Boxed Warning
Weight reduction:
Drugs with thyroid hormone activity, alone or with other therapeutic agents, have been used for the treatment of obesity. In euthyroid patients, doses within the range of daily hormonal requirements are ineffective for weight reduction. Larger doses may produce serious or even life-threatening manifestations of toxicity, particularly when given in association with sympathomimetic amines such as those used for their anorectic effects.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Armour Thyroid: 15 mg, 30 mg, 60 mg, 90 mg, 120 mg
Armour Thyroid: 180 mg [scored]
Armour Thyroid: 240 mg
Armour Thyroid: 300 mg [scored]
Nature-Throid: 16.25 mg, 32.5 mg
Nature-Throid: 48.75 mg, 65 mg, 81.25 mg, 97.5 mg, 113.75 mg, 130 mg, 146.25 mg, 162.5 mg, 195 mg, 260 mg, 325 mg [scored]
NP Thyroid: 15 mg, 30 mg, 60 mg, 90 mg, 120 mg
Westhroid: 32.5 mg
Westhroid: 65 mg, 97.5 mg, 130 mg, 195 mg [scored]
WP Thyroid: 16.25 mg, 32.5 mg
WP Thyroid: 48.75 mg, 65 mg [scored]
WP Thyroid: 81.25 mg
WP Thyroid: 81.25 mg, 97.5 mg, 113.75 mg, 130 mg [scored]
Generic: 15 mg, 30 mg, 60 mg, 90 mg, 120 mg
Pharmacology
Mechanism of Action
The primary active compound is T3 (triiodothyronine), which may be converted from T4 (thyroxine) and then circulates throughout the body to influence growth and maturation of various tissues; exact mechanism of action is unknown; however, it is believed the thyroid hormone exerts its many metabolic effects through control of DNA transcription and protein synthesis; involved in normal metabolism, growth, and development; promotes gluconeogenesis, increases utilization and mobilization of glycogen stores and stimulates protein synthesis, increases basal metabolic rate
Pharmacokinetics/Pharmacodynamics
Absorption
Thyroxine (T4): 40% to 80%; T3: 95%; desiccated thyroid contains T4, T3, and iodine (primarily bound)
Metabolism
Hepatic to triiodothyronine (active); ~80% T4 deiodinated in kidney and periphery; glucuronidation/conjugation also occurs; undergoes enterohepatic recirculation
Excretion
Urine (major route of elimination); partially feces
Onset of Action
Liothyronine (T3): ~3 hours
Time to Peak
Serum: T4: 2 to 4 hours; T3: 2 to 3 days
Half-Life Elimination
T4: Euthyroid: 6 to 7 days; Hyperthyroid: 3 to 4 days; Hypothyroid: 9 to 10 days
T3: 0.75 days (Brent, 2011)
Protein Binding
T4: >99% bound to plasma proteins including thyroxine-binding globulin, thyroxine-binding prealbumin, and albumin
Use: Labeled Indications
Hypothyroidism: Replacement or supplemental therapy in hypothyroidism
Contraindications
Hypersensitivity to any component of the formulation; untreated thyrotoxicosis; uncorrected adrenal insufficiency
Dosage and Administration
Dosing: Adult
Note: The American Thyroid Association/American Association of Clinical Endocrinologists do not recommend the use of desiccated thyroid as replacement therapy for hypothyroidism (ATA [Jonklaas 2014]; ATA/AACE [Garber 2012]). Tablet strengths may vary by manufacturer in terms of grains or mg; dosing recommendations are based on general clinical equivalencies that 1 grain = 60 mg or 65 mg; 1/2 grain = 30 mg or 32.5 mg; and 1/4 grain = 15 mg or 16.25 mg.
Hypothyroidism: Oral: Initial: 30 or 32.5 mg/day; may increase dose in 15 or 16.25 mg increments every 2 to 3 weeks until adequate replacement dose determined; initiate with 15 or 16.25 mg/day in patients with cardiovascular disease or long-standing myxedema. Usual dosage range: 60 to 130 mg/day. Inadequate response to doses up to 195 mg/day suggests noncompliance or malabsorption.
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Dosing: Pediatric
Note: Doses presented as mg/kg/dose or mg/dose; closely review dosing units; adjust dose based upon clinical response and laboratory parameters. Tablet strengths may vary by manufacturer in terms of grains or mg; dosing recommendations are based on general clinical equivalencies that 1 grain = 60 mg or 65 mg; 1/2 grain = 30 mg or 32.5 mg; and 1/4 grain = 15 mg or 16.25 mg.
Congenital hypothyroidism: Note: Guidelines do not recommend routine use of desiccated thyroid over levothyroxine monotherapy in the management of hypothyroidism (AAP 2006; ATA [Jonklaas 2014]). Infants should have therapy initiated at full doses; Oral:
Infants 1 to 6 months: 4.8 to 6 mg/kg/dose or 15 to 32.5 mg/dose once daily
Infants >6 to 12 months: 3.6 to 4.8 mg/kg/dose or 30 to 48.75 mg/dose once daily
Children 1 to 5 years: 3 to 3.6 mg/kg/dose or 45 to 65 mg/dose once daily
Children 6 to 12 years: 2.4 to 3 mg/kg/dose or 60 to 97.5 mg/dose once daily
Adolescents: Typical doses 1.2 to 1.8 mg/kg/dose or >90 mg/dose once daily
Administration
Oral: Administer on an empty stomach (eg, 30 to 60 minutes prior to breakfast) to increase absorption.
Storage
Store at 15°C to 30°C (59°F to 86°F).
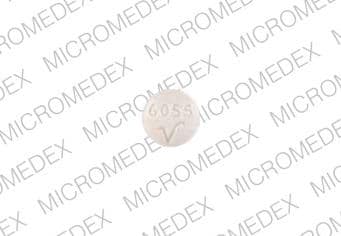
Thyroid, Desiccated Images
Drug Interactions
Amezinium: Thyroid Products may enhance the stimulatory effect of Amezinium. Monitor therapy
Amiodarone: May diminish the therapeutic effect of Thyroid Products. Monitor therapy
Apalutamide: May diminish the therapeutic effect of Thyroid Products. Monitor therapy
Bile Acid Sequestrants: May decrease the serum concentration of Thyroid Products. Management: Administer oral thyroid products at least 4 h prior to colesevelam, and at least 1 h before or 4-6 h after cholestyramine. Specific recommendations for colestipol are not available. Monitor for decreased concentrations/effects of the thyroid product. Consider therapy modification
Calcium Polystyrene Sulfonate: May decrease the serum concentration of Thyroid Products. Management: To minimize risk of interaction, separate dosing of oral calcium polystyrene sulfonate and thyroid products (eg, levothyroxine) or administer calcium polystyrene sulfonate rectally. Monitor for signs/symptoms of hypothyroidism with concomitant use (oral). Consider therapy modification
Calcium Salts: May diminish the therapeutic effect of Thyroid Products. Management: Separate the doses of the thyroid product and the oral calcium supplement by at least 4 hours. Consider therapy modification
CarBAMazepine: May decrease the serum concentration of Thyroid Products. Monitor therapy
Ciprofloxacin (Systemic): May decrease the serum concentration of Thyroid Products. Monitor therapy
Estrogen Derivatives: May diminish the therapeutic effect of Thyroid Products. Monitor therapy
Fosphenytoin: May decrease the serum concentration of Thyroid Products. Phenytoin may also displace thyroid hormones from protein binding sites. Monitor therapy
Lanthanum: May decrease the serum concentration of Thyroid Products. Management: Administer oral thyroid products at least two hours before or after lanthanum. Consider therapy modification
Phenytoin: May decrease the serum concentration of Thyroid Products. Phenytoin may also displace thyroid hormones from protein binding sites. Monitor therapy
Piracetam: May enhance the adverse/toxic effect of Thyroid Products. Specifically, symptoms including confusion, irritability, and sleep disorder have been described during concomitant use. Monitor therapy
RifAMPin: May decrease the serum concentration of Thyroid Products. Monitor therapy
Ritonavir: May diminish the therapeutic effect of Thyroid Products. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May diminish the therapeutic effect of Thyroid Products. Thyroid product dose requirements may be increased. Monitor therapy
Sodium Iodide I131: Thyroid Products may diminish the therapeutic effect of Sodium Iodide I131. Avoid combination
Sodium Polystyrene Sulfonate: May decrease the serum concentration of Thyroid Products. Management: To minimize risk of interaction, separate dosing of oral sodium polystyrene sulfonate and thyroid products (e.g., levothyroxine) or administer sodium polystyrene sulfonate rectally. Monitor for signs/symptoms of hypothyroidism with concomitant use (oral). Consider therapy modification
Somatropin: May diminish the therapeutic effect of Thyroid Products. Monitor therapy
Theophylline Derivatives: Thyroid Products may increase the metabolism of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
Tricyclic Antidepressants: Thyroid Products may enhance the arrhythmogenic effect of Tricyclic Antidepressants. Thyroid Products may enhance the stimulatory effect of Tricyclic Antidepressants. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Thyroid Products may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Test Interactions
T4-binding globulin (TBG): Factors that alter binding in serum (ATA/AACE [Garber 2012]):
Note: T4 is ~99.97% protein bound. Factors that alter protein binding will affect serum total T4 levels; however, measurement of serum free T4 (the metabolically active moiety) has largely replaced serum total T4 for thyroid status assessment.
Conditions/states that increase TBG binding: Pregnancy, hepatitis, porphyria, neonatal state
Medications that increase TBG binding: Estrogens, 5-fluorouracil, heroin, methadone, mitotane, perphenazine, selective estrogen receptor modulators (eg, tamoxifen, raloxifene)
Conditions/states that decrease TBG binding: Hepatic failure, nephrosis, severe illness
Medications that decrease TBG binding: Androgens, anabolic steroids, glucocorticoids, L-asparaginase, nicotinic acid
Thyroxine (T4) and Triiodothyronine (T3): Serum binding inhibitors (ATA/AACE [Garber 2012]):
Medications that inhibit T4 and T3 binding: Carbamazepine, furosemide, free fatty acids, heparin, NSAIDS (variable, transient), phenytoin, salicylates
Thyroid gland hormone: Interference with production and secretion (ATA/AACE [Garber 2012]):
Medications affecting iodine uptake: Amiodarone, iodinated contrast agents, iodine, ethionamide
Medications affecting hormone production: Amiodarone, ethionamide, iodinated contrast agents, iodine, sulfonylureas, sulfonamides, thionamides (carbimazole, methimazole, propylthiouracil)
Medications affecting secretion: Amiodarone, iodinated contrast agents, iodine, lithium
Medications inducing thyroiditis: Alemtuzumab, amiodarone, antiangiogenic agents (lenalidomide, thalidomide), denileukin diftitoxin, interferon alpha, interleukins, lithium, tyrosine kinase inhibitors (sunitinib, sorafenib)
Medications potentially causing the development of Graves’: Alemtuzumab, interferon alpha, antiretroviral therapy
Medications potentially ameliorating thyroiditis (if autoimmune) or Graves’: Glucocorticoids
Hypothalamic-pituitary axis and TSH: Interference with secretion (ATA/AACE [Garber 2012]):
Medications decreasing TSH secretion: Bexarotene, dopamine, dopaminergic agonists (bromocriptine, cabergoline), glucocorticoids, interleukin-6, metformin, opiates, somatostatin analogues (octreotide, lanreotide), thyroid hormone analogues
Medications increasing TSH secretion: Amphetamine, interleukin 2, metoclopramide, ritonavir, St John's wort
Medications potentially causing hypophysitis: Ipilimumab
Adverse Reactions
Adverse reactions are often indicative of excess thyroid replacement and/or hyperthyroidism.
<1%, postmarketing, and/or case reports: Abdominal cramps, alopecia, ataxia, cardiac arrhythmia, chest pain, constipation, diaphoresis, diarrhea, dyspnea, fever, headache, heat intolerance, increased appetite, insomnia, menstrual disease, myalgia, nervousness, palpitations, tachycardia, tremor, tremor of hands, vomiting, weight loss
Warnings/Precautions
Disease-related concerns:
- Adrenal insufficiency: Use with caution in patients with adrenal insufficiency; symptoms may be exaggerated or aggravated; contraindicated in patients with uncorrected adrenal insufficiency. Treatment with glucocorticoids should precede thyroid replacement therapy in patients with adrenal insufficiency (ATA/AACE [Garber 2012]).
- Cardiovascular disease: Use with caution and reduce dosage in patients with angina pectoris or other cardiovascular disease; chronic hypothyroidism predisposes patients to coronary artery disease.
- Diabetes: Use with caution in patients with diabetes mellitus and insipidus; symptoms may be exaggerated or aggravated.
- Myxedema: Use with caution in patients with myxedema; symptoms may be exaggerated or aggravated; initial dosage reduction is recommended in patients with long-standing myxedema.
Dosage form specific issues:
- Desiccated thyroid: Contains variable amounts of T3, T4, and other triiodothyronine compounds which are more likely to cause cardiac signs or symptoms due to fluctuating levels.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Infertility (unapproved use): Thyroid supplements are not recommended for the treatment of female or male infertility, unless associated with hypothyroidism.
- Porcine derived: Some desiccated thyroid products are acquired from porcine thyroid glands of pigs processed for human food; production also occurs at a facility that handles bovine tissues from cows processed for human food. Contamination with porcine or bovine viruses, or other novel or unidentified viruses, is potentially a risk; however, there have been no reported cases of transmission of an infectious illness.
- Weight reduction (unapproved use): [US Boxed Warning]: In euthyroid patients, thyroid supplements within the range of daily hormonal requirements are ineffective for weight reduction. High doses may produce serious or even life-threatening toxic effects particularly when used with some anorectic drugs (eg, sympathomimetic amines).
Monitoring Parameters
TSH 4 to 6 weeks after treatment initiation or dose changes, 4 to 6 months after adequate replacement dose determined, followed by every 12 months thereafter (or more frequently depending on clinical situation) (Jonklaas 2014); T4; heart rate, blood pressure; clinical signs of hypo- and hyperthyroidism; TSH is the most reliable guide for evaluating adequacy of thyroid replacement dosage in primary thyroid dysfunction. TSH may be elevated during the first few months of thyroid replacement despite patients being clinically euthyroid. In cases where T4 remains low and TSH is within normal limits, an evaluation of “free” (unbound) T4 is needed to evaluate further increase in dosage. Free T4 (not TSH) should be monitored to guide treatment in patients with central hypothyroidism (ATA/AACE [Garber 2012]).
Pregnancy
Pregnancy Risk Factor
A
Pregnancy Considerations
Endogenous thyroid hormones minimally cross the placenta. Desiccated thyroid has not been found to adversely affect the fetus following maternal use during pregnancy.
Uncontrolled maternal hypothyroidism may result in adverse neonatal and maternal outcomes (ACOG 2015). Subnormal intellectual development may occur in infants of mothers with serum thyroxine concentrations in the lowest tenth percentile at the end of the first trimester (ATA/AACE [Garber 2012]). To prevent adverse events, normal maternal thyroid function should be maintained prior to conception and throughout pregnancy and thyroid replacement should not be discontinued during pregnancy (ACOG 2015). However, desiccated thyroid is not the preferred treatment for hypothyroidism in pregnant women because use may result in lowering serum thyroxine concentrations. Women treated with desiccated thyroid who are planning to conceive or who become pregnant should be transitioned to a preferred therapy and TSH should be monitored (ACOG 2015; ATA/AACE [Garber 2012]).
Patient Education
What is this drug used for?
- It is used to add thyroid hormone to the body.
- It is used to treat or prevent an enlarged thyroid.
- It is used to manage thyroid cancer.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Hair loss
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Chest pain
- Fast heartbeat
- Abnormal heartbeat
- Headache
- Shortness of breath
- Swelling of arms or legs
- Lump in neck
- Anxiety
- Tremors
- Trouble sleeping
- Sensitivity to heat
- Sweating a lot
- Lack of appetite
- Increased hunger
- Excessive weight gain
- Weight loss
- Diarrhea
- Vomiting
- Irritability
- Abdominal cramps
- Leg cramps
- Muscle weakness
- Menstrual changes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.