Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
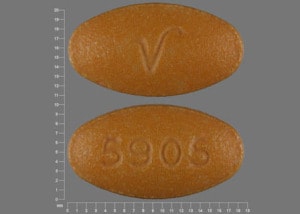
Tablet, Oral:
Azulfidine: 500 mg [scored]
Generic: 500 mg
Tablet Delayed Release, Oral:
Azulfidine EN-tabs: 500 mg
Generic: 500 mg
Pharmacology
Mechanism of Action
5-aminosalicylic acid (5-ASA) is the active component of sulfasalazine; the specific mechanism of action of 5-ASA is unknown; however, it is thought that it modulates local chemical mediators of the inflammatory response, especially leukotrienes, and is also postulated to be a free radical scavenger or an inhibitor of tumor necrosis factor (TNF); action appears topical rather than systemic
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Sulfasalazine: <15% as parent drug
Distribution
Vd: Sulfasalazine: 7.5 ± 1.6 L
Metabolism
Via colonic intestinal flora to sulfapyridine and 5-aminosalicylic acid (5-ASA). Following absorption, sulfapyridine undergoes acetylation to form AcSP and ring hydroxylation while 5-ASA undergoes N-acetylation (non-acetylation phenotype dependent process); rate of metabolism via acetylation dependent on acetylation phenotype
Excretion
Primarily urine (as unchanged drug, conjugates, and acetylated metabolites); feces (small amounts)
Onset of Action
Rheumatoid arthritis: >4 weeks; Ulcerative colitis: >3 to 4 weeks
Time to Peak
Sulfasalazine: 3 to 12 hours (mean: 6 hours); Sulfapyridine and 5-aminosalicylic acid (5-ASA) : ~10 hours
Half-Life Elimination
Sulfasalazine: 7.6 ± 3.4 hours (prolonged in elderly patients); Sulfapyridine: 14.8 hours (slow acetylators) and 10.4 hours (fast acetylators)
Protein Binding
Sulfasalazine: >99% to albumin; Sulfapyridine: ~70% to albumin; Acetylsulfapyridine (AcSP): ~90% to plasma proteins
Use in Specific Populations
Special Populations: Elderly
Elderly patients with rheumatoid arthritis showed a prolonged plasma half-life for sulfasalazine, sulfapyridine, and their metabolites.
Special Populations Note
Acetylator status: SP metabolism is mediated by polymorphic enzymes such that 2 distinct populations of slow and fast metabolizer exist. Slow acetylator phenotype (~60% of white patients) display a prolonged plasma half-life and an accumulation of higher plasma levels of SP than fast acetylators.
Use: Labeled Indications
Juvenile rheumatoid arthritis: Delayed release: Treatment of pediatric patients with polyarticular-course juvenile rheumatoid arthritis who have responded inadequately to salicylates or other NSAIDs.
Rheumatoid arthritis: Delayed release: Treatment of rheumatoid arthritis in patients who have responded inadequately to salicylates or other NSAIDs. Note: Treatment initiation with a DMARD is recommended in DMARD-naive patients with either early rheumatoid arthritis (RA) (disease duration <6 months) or established RA (disease duration ≥6 months) (Singh [ACR 2016]).
Ulcerative colitis: Immediate and delayed release: Treatment of mild to moderate ulcerative colitis; adjunctive therapy in severe ulcerative colitis; prolongation of the remission period between acute attacks of ulcerative colitis.
Use: Off Label
Ankylosing spondylitisyes
The American College of Rheumatology recommends the use of sulfasalazine in patients with active ankylosing spondylitis disease despite treatment with NSAIDs and who have contraindications to anti-TNF agents Ward 2016.
Crohn disease (mild to moderately active)byes
Data from a systematic review of randomized, controlled trials evaluating sulfasalazine or mesalamine efficacy (compared with placebo) for the treatment of mild to moderately active Crohn disease supports the use of sulfasalazine in the management of this condition. Sulfasalazine demonstrates modest effectiveness with some benefit over placebo for induction of remission Lim 2016.
Based on the American College of Gastroenterology Management of Crohn's Disease in Adults guidelines, sulfasalazine given for mild to moderately active colonic and/or ileocolonic Crohn disease is effective in managing symptoms of this condition.
Psoriasisyes
According to the American Academy of Dermatology guidelines, methotrexate, cyclosporine, and acitretin are considered first-line systemic agents for psoriasis, but sulfasalazine may be an appropriate alternative for certain patients AAD [Menter 2009]. Sulfasalazine is contraindicated in patients with porphyria, urinary or intestinal obstruction, and hypersensitivity to sulfasalazine, its metabolites, sulfonamides, or salicylates.
Psoriatic arthritisyes
The Group for Research and Assessment of Psoriasis and Psoriatic Arthritis recommends the use of sulfasalazine in patients with peripheral arteritis (DMARD-naïve) or dactylitis psoriatic arthritis Coates 2016.
Contraindications
Hypersensitivity to sulfasalazine, its metabolites, sulfonamides, salicylates, or any component of the formulation; intestinal or urinary obstruction; porphyria
Note: Although the FDA-approved product labeling states this medication is contraindicated with other sulfonamide-containing drug classes, the scientific basis of this statement has been challenged. See "Warnings/Precautions" for more detail.
Canadian labeling: Additional contraindications (not in US labeling): Severe renal impairment (GFR <30 mL/minute/1.73 m2); severe hepatic impairment; use in pediatric patients <2 years of age; patients in whom acute asthmatic attacks, urticaria, rhinitis, or other allergic manifestations are precipitated by acetyl salicylic acid (ASA) or other NSAIDs
Dosage and Administration
Dosing: Adult
Rheumatoid arthritis: Oral: Delayed release: Initial: 500 mg once daily or 1 g/day in 2 divided doses; increase weekly to maintenance dose: 2 g/day in 2 divided doses; maximum: 3 g/day (if response to 2 g/day is inadequate after 12 weeks of treatment)
Ulcerative colitis: Oral: Immediate and delayed release:
Initial: 3 to 4 g/day in divided doses at ≤8-hour intervals; may initiate therapy with 1 to 2 g/day to reduce GI intolerance. Doses >4 g/day can increase the risk of toxicity.
Maintenance dose: 2 g/day in divided doses at ≤8-hour intervals when endoscopic exam confirms improvement
Dosage adjustment: If GI intolerance occurs, reduce dosage by 50% and gradually increase to target dose over several days. If GI intolerance persists, stop therapy for 5 to 7 days and reintroduce at a lower daily dose.
Ankylosing spondylitis (off-label use): Oral: Initial: 500 mg once daily; may increase up to 2 to 3 g/day in divided doses; if intolerance occurs, decrease dose by 500 mg each week as needed (Braun 2011; Clegg 1999; Dougados 1995).
Crohn disease (mild to moderately active) (off-label use): Oral: 3 to 6 g/day in divided doses for up to 16 weeks (Lichtenstein 2018; Sandborn 2007)
Psoriasis (off-label use): Oral: Initial: 500 mg twice daily; Maintenance: doses may be increased to 3 to 4 g/day as tolerated (Menter 2009).
Psoriatic arthritis (off-label use): Oral: Initial: 500 mg once daily; may increase up to 2 to 3 g daily in divided doses (Clegg 1996; Clegg 1999; Gupta 1995).
Desensitization regimen: For patients who may be sensitive to treatment, it is suggested to start with a total dose of 50 to 250 mg daily and double it every 4 to 7 days until the desired therapeutic level is achieved. Discontinue if symptoms of sensitivity occur. Do not attempt in patients with a history of agranulocytosis or those who have had a previous anaphylactoid reaction on sulfasalazine therapy
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Inflammatory bowel disease (eg, ulcerative colitis; Crohn disease):
Weight-directed dosing: Children and Adolescents:
Induction: Crohn disease, ulcerative colitis: Oral: 40 to 70 mg/kg/day in 3 to 6 divided doses; in some cases, higher induction doses up to 100 mg/kg/day may be required; maximum daily dose: 4,000 mg/day (ECCO/ESPGHAN [Turner 2018]; Rufo 2012; Sandhu 2010)
Maintenance: Ulcerative colitis: Oral: 30 to 70 mg/kg/day in 3 to 6 divided doses; maximum daily dose: 4,000 mg/day; effective induction dose should be transitioned as the initial maintenance dose; may consider dose reduction once remission sustained for several months (ECCO/ESPGHAN [Turner 2018]; Sandhu 2010)
Fixed dosing (Salazopyrin prescribing information [Canada] 2013): Children ≥25 kg and Adolescents: Note: Consider dose reduction or use of enteric-coated tablet in patients experiencing adverse gastrointestinal effects with uncoated tablet.
Acute attacks:
25 to <35 kg: Oral: 500 mg 3 times daily
35 to 50 kg: Oral: 1,000 mg 2 to 3 times daily
Maintenance of remission:
25 to <35 kg: Oral: 500 mg 2 times daily
35 to 50 kg: Oral: 500 mg 2 to 3 times daily
Juvenile idiopathic arthritis: Children and Adolescents 6 to 16 years: Oral: Enteric-coated tablet: 30 to 50 mg/kg/day in 2 divided doses; maximum daily dose: 2,000 mg/day (Beukelman 2011); Note: Although it is an FDA-labeled indication, the use of sulfasalazine for treatment of JIA is not included as a therapeutic option by experts (ACR [Ringold 2013])
Desensitization regimen: Children ≥6 years and Adolescents: For patients who may be sensitive to treatment, it is suggested to start with a lower total dose, for example when treating inflammatory bowel disease; lower initial doses of 50 to 250 mg daily is suggested (usual is 1,500 to 3,000 mg/day) and double it every 4 to 7 days until the desired dose is achieved. Discontinue if symptoms of sensitivity occur. Do not attempt in patients with a history of agranulocytosis or those who have had a previous anaphylactoid reaction on sulfasalazine therapy.
Extemporaneously Prepared
A 100 mg/mL oral suspension may be made with tablets. Place twenty 500 mg tablets in a mortar and add a small amount of a 1:1 mixture of Ora-Sweet® and Ora-Plus® to cover the tablets. Let soak for 20-30 minutes. Crush the tablets and mix to a uniform paste; mix while adding the vehicle in equal proportions to almost 100 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add sufficient quantity of vehicle to make 100 mL. Label "shake well". Stable 91 days under refrigeration or at room temperature.
Lingertat-Walsh K, Walker SE, Law S, et al, "Stability of Sulfasalazine Oral Suspension," Can J Hosp Pharm, 2006, 59(4):194-200.
Administration
Tablets should be administered in evenly divided doses, preferably after meals. Delayed-release tablets should be swallowed whole.
Dietary Considerations
Sulfasalazine impairs folate absorption. Adequate fluid intake is required to prevent crystalluria and stone formation.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
SulfaSALAzine Images
Drug Interactions
Cardiac Glycosides: 5-Aminosalicylic Acid Derivatives may decrease the serum concentration of Cardiac Glycosides. Monitor therapy
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Eltrombopag: May increase the serum concentration of BCRP/ABCG2 Substrates. Monitor therapy
Folic Acid: SulfaSALAzine may decrease the serum concentration of Folic Acid. Monitor therapy
Heparin: 5-Aminosalicylic Acid Derivatives may enhance the adverse/toxic effect of Heparin. Specifically, the risk for bleeding/bruising may be increased. Monitor therapy
Heparins (Low Molecular Weight): 5-Aminosalicylic Acid Derivatives may enhance the adverse/toxic effect of Heparins (Low Molecular Weight). Specifically, the risk for bleeding/bruising may be increased. Monitor therapy
Lasmiditan: May increase the serum concentration of BCRP/ABCG2 Substrates. Avoid combination
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Methotrexate: SulfaSALAzine may enhance the hepatotoxic effect of Methotrexate. Monitor therapy
Methylfolate: SulfaSALAzine may decrease the serum concentration of Methylfolate. Monitor therapy
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May enhance the nephrotoxic effect of 5-Aminosalicylic Acid Derivatives. Monitor therapy
Osimertinib: May increase the serum concentration of BCRP/ABCG2 Substrates. Monitor therapy
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Regorafenib: May increase the serum concentration of BCRP/ABCG2 Substrates. Monitor therapy
Riluzole: SulfaSALAzine may enhance the adverse/toxic effect of Riluzole. Specifically, the risk of hepatotoxicity may be increased. Management: Consider alternatives to sulfasalazine in patients receiving treatment with riluzole due to the potential for additive hepatotoxicity. Consider therapy modification
Rolapitant: May increase the serum concentration of BCRP/ABCG2 Substrates. Management: Monitor patients receiving rolapitant for increased exposure to and/or effects of BCRP/ABCG2 substrates. Use the lowest effective rosuvastatin dose when used in combination with rolapitant. Monitor therapy
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Tafamidis: May increase the serum concentration of BCRP/ABCG2 Substrates. Monitor therapy
Tedizolid: May increase the serum concentration of BCRP/ABCG2 Substrates. Monitor therapy
Teriflunomide: May increase the serum concentration of BCRP/ABCG2 Substrates. Monitor therapy
Thiopurine Analogs: 5-Aminosalicylic Acid Derivatives may decrease the metabolism of Thiopurine Analogs. Monitor therapy
Tolvaptan: May increase the serum concentration of BCRP/ABCG2 Substrates. Consider therapy modification
Varicella Virus-Containing Vaccines: 5-Aminosalicylic Acid Derivatives may enhance the adverse/toxic effect of Varicella Virus-Containing Vaccines. The primary concern is the potential development of Reye's Syndrome, a condition that has been associated with the use of salicylates in children with varicella infections. Consider therapy modification
Voxilaprevir: May increase the serum concentration of BCRP/ABCG2 Substrates. Avoid combination
Test Interactions
Reports of possible interference with measurements, by liquid chromatography, of urinary normetanephrine causing a false-positive test result have been observed in patients exposed to sulfasalazine or its metabolite, mesalamine/mesalazine.
Adverse Reactions
>10%:
Central nervous system: Headache (RA 9%)
Dermatologic: Skin rash (RA 13%)
Gastrointestinal: Nausea (RA 19%), dyspepsia (RA 13%), anorexia, gastric distress, vomiting
Genitourinary: Oligospermia (reversible)
1% to 10%:
Central nervous system: Dizziness
Dermatologic: Pruritus (RA 4%), urticaria
Gastrointestinal: Abdominal pain (RA 8%), stomatitis (RA 4%)
Hematologic & oncologic: Leukopenia (RA 3%), thrombocytopenia (RA 1%), Heinz body anemia, hemolytic anemia
Hepatic: Abnormal hepatic function tests (RA 4%)
Respiratory: Cyanosis
Miscellaneous: Fever
<1%, postmarketing, and/or case reports (includes reactions reported with mesalamine or other sulfonamides): Agranulocytosis, alopecia, anaphylaxis, angioedema, aplastic anemia, arthralgia, ataxia, cauda equina syndrome, cholestasis, cholestatic hepatitis, cholestatic jaundice, conjunctival injection, crystalluria, depression, diarrhea, DRESS syndrome, drowsiness, eosinophilia, exfoliative dermatitis, folate deficiency, fulminant hepatitis, Guillain-Barré syndrome, hallucination, hearing loss, hematologic abnormality, hematologic disease (pseudomononucleosis), hematuria, hemolytic-uremic syndrome, hepatic cirrhosis, hepatic failure, hepatic necrosis, hepatitis, hepatotoxicity (idiosyncratic) (Chalasani, 2014), hypoglycemia, hypoprothrombinemia, injected sclera, insomnia, interstitial nephritis, interstitial pulmonary disease, jaundice, Kawasaki syndrome (single case report), lupus-like syndrome, megaloblastic anemia, meningitis, methemoglobinemia, myelitis, myelodysplastic syndrome, myocarditis (allergic), nephritis, nephrolithiasis, nephrotic syndrome, neutropenia (congenital), neutropenic enterocolitis, oropharyngeal pain, pallor, pancreatitis, parapsoriasis varioliformis acuta, periarteritis nodosa, pericarditis, periorbital edema, peripheral neuropathy, pleurisy, pneumonia, pneumonitis, proteinuria, pulmonary alveolitis, purpura, renal disease (acute), rhabdomyolysis, seizure, sepsis, serum sickness-like reaction (children with JRA have frequent and severe reaction), skin discoloration, skin photosensitivity, Stevens-Johnson syndrome, thyroid function impairment, tinnitus, toxic epidermal necrolysis, toxic nephrosis, urinary tract infection, urine discoloration, vasculitis, vertigo
Warnings/Precautions
Concerns related to adverse effects:
- Blood dyscrasias: Fatalities associated with severe reactions, including agranulocytosis, aplastic anemia, and other blood dyscrasias, have occurred; discontinue use at first sign of rash or signs of serious adverse reactions. The presence of clinical signs such as sore throat, fever, pallor, or purpura may be indicative of a serious blood disorder. Use with extreme caution in patients with blood dyscrasias; monitor CBC frequently.
- CNS effects: Deaths from irreversible neuromuscular and CNS changes have been reported.
- Dermatologic reactions: Severe skin reactions (some fatal), including Stevens-Johnson syndrome (SJS), exfoliative dermatitis, and toxic epidermal necrolysis (TEN), have occurred with sulfonamides (including sulfasalazine), most commonly during the first month of treatment; discontinue use at first sign of skin rash, mucosal lesions, or any other sign of dermatologic toxicity.
- Fibrosing alveolitis: Deaths from fibrosing alveolitis have been reported.
- Folate deficiency: May decrease folic acid absorption.
- GI effects: Nausea, vomiting, and abdominal discomfort commonly occur; titration of dose and/or using the enteric coated formulation may decrease GI adverse effects.
- Hepatic necrosis: Fatalities associated with hepatic damage have occurred; discontinue use at first sign of jaundice or hepatotoxicity.
- Hypersensitivity reactions: Severe and life-threatening reactions, including drug rash with eosinophilia and systemic symptoms (DRESS) syndrome, have been reported. Fever or lymphadenopathy may be present prior to rash development. Other severe hypersensitivity reactions may include internal organ involvement, such as hepatitis, nephritis, myocarditis, mononucleosis-like syndrome, hematologic abnormalities (including hematophagic histiocytosis), and/or pneumonitis including eosinophilic infiltration. Discontinue treatment for severe reactions and evaluate promptly.
- Infections: Serious infections (some fatal), including sepsis and pneumonia, have been reported. Infections may be associated with agranulocytosis, neutropenia, or myelosuppression. Monitor for signs/symptoms of infection during and after sulfasalazine therapy and promptly evaluate if infection occurs; discontinue therapy for serious infections. Use cautiously in patients with a history of recurring or chronic infections or with underlying conditions or concomitant therapy which may predispose them to infectious complications.
- Oligospermia: In males, oligospermia (rare) and infertility have been reported; usually reverses upon discontinuation.
- Sulfonamide ("sulfa") allergy: Traditionally, concerns for cross-reactivity have extended to all compounds containing the sulfonamide structure (SO2NH2). An expanded understanding of allergic mechanisms indicates cross-reactivity between antibiotic sulfonamides and nonantibiotic sulfonamides may not occur, or at the very least this potential is extremely low (Brackett 2004; Johnson 2005; Slatore 2004; Tornero 2004). In particular, mechanisms of cross-reaction due to antibody production (anaphylaxis) are unlikely to occur with nonantibiotic sulfonamides and antibiotic sulfonamides. A nonantibiotic sulfonamide compound which contains the arylamine structure and therefore may cross-react with antibiotic sulfonamides is sulfasalazine (Zawodniak 2010). T-cell-mediated (type IV) reactions (eg, maculopapular rash) are less understood and it is not possible to completely exclude this potential based on current insights. In cases where prior reactions were severe (Stevens-Johnson syndrome/TEN), some clinicians choose to avoid exposure to these classes.
Disease-related concerns:
- Allergies/asthma: Use with caution in patients with severe allergies or bronchial asthma.
- G6PD deficiency: Use with caution in patients with G6PD deficiency; hemolytic anemia may occur (dose related).
- Hepatic impairment: Use with extreme caution in patients with impaired hepatic function.
- Renal impairment: Use with extreme caution in patients with renal impairment. Maintain adequate hydration to prevent crystalluria and stone formation.
Special populations:
- Slow acetylators: Patients classified as slow acetylators may be at increased risk for adverse reactions due to a prolonged half-life of sulfapyrazine (metabolite of sulfasalazine).
Dosage form specific issues:
- Appropriate use: Delayed release: Use in patients with ulcerative colitis who cannot take uncoated sulfasalazine tablets because of GI intolerance, and in whom there is evidence that this intolerance is not primarily the result of high blood levels of sulfapyridine and its metabolites (eg, patients experiencing nausea and vomiting with the first few doses of the drug, patients in whom a reduction in dosage does not alleviate the adverse GI effects).
- Enteric-coated tablets: Discontinue if tablets are noted to pass without disintegrating.
Other warnings/precautions:
- Skin/urine discoloration: May cause skin and urine discoloration (orange/yellow).
Monitoring Parameters
Manufacturer's labeling: CBC with differential and liver function tests (prior to therapy, then every other week for first 3 months of therapy, followed by every month for the second 3 months, then once every 3 months thereafter or as clinically indicated); periodic urinalysis and renal/liver function tests; stool frequency; signs of infection, dermatologic toxicity, or hypersensitivity reactions.
Alternate recommendations: Rheumatoid arthritis: Complete blood count, serum creatinine, and LFTs: Baseline and every 2 to 4 weeks for 3 months after initiation or following dose increases, then every 8 to 12 weeks during 3 to 6 months of treatment, followed by every 12 weeks beyond 6 months of treatment; monitor more frequently if clinically indicated (Singh [ACR 2016]).
Pregnancy
Pregnancy Considerations
Sulfasalazine and sulfapyridine cross the placenta.
Based on available data, an increase in fetal malformations has not been observed following maternal use of sulfasalazine for the treatment of inflammatory bowel disease. Cases of neural tube defects have been reported (causation undetermined). Agranulocytosis was noted in an infant following maternal use of sulfasalazine during pregnancy. Although sulfapyridine has poor bilirubin-displacing ability, a potential for kernicterus in the newborn exists.
Sulfasalazine is known to inhibit the absorption and metabolism of folic acid and may diminish the effects of folic acid supplementation. When treatment for inflammatory bowel disease is needed during pregnancy, sulfasalazine may be used, although supplementation with folic acid is recommended (Flint 2016; Huang 2014; Mahadevan 2015).
Sulfasalazine may cause oligospermia and reversible infertility in males (Habal 2012). Use is compatible in males with female partners of reproductive potential; however, discontinuing treatment for 3 months may enhance conception (Flint 2016).
Patient Education
What is this drug used for?
- It is used to treat rheumatoid arthritis and ulcerative colitis. It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Headache
- Abdominal pain
- Heartburn
- Nausea
- Vomiting
- Lack of appetite
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Severe loss of strength and energy
- Excessive weight gain
- Swelling of arms or legs
- Swollen glands
- Shortness of breath
- Bruising
- Bleeding
- Pale skin
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.