDONE may enhance the adverse/toxic effect of Paliperidone. Management: Additive paliperidone exposure is expected with this combination. Consider using an alternative combination when possible. Consider therapy modification
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Pentamidine (Systemic): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Perhexiline: CYP2D6 Substrates (High risk with Inhibitors) may increase the serum concentration of Perhexiline. Perhexiline may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Pimozide: May enhance the QTc-prolonging effect of QT-prolonging Agents (Moderate Risk). Avoid combination
Piribedil: Antipsychotic Agents may diminish the therapeutic effect of Piribedil. Piribedil may diminish the therapeutic effect of Antipsychotic Agents. Management: Use of piribedil with antiemetic neuroleptics is contraindicated, and use with antipsychotic neuroleptics, except for clozapine, is not recommended. Avoid combination
Potassium Chloride: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Chloride. Management: Patients on drugs with substantial anticholinergic effects should avoid using any solid oral dosage form of potassium chloride. Avoid combination
Potassium Citrate: Anticholinergic Agents may enhance the ulcerogenic effect of Potassium Citrate. Avoid combination
Pramlintide: May enhance the anticholinergic effect of Anticholinergic Agents. These effects are specific to the GI tract. Consider therapy modification
QT-prolonging Agents (Highest Risk): May enhance the CNS depressant effect of RisperiDONE. QT-prolonging Agents (Highest Risk) may enhance the QTc-prolonging effect of RisperiDONE. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: QuiNIDine. Consider therapy modification
QT-prolonging Antidepressants (Moderate Risk): QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Antidepressants (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Antipsychotics (Moderate Risk): May enhance the QTc-prolonging effect of RisperiDONE. QT-prolonging Antipsychotics (Moderate Risk) may increase the serum concentration of RisperiDONE. Specifically, thioridazine may increase concentrations of risperidone. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Amisulpride; CloZAPine; Droperidol; Flupentixol; OLANZapine; Pimozide; QUEtiapine; RisperiDONE. Monitor therapy
QT-prolonging Class IC Antiarrhythmics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Kinase Inhibitors (Moderate Risk): QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of QT-prolonging Kinase Inhibitors (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Miscellaneous Agents (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Exceptions: Domperidone. Monitor therapy
QT-prolonging Moderate CYP3A4 Inhibitors (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QT-prolonging Quinolone Antibiotics (Moderate Risk): May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QUEtiapine: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of QUEtiapine. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Quinagolide: Antipsychotic Agents may diminish the therapeutic effect of Quinagolide. Monitor therapy
QuiNIDine: May enhance the QTc-prolonging effect of RisperiDONE. QuiNIDine may increase the serum concentration of RisperiDONE. Management: Consider alternatives to this drug combination. If combined, monitor for QTc interval prolongation and ventricular arrhythmias. Patients with additional risk factors for QTc prolongation may be at even higher risk. Consider therapy modification
Ramosetron: Anticholinergic Agents may enhance the constipating effect of Ramosetron. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Revefenacin: Anticholinergic Agents may enhance the anticholinergic effect of Revefenacin. Avoid combination
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Saquinavir: QT-prolonging Antipsychotics (Moderate Risk) may enhance the QTc-prolonging effect of Saquinavir. Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Secretin: Anticholinergic Agents may diminish the therapeutic effect of Secretin. Management: Avoid concomitant use of anticholinergic agents and secretin. Discontinue anticholinergic agents at least 5 half-lives prior to administration of secretin. Consider therapy modification
Selective Serotonin Reuptake Inhibitors: May decrease the metabolism of RisperiDONE. Exceptions: Citalopram; Escitalopram; FluvoxaMINE. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Serotonergic Agents (High Risk): May enhance the adverse/toxic effect of Antipsychotic Agents. Specifically, serotonergic agents may enhance dopamine blockade, possibly increasing the risk for neuroleptic malignant syndrome. Antipsychotic Agents may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Sulpiride: Antipsychotic Agents may enhance the adverse/toxic effect of Sulpiride. Avoid combination
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrabenazine: May enhance the adverse/toxic effect of Antipsychotic Agents. Monitor therapy
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Thiazide and Thiazide-Like Diuretics: Anticholinergic Agents may increase the serum concentration of Thiazide and Thiazide-Like Diuretics. Monitor therapy
Tiotropium: Anticholinergic Agents may enhance the anticholinergic effect of Tiotropium. Avoid combination
Topiramate: Anticholinergic Agents may enhance the adverse/toxic effect of Topiramate. Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Umeclidinium: May enhance the anticholinergic effect of Anticholinergic Agents. Avoid combination
Valproate Products: May enhance the adverse/toxic effect of RisperiDONE. Generalized edema has developed. Monitor therapy
Verapamil: May increase the serum concentration of RisperiDONE. Monitor therapy
Voriconazole: May enhance the QTc-prolonging effect of QT-prolonging Antipsychotics (Moderate Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
>10%:
Central nervous system: Sedation (children and adolescents: 12% to 63%; adults: 5% to 11%), drowsiness (adults: 5% to 41%), drug-induced extrapyramidal reaction (2% to 35%), insomnia (≤32%), fatigue (children and adolescents: 18% to 31%; adults: 1% to 9%), parkinsonian-like syndrome (children and adolescents: 6% to 28% ; adults: 8% to 25%), headache (12% to 21%), anxiety (adults ≤16%; children and adolescents: 6% to 8%), dizziness (3% to 16%), drooling (children: 12%; adults: <4%), akathisia (3% to 11%)
Endocrine & metabolic: Hyperprolactinemia (children and adolescents: 49% to 87%; adults: <4%), weight gain (≥7% kg increase from baseline: adults: 8% to 42%; children: 8% to 33%)
Gastrointestinal: Increased appetite (children and adolescents: 4% to 44%; adults: 2% to 4%), vomiting (children and adolescents: 10% to 20%; adults <4%), constipation (5% to 17%), upper abdominal pain (adolescents: 13% to 16%), nausea (3% to 16%)
Genitourinary: Urinary incontinence (children: 16%; adults <4%)
Neuromuscular & skeletal: Tremor (adults: ≤24%; children and adolescents: ≤11%; including head titubation)
Respiratory: Nasopharyngitis (children: 19%; adults: ≤4%), cough (children: ≤17%; adults: ≤4%), rhinorrhea (children: 12%; adults: <4%)
Miscellaneous: Fever (children: 16%; adults: 1% to 2%)
1% to 10%:
Cardiovascular: Bradycardia (<4%), bundle branch block (<4%), chest discomfort (<4%), chest pain (<4%), ECG changes (<4%), facial edema (<4%), first-degree atrioventricular block (<4%), hypotension (<4%), orthostatic hypotension (<4%), palpitations (<4%), prolonged Q-T interval on ECG (<4%), tachycardia (adults: <4%), hypertension (≤3%), peripheral edema (≤3%), syncope (1% to 2%)
Central nervous system: Dystonia (2% to 6%), abnormal gait (4%), procedural pain (4%), pain (1% to 4%), disturbance in attention (≤4%), agitation (<4%), ataxia (<4%), depression (<4%), dysarthria (<4%), falling (<4%), lethargy (<4%), malaise (<4%), nervousness (<4%), orthostatic dizziness (<4%), paresthesia (<4%), seizure (<4%), sleep disturbance (<4%), tardive dyskinesia (<4%), vertigo (<4%), hypoesthesia (≤2%)
Dermatologic: Skin rash (≤8%), eczema (<4%), pruritus (<4%), xeroderma (≤3%), acne vulgaris (≤2%)
Endocrine & metabolic: Decrease in HDL cholesterol (10%), increased thirst (children: ≤7%), increased serum cholesterol (4% to 6%), amenorrhea (4%), weight loss (≤4%), decreased libido (<4%), delayed ejaculation (<4%), galactorrhea not associated with childbirth (<4%), glycosuria (<4%), gynecomastia (<4%), hyperglycemia (<4%), increased gamma-glutamyl transferase (<4%), infrequent uterine bleeding (<4%), menstrual disease (<4%), increased serum triglycerides (3%)
Gastrointestinal: Xerostomia (≤10%), dyspepsia (3% to 10%), sialorrhea (1% to 10%), diarrhea (≤8%), decreased appetite (≤6%), stomach discomfort (<6%), abdominal pain (adults: <4%), anorexia (<4%), gastritis (<4%), gastroenteritis (<4%), abdominal distress (1% to 3%), toothache (≤3%)
Genitourinary: Menstruation (≤4%; delayed), cystitis (<4%), erectile dysfunction (<4%), irregular menses (<4%), mastalgia (<4%), sexual disorder (<4%), urinary tract infection (<4%)
Hematologic & oncologic: Anemia (<4%), neutropenia (<4%)
Hepatic: Increased liver enzymes (<4%), increased serum alanine aminotransferase (<4%), increased serum aspartate aminotransferase (<4%)
Hypersensitivity: Hypersensitivity reaction (<4%)
Infection: Abscess at injection site (<4%), infection (<4%), influenza (<4%), localized infection (<4%), viral infection (<4%)
Local: Induration at injection site (<4%), injection site reaction (<4%), local pain (buttock: <4%), pain at injection site (<4%), swelling at injection site (<4%)
Neuromuscular & skeletal: Limb pain (≤8%), back pain (≤7%), dyskinesia (adults: ≤6%), musculoskeletal pain (5%), arthralgia (2% to 4%), abnormal posture (<4%), akinesia (<4%), hypokinesia (<4%), musculoskeletal chest pain (<4%), myalgia (<4%), myasthenia (<4%), neck pain (<4%), muscle spasm (3%), muscle rigidity (≤3%), asthenia (1% to 2%), increased creatine phosphokinase (≤2%)
Ophthalmic: Blurred vision (2% to 7%), conjunctivitis (<4%), decreased visual acuity (<4%)
Otic: Otalgia (≤4%), otic infection (<4%)
Respiratory: Nasal congestion (≤10%), pharyngolaryngeal pain (3% to 10%), rhinitis (≤9%), respiratory tract infection (≤8%), bronchitis (<4%), dyspnea (<4%), flu-like symptoms (<4%), pharyngitis (<4%), pneumonia (<4%), sinusitis (<4%), epistaxis (≤2%), paranasal sinus congestion (≤2%)
<1%, postmarketing, and/or case reports: Abnormal eye movements (eye rolling), agranulocytosis, alopecia, anaphylaxis, angioedema, anorgasmia, aspiration pneumonia, atrial fibrillation, blepharospasm, blunted affect, breast engorgement, breast hypertrophy, breast secretion, breast tenderness, bronchopneumonia, bruxism, cellulitis, cerebral ischemia, cerebrovascular accident, cerebrovascular disease, cheilitis, chills, cogwheel rigidity, cold extremities, coma, confusion, crusting of eyelid, cutaneous nodule, cyst, dermal ulcer, dermatitis (acarodermatitis), dermatologic disorders, diabetes mellitus, diabetic coma, diabetic ketoacidosis, disruption of body temperature regulation, drug-induced hypersensitivity, drug withdrawal, dry eye syndrome, dysgeusia, dysphagia, dysuria, edema, eosinophilia, erythema, esophageal motility disorder, eye discharge, eye infection, eyelid edema, fecal incontinence, fecaloma, feeling abnormal, flushing, glaucoma, granulocytopenia, hematoma, hyperkeratosis, hyperthermia, hypertonia, hypertriglyceridemia, hyperventilation, hypoglycemia, hypomenorrhea, hypothermia, impaired consciousness, increased serum transaminases, intestinal obstruction, jaundice, joint stiffness, joint swelling, lacrimation, leukopenia, lip edema, loss of balance, lower respiratory tract infection, maculopapular rash, mania, mask-like face, movement disorder, muscle twitching, nasal mucosa swelling, neuroleptic malignant syndrome, night sweats, ocular hyperemia, onychomycosis, oral hypoesthesia, oromandibular dystonia, otitis media (including chronic), pancreatitis, papular rash, photophobia, pitting edema, pituitary neoplasm, pollakiuria, polydipsia, precocious puberty, priapism, pulmonary congestion, pulmonary embolism, rales, respiratory congestion, respiratory distress, restlessness, retinal artery occlusion, retrograde ejaculation, rhabdomyolysis seborrheic dermatitis of scalp, SIADH, skin discoloration, skin lesion, sleep apnea, somnambulism, speech disturbance, swelling of eye, thrombocytopenia, thrombotic thrombocytopenic purpura, tinnitus, tissue necrosis, tongue paralysis, tongue spasm, tonsillitis, torticollis, tracheobronchitis, transient ischemic attacks, trismus, unresponsive to stimuli, urinary retention, vaginal discharge, ventricular tachycardia, visual disturbance, voice disorder, water intoxication, wheezing
Warnings/Precautions
Concerns related to adverse effects:
- Altered cardiac conduction: May alter cardiac conduction and prolong the QT interval; life-threatening arrhythmias have occurred with therapeutic doses of antipsychotics (Haddad 2002; Ray 2009). Risk may be increased by conditions or concomitant medications which cause bradycardia, hypokalemia, and/or hypomagnesemia. Use caution in patients with a history of conduction abnormalities. Relative to other neuroleptics, risperidone has a low risk of arrhythmias (APA [Lehman 2004]).
- Anticholinergic effects: May cause anticholinergic effects (confusion, agitation, constipation, xerostomia, blurred vision, urinary retention); use with caution in patients with decreased gastrointestinal motility, urinary retention, BPH, xerostomia, or visual problems. Relative to other neuroleptics, risperidone has a low potency of cholinergic blockade (Richelson 1999).
- Antiemetic effects: May mask toxicity of other drugs or conditions (eg, intestinal obstruction, Reyes syndrome, brain tumor) due to antiemetic effects.
- Blood dyscrasias: Leukopenia, neutropenia, and agranulocytosis (sometimes fatal) have been reported in clinical trials and postmarketing reports with antipsychotic use; presence of risk factors (eg, pre-existing low WBC or history of drug-induced leuko-/neutropenia) should prompt periodic blood count assessment. Discontinue therapy at first signs of blood dyscrasias or if absolute neutrophil count <1,000/mm3.
- Cerebrovascular effects: An increased incidence of cerebrovascular effects (eg, transient ischemic attack, stroke), including fatalities, has been reported in placebo-controlled trials of risperidone for the unapproved use in elderly patients with dementia-related psychosis.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving). May be low to moderately sedating in comparison with other antipsychotics (Richelson 1999); dose-related effects have been observed.
- Dyslipidemia: Has been reported with atypical antipsychotics; risk profile may differ between agents. Compared to other antipsychotics, the risk of metabolic side effects (including dyslipidemia) with risperidone is low (Solmi 2017).
- Esophageal dysmotility/Aspiration: Antipsychotic use has been associated with esophageal dysmotility and aspiration; risk increases with age. Use with caution in patients at risk for aspiration pneumonia (eg, Alzheimer disease), particularly in patients >75 years of age (Herzig 2017; Maddalena 2004).
- Extrapyramidal symptoms: May cause extrapyramidal symptoms (EPS), including pseudoparkinsonism, acute dystonic reactions, akathisia, and tardive dyskinesia (risk of these reactions is generally much lower relative to typical/conventional antipsychotics; frequencies reported are similar to placebo). Risk of dystonia (and possibly other EPS) may be greater with increased doses, use of conventional antipsychotics, males, and younger patients. Factors associated with greater vulnerability to tardive dyskinesia include older in age, female gender combined with postmenopausal status, Parkinson disease, pseudoparkinsonism symptoms, affective disorders (particularly major depressive disorder), concurrent medical diseases such as diabetes, previous brain damage, alcoholism, poor treatment response, and use of high doses of antipsychotics (APA [Lehman 2004]; Soares-Weiser 2007). Consider therapy discontinuation with signs/symptoms of tardive dyskinesia.
- Falls: May increase the risk for falls due to somnolence, orthostatic hypotension, and motor or sensory instability. Complete fall risk assessments at baseline and periodically during treatment in patients with diseases or on medications that may also increase fall risk.
- Hyperglycemia: Atypical antipsychotics have been associated with development of hyperglycemia; in some cases, may be extreme and associated with ketoacidosis, hyperosmolar coma, or death. Use with caution in patients with diabetes or other disorders of glucose regulation; monitor for worsening of glucose control. Compared to other antipsychotics, the risk of metabolic side effects (including hyperglycemia) with risperidone is low (Solmi 2017).
- Hyperprolactinemia: Risperidone is associated with greater increases in prolactin levels as compared to other antipsychotic agents; clinical significance of hyperprolactinemia in patients with breast cancer or other prolactin-dependent tumors is unknown. Risk factors for hyperprolactinemia in patients taking risperidone include female gender, younger age at onset of illness, and higher scores on the Positive and Negative Symptom Scale (PANSS). Additionally, higher doses are associated with greater elevations in prolactin concentrations (Bo 2016).
- Hypersensitivity: Hypersensitivity reactions including anaphylactic reactions and angioedema have been reported.
- Intraoperative floppy iris syndrome: Few case reports describe intraoperative floppy iris syndrome (IFIS) in patients receiving risperidone and undergoing cataract surgery (Ford 2011). Prior to cataract surgery, evaluate for prior or current risperidone use. The benefits or risks of interrupting risperidone prior to surgery have not been established; clinicians are advised to proceed with surgery cautiously.
- Neuroleptic malignant syndrome: Use may be associated with neuroleptic malignant syndrome (NMS); monitor for mental status changes, fever, muscle rigidity, and/or autonomic instability.
- Orthostatic hypotension: May cause orthostatic hypotension; use with caution in patients at risk of this effect (eg, concurrent medication use which may predispose to hypotension/bradycardia or presence of hypovolemia) or in those who would not tolerate transient hypotensive episodes. Use caution with history of cerebrovascular or cardiovascular disease (MI, heart failure, or ischemic disease).
- Priapism: Rare cases of priapism have been reported.
- Suicidal ideation: The possibility of a suicide attempt is inherent in psychotic illness or bipolar disorder; use with caution in high-risk patients during initiation of therapy. Prescriptions should be written for the smallest quantity consistent with good patient care.
- Temperature regulation: Impaired core body temperature regulation may occur; caution with strenuous exercise, heat exposure, dehydration, and concomitant medication possessing anticholinergic effects (Kwok 2005, Martinez 2002).
- Weight gain: Significant weight gain has been observed with antipsychotic therapy; incidence varies with product. Compared to other antipsychotics, the risk of weight gain with risperidone is moderate (Solmi 2017). Monitor waist circumference and BMI.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with severe cardiac disease, hemodynamic instability, prior myocardial infarction or ischemic heart disease.
- Dementia: [US Boxed Warning]: Elderly patients with dementia-related psychosis treated with antipsychotics are at an increased risk of death compared to placebo. Most deaths appeared to be either cardiovascular (eg, heart failure, sudden death) or infectious (eg, pneumonia) in nature. Use with caution in patients with Lewy body dementia or Parkinson disease dementia due to greater risk of adverse effects, increased sensitivity to extrapyramidal effects, and association with irreversible cognitive decompensation or death. (APA [Reus 2016]). Risperidone is not approved for the treatment of dementia-related psychosis. Careful assessment of risk factors for stroke or existing cardiovascular morbidities is required prior to initiation.
- Hepatic impairment: Use with caution in patients with hepatic disease or impairment; dosage reduction is recommended.
- Renal impairment: Use with caution in patients with renal disease; dosage reduction is recommended.
- Seizures: Use with caution in patients at risk of seizures, including those with a history of seizures, head trauma, brain damage, alcoholism, or concurrent therapy with medications which may lower seizure threshold.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer’s labeling.
- Dispersible tablet: Inform patients with phenylketonuria that dispersible tablets contain phenylalanine.
- SubQ injection site reactions: Following each SubQ injection, a lump may develop and persist for several weeks; it will decrease in size over time. Do not rub or massage the injection site.
Other warnings/precautions:
- Discontinuation of therapy: When discontinuing antipsychotic therapy, the American Psychiatric Association (APA), Canadian Psychiatric Association (CPA), and World Federation of Societies of Biological Psychiatry (WFSBP) guidelines recommend gradually tapering antipsychotics to avoid physical withdrawal symptoms, including anorexia, anxiety, diaphoresis, diarrhea, dizziness, dyskinesia, headache, myalgia, nausea, paresthesia, restlessness, tremulousness, and vomiting (APA [Lehman 2004]; CPA [Addington 2005]; Lambert 2007; WFSBP [Hasan 2012]). The risk of withdrawal symptoms is highest following abrupt discontinuation of highly anti-cholinergic or dopaminergic antipsychotics (Cerovecki 2013). Additional factors such as duration of antipsychotic exposure, the indication for use, medication half-life, and risk for relapse should be considered. In schizophrenia, there is no reliable indicator to differentiate the minority who will not from the majority who will relapse with drug discontinuation. However, studies in which the medication of well-stabilized patients were discontinued indicate that 75% of patients relapse within 6 to 24 months. Indefinite maintenance antipsychotic medication is generally recommended, and especially for patients who have had multiple prior episodes or 2 episodes within 5 years (APA [Lehman 2004]).
Monitoring Parameters
Mental status; vital signs (as clinically indicated); blood pressure (baseline; repeat 3 months after antipsychotic initiation, then yearly); weight, height, BMI, waist circumference (baseline; repeat at 4, 8, and 12 weeks after initiating or changing therapy, then quarterly; consider switching to a different antipsychotic for a weight gain ≥5% of initial weight); CBC (as clinically indicated; monitor frequently during the first few months of therapy in patients with pre-existing low WBC or history of drug-induced leukopenia/neutropenia); electrolytes, renal and liver function (annually and as clinically indicated); personal and family history of obesity, diabetes, dyslipidemia, hypertension, or cardiovascular disease (baseline; repeat annually); fasting plasma glucose level/HbA1c (baseline; repeat 3 months after starting antipsychotic, then yearly); fasting lipid panel (baseline; repeat 3 months after initiation of antipsychotic; if LDL level is normal repeat at 2 to 5 year intervals or more frequently if clinical indicated); changes in menstruation, libido, development of galactorrhea, erectile and ejaculatory function (at each visit for the first 12 weeks after the antipsychotic is initiated or until the dose is stable, then yearly); abnormal involuntary movements or parkinsonian signs (baseline; repeat weekly until dose stabilized for at least 2 weeks after introduction and for 2 weeks after any significant dose increase); tardive dyskinesia (every 12 months; high-risk patients every 6 months); ocular examination (yearly in patients >40 years; every 2 years in younger patients) (ADA 2004; Lehman 2004; Marder 2004).
Pregnancy
Pregnancy Considerations
Risperidone and its metabolite cross the placenta (Newport 2007). Agenesis of the corpus callosum has been noted in one case report of an infant exposed to risperidone in utero; relationship to risperidone exposure is not known. Antipsychotic use during the third trimester of pregnancy has a risk for extrapyramidal symptoms (EPS) and/or withdrawal symptoms in newborns following delivery. Symptoms in the newborn may include agitation, feeding disorder, hypertonia, hypotonia, respiratory distress, somnolence, and tremor. These effects may be self-limiting and allow recovery within hours or days with no specific treatment, or they may be severe requiring prolonged hospitalization.
When using the IM injection, patients should notify health care provider if they become or intend to become pregnant during therapy or within 12 weeks of last injection.
The ACOG recommends that therapy during pregnancy be individualized; treatment with psychiatric medications during pregnancy should incorporate the clinical expertise of the mental health clinician, obstetrician, primary health care provider, and pediatrician. Safety data related to atypical antipsychotics during pregnancy is limited. As a result, routine use is not recommended. However, if a woman is inadvertently exposed to an atypical antipsychotic while pregnant, continuing therapy may be preferable to switching to an agent that the fetus has not yet been exposed to; consider risk:benefit (ACOG 2008). If treatment is needed in a woman planning a pregnancy or if treatment is initiated during pregnancy, use of an agent other than risperidone is preferred (Larsen 2015).
Risperidone may cause hyperprolactinemia, which may cause a reversible decrease in reproductive function in females.
Health care providers are encouraged to enroll women 18 to 45 years of age exposed to risperidone during pregnancy in the Atypical Antipsychotics Pregnancy Registry (1-866-961-2388 or http://www.womensmentalhealth.org/pregnancyregistry).
Patient Education
What is this drug used for?
- It is used to treat schizophrenia.
- It is used to treat bipolar problems.
- It is used to treat irritation that happens with autistic disorder.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Weight gain
- Injection site lump
- Back pain
- Muscle pain
- Agitation
- Fatigue
- Anxiety
- Nausea
- Vomiting
- Abdominal pain
- Heartburn
- Diarrhea
- Constipation
- Dry mouth
- Increased hunger
- Loss of strength and energy
- Stuffy nose
- Runny nose
- Sore throat
- Headache
- Trouble sleeping
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- High blood sugar like confusion, feeling sleepy, more thirst, hunger, passing urine more often, flushing, fast breathing, or breath that smells like fruit.
- Severe dizziness
- Passing out
- Behavioral changes
- Mood changes
- Tremors
- Abnormal movements
- Rigidity
- Unable to pass urine
- Change in amount of urine passed
- Difficulty swallowing
- Difficulty speaking
- Difficulty focusing
- Seizures
- Vision changes
- Shortness of breath
- Drooling
- Enlarged breasts
- Sexual dysfunction
- Decreased sex drive
- Nipple discharge
- No menstrual periods
- Erection that lasts more than 4 hours
- Neuroleptic malignant syndrome like fever, muscle cramps or stiffness, dizziness, very bad headache, confusion, change in thinking, fast heartbeat, abnormal heartbeat, or sweating a lot.
- Tardive dyskinesia like unable to control body movements; tongue, face, mouth, or jaw sticking out; mouth puckering; and puffing cheeks.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.