Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Suspension, Oral:
Banzel: 40 mg/mL (460 mL) [contains methylparaben, propylene glycol, propylparaben; orange flavor]
Tablet, Oral:
Banzel: 200 mg, 400 mg [scored; contains corn starch]
Pharmacology
Mechanism of Action
A triazole-derivative antiepileptic whose exact mechanism is unknown. In vitro, it prolongs the inactive state of the sodium channels, thereby limiting repetitive firing of sodium-dependent action potentials mediating anticonvulsant effects.
Pharmacokinetics/Pharmacodynamics
Absorption
Slow; extensive ≥85%; increased with food
Distribution
Vd: ~50 L
Metabolism
Extensively via carboxylesterase-mediated hydrolysis of the carboxylamide group to CGP 47292 (inactive metabolite); weak inhibitor of CYP2E1 and weak inducer of CYP3A4
Excretion
Urine (85%, ~66% as CGP 47292, 2% as unchanged drug)
Time to Peak
4 to 6 hours
Half-Life Elimination
~6 to 10 hours
Protein Binding
34%, primarily to albumin (27%)
Use in Specific Populations
Special Populations: Renal Function Impairment
Patients undergoing dialysis 3 hours postdosing displayed a decrease in AUC and Cmax of 29% and 16%, respectively.
Special Populations: Gender
Population pharmacokinetic analyses of women show a 6% to 14% lower apparent Cl of rufinamide compared with men.
Use: Labeled Indications
Lennox-Gastaut syndrome: Adjunctive treatment of seizures associated with Lennox-Gastaut syndrome in adults and children 1 year and older
Contraindications
Patients with familial short QT syndrome
Canadian labeling: Additional contraindications (not in US labeling): Family history of short QT syndrome; presence or history of short QT interval; hypersensitivity to rufinamide, triazole derivatives, or any component of the formulation
Dosage and Administration
Dosing: Adult
Lennox-Gastaut syndrome (adjunctive): Oral: 400 to 800 mg daily in 2 equally divided doses; increase dose by 400 to 800 mg daily every other day to a maximum dose of 3,200 mg daily in 2 equally divided doses
Note: Discontinue therapy gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal. Reducing dose by approximately 25% every 2 days was effective in trials.
Dosage adjustment for concomitant medications: Valproate: Initial rufinamide dose should be <400 mg/day
Dosing: Geriatric
Refer to adult dosing. Initiate at the low end of the dosing range; use with caution.
Dosing: Pediatric
Lennox-Gastaut syndrome (adjunctive):
Children and Adolescents <17 years: Oral: Initial: 10 mg/kg/day in 2 equally divided doses; increase dose by ~10 mg/kg increments every other day to a target daily dose of 45 mg/kg/day in 2 equally divided doses; maximum daily dose: 3,200 mg/day; effectiveness of doses lower than the target dose is unknown
Adolescents ≥17 years: Oral: Initial: 400 to 800 mg/day in 2 equally divided doses; increase dose by 400 to 800 mg daily every other day to a maximum daily dose of 3,200 mg/day in 2 equally divided doses; effectiveness of doses lower than 3,200 mg/day is unknown
Discontinuation of therapy: Children and Adolescents: Discontinue therapy gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal. Reducing dose by approximately 25% every 2 days was effective in trials.
Dosing adjustment for concomitant valproate: Children and Adolescents: Oral: Initial rufinamide dose should be <10 mg/kg/day (pediatric patients <17 years) or <400 mg/day (adolescents ≥17 years)
Extemporaneously Prepared
A 40 mg/mL oral suspension may be made using tablets. Crush twelve 400 mg tablets (or twenty-four 200 mg tablets) and reduce to a fine powder. Add 60 mL of Ora-Plus® in incremental proportions until a smooth suspension is obtained; then mix well while adding 60 mL of Ora-Sweet® or Ora-Sweet® SF; transfer to a calibrated bottle. Label "shake well". Stable 90 days at room temperature.
Hutchinson DJ, Liou Y, Best R, et al, "Stability of Extemporaneously Prepared Rufinamide Oral Suspensions," Ann Pharmacother, 2010, 44(3):462-5.20150505
Administration
Oral: Administer with food. Tablets may be swallowed whole, split in half, or crushed. Oral suspension should be administered using the provided adapter and calibrated oral syringe; shake well before each dose.
Dietary Considerations
Take with food.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect tablets from moisture. Discard oral suspension within 90 days after opening; cap of bottle fits over the adapter.
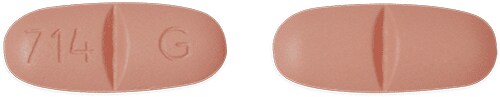
Rufinamide Images
Drug Interactions
Alcohol (Ethyl): May enhance the adverse/toxic effect of Rufinamide. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
CarBAMazepine: Rufinamide may decrease the serum concentration of CarBAMazepine. CarBAMazepine may decrease the serum concentration of Rufinamide. Monitor therapy
CloZAPine: CYP3A4 Inducers (Weak) may decrease the serum concentration of CloZAPine. Monitor therapy
CNS Depressants: Rufinamide may enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Ethinyl Estradiol: Rufinamide may decrease the serum concentration of Ethinyl Estradiol. Consider therapy modification
Fosphenytoin: May decrease the serum concentration of Rufinamide. Rufinamide may increase the serum concentration of Fosphenytoin. Monitor therapy
Lacosamide: Antiepileptic Agents (Sodium Channel Blockers) may enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
NiMODipine: CYP3A4 Inducers (Weak) may decrease the serum concentration of NiMODipine. Monitor therapy
Norethindrone: Rufinamide may decrease the serum concentration of Norethindrone. Consider therapy modification
PHENobarbital: Rufinamide may increase the serum concentration of PHENobarbital. PHENobarbital may decrease the serum concentration of Rufinamide. Monitor therapy
Phenytoin: Rufinamide may increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Rufinamide. Monitor therapy
Primidone: May decrease the serum concentration of Rufinamide. Monitor therapy
Ubrogepant: CYP3A4 Inducers (Weak) may decrease the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 100 mg and second dose (if needed) of 100 mg when used with a weak CYP3A4 inducer. Consider therapy modification
Valproate Products: May increase the serum concentration of Rufinamide. Management: Initiate rufinamide at a dose less than 10 mg/kg/day (children) or 400 mg/day (adults) in patients receiving valproic acid. In patients receiving rufinamide, initiate valproic acid at a low dose and titrate based on clinical response. Consider therapy modification
Adverse Reactions
>10%:
Cardiovascular: Shortened QT interval (46% to 65%; dose related)
Central nervous system: Headache (adults 27%, children 16%), drowsiness (11% to 24%), dizziness (3% to 19%), fatigue (9% to 16%)
Gastrointestinal: Vomiting (children 17%, adults 5%), nausea (7% to 12%)
1% to 10%:
Central nervous system: Ataxia (4% to 5%), status epilepticus (≤4%), aggressive behavior (children 3%), anxiety (adults 3%), disturbance in attention (children 3%), hyperactivity (children 3%), vertigo (adults 3%), abnormal gait (1% to 3%), convulsions (children 2%)
Dermatologic: Skin rash (children 4%), pruritus (children 3%)
Gastrointestinal: Decreased appetite (children 5%), constipation (adults 3%), dyspepsia (adults 3%), upper abdominal pain (3%), increased appetite (≥1%)
Hematologic & oncologic: Leukopenia (4%), anemia (1%)
Infection: Influenza (children 5%)
Neuromuscular & skeletal: Tremor (adults 6%), back pain (adults 3%)
Ophthalmic: Diplopia (4% to 9%), blurred vision (adults 6%), nystagmus (adults 6%)
Otic: Otic infection (children 3%), pollakiuria (1%)
Respiratory: Nasopharyngitis (children 5%), bronchitis (children 3%), sinusitis (children 3%)
<1%, postmarketing, and/or case reports: Atrioventricular block (first degree), bundle branch block (right), dysuria, hematuria, hypersensitivity (multiorgan), iron-deficiency anemia, lymphadenopathy, nephrolithiasis, neutropenia, nocturia, polyuria, Stevens-Johnson syndrome, suicidal ideation, thrombocytopenia, urinary incontinence
Warnings/Precautions
Concerns related to adverse effects:
- Altered cardiac conduction: Has been associated with shortening of the QT interval. Use caution in patients receiving concurrent medications that shorten the QT interval. Contraindicated in patients with familial short-QT syndrome.
- CNS effects: Use has been associated with CNS-related adverse events, most significant of these were cognitive symptoms (including somnolence or fatigue) and coordination abnormalities (including ataxia, dizziness, and gait disturbances). Caution patients about performing tasks that require mental alertness (eg, operating machinery or driving).
- Multiorgan hypersensitivity reactions: Potentially serious, sometimes fatal, multiorgan hypersensitivity reactions (also known as drug reaction with eosinophilia and systemic symptoms [DRESS]) have been reported. Monitor for signs and symptoms (eg, fever, rash, lymphadenopathy, eosinophilia) in association with other organ system involvement (eg, hepatitis, nephritis, hematological abnormalities, myocarditis, myositis). Evaluate immediately if signs or symptoms are present. Discontinuation and conversion to alternate therapy may be required.
- Dermatologic reactions: Potentially serious, sometimes fatal, dermatologic reactions including Stevens-Johnson syndrome (SJS) have been reported; monitor for signs and symptoms of skin reactions; discontinuation and conversion to alternate therapy may be required.
- Leukopenia: Decreased white blood cell count has been reported during treatment.
- Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; notify health care provider immediately if symptoms occur.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with mild to moderate impairment; use in not recommended in patients with severe impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP 1997; Zar 2007).
Other warnings/precautions:
- Withdrawal: Anticonvulsants should not be discontinued abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal. Reducing dose by ~25% every two days was effective in trials.
Monitoring Parameters
Seizure (frequency and duration); serum levels of concurrent anticonvulsants; suicidality (eg, suicidal thoughts, depression, behavioral changes); rash (may indicate multi-organ hypersensitivity reactions)
Pregnancy
Pregnancy Considerations
Adverse effects were seen in animal reproduction studies. Some hormonal contraceptives may be less effective with concurrent rufinamide use; additional forms of nonhormonal contraceptives should be used.
Patients exposed to rufinamide during pregnancy are encouraged to enroll themselves into the AED Pregnancy Registry by calling 1-888-233-2334. Additional information is available at www.aedpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used to help control certain kinds of seizures.
Frequently reported side effects of this drug
- Fatigue
- Headache
- Dizziness
- Flu-like symptoms
- Stuffy nose
- Sore throat
- Lack of appetite
- Vomiting
- Nausea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion
- Shortness of breath
- Excessive weight gain
- Swelling of arms or legs
- Infection
- Severe loss of strength and energy
- Bruising
- Bleeding
- Severe muscle pain
- Severe muscle weakness
- Swollen glands
- Chest pain
- Unable to pass urine
- Change in amount of urine passed
- Change in balance
- Abnormal gait
- Tremors
- Vision changes
- Involuntary eye movements
- Seizures
- Agitation
- Panic attacks
- Mood changes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.