Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral, as hydrochloride:
Gabitril: 2 mg [contains fd&c yellow #6 (sunset yellow)]
Gabitril: 4 mg [contains fd&c yellow #10 (quinoline yellow)]
Gabitril: 12 mg [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #10 (quinoline yellow)]
Gabitril: 16 mg [contains fd&c blue #2 (indigotine)]
Generic: 2 mg, 4 mg, 12 mg, 16 mg
Pharmacology
Mechanism of Action
The exact mechanism by which tiagabine exerts antiseizure activity is not definitively known; however, in vitro experiments demonstrate that it enhances the activity of gamma aminobutyric acid (GABA). It is thought that the binding of tiagabine to the GABA uptake carrier inhibits the uptake of GABA into presynaptic neurons, allowing an increased amount of GABA to be available to postsynaptic neurons; based on in vitro studies, tiagabine does not inhibit the uptake of dopamine, norepinephrine, serotonin, glutamate, or choline
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid (45 minutes), well absorbed (>95%); prolonged with food
Distribution
Note: Vd values are more similar between children and adults when expressed as L/m2 (Gustavson 1997); Mean Vd:
Children 3 to 10 years: 2.4 L/kg
Adults: 1.3 to 1.6 L/kg
Metabolism
Hepatic via CYP (primarily 3A4); undergoes enterohepatic recirculation
Excretion
Feces (63%); urine (25%); 2% as unchanged drug; primarily as metabolites
Clearance: Note: Clearance values are more similar between children and adults when expressed as mL/minute/m2 (Gustavson 1997)
Children 3 to 10 years: 4.2 ± 1.6 mL/minute/kg
Children 3 to 10 years receiving enzyme-inducing AEDs: 8.6 ± 3.3 mL/minute/kg
Adults (normal volunteers): 109 mL/minute
Adult patients: 1.9 ± 0.5 mL/minute/kg
Adult patients receiving enzyme-inducing AEDs: 6.3 ± 3.5 mL/minute/kg
Hepatic impairment: Clearance of unbound drug is decreased by 60%
Time to Peak
Plasma: Fasting state: 45 minutes
Half-Life Elimination
Children 3 to 10 years: Mean: 5.7 hours (range: 2 to 10 hours); receiving enzyme-inducing AEDs: Mean: 3.2 hours (range: 2 to 7.8 hours)
Adults: 7 to 9 hours; receiving enzyme-inducing AEDs: 2 to 5 hours
Protein Binding
96%, primarily to albumin and alpha-1 acid glycoprotein
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Moderate hepatic impairment (Child-Pugh class B) caused a 60% decrease in the Cl of unbound tiagabine.
Use: Labeled Indications
Partial seizures: Adjunctive therapy in adults and children ≥12 years in the treatment of partial seizures
Contraindications
Hypersensitivity to tiagabine or any component of the formulation
Dosage and Administration
Dosing: Adult
Partial seizures (adjunct): Oral: Note: Do not use a loading dose, rapid titration, and/or increases with large dose increments.
Patients receiving enzyme-inducing AED regimens: Initial: 4 mg once daily for 1 week; may increase by 4 to 8 mg at weekly intervals, based on clinical response, up to 56 mg daily in 2 to 4 divided doses; usual maintenance: 32 to 56 mg/day
Patients not receiving enzyme-inducing AED regimens: The estimated plasma concentrations of tiagabine in patients not taking enzyme-inducing medications is twice that of patients receiving enzyme-inducing AEDs. Lower doses are required; slower titration may be necessary.
Dosage adjustment: Consider dosage adjustment when a change in enzyme-inducing status occurs due to the addition, discontinuation, or dose change of the enzyme-inducing agent. If multiple doses are missed, evaluate if retitration is clinically indicated.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Partial seizures; adjunctive therapy: Note: Do not use loading doses of tiagabine in any patient; do not use a rapid dosage escalation or increase the dose in large increments.
Children and Adolescents 12 to 18 years:
Patients receiving enzyme-inducing AED regimens: Oral: Initial: 4 mg once daily for 1 week, then 8 mg/day given in 2 divided doses for 1 week, then increase weekly by 4 to 8 mg/day; administer in 2 to 4 divided doses per day; titrate dose to response; maximum dose: 32 mg/day (doses >32 mg/day have been used in select adolescent patients for short periods of time)
Patients not receiving enzyme-inducing AED regimens: Oral: The estimated plasma concentrations of tiagabine in patients not taking enzyme-inducing medications is twice that of patients receiving enzyme-inducing AEDs. Lower doses are required; slower titration may be necessary.
Dosage adjustment: Consider dosage adjustment when a change in enzyme-inducing status occurs due to the addition, discontinuation, or dose change of the enzyme-inducing agent. If multiple doses are missed, evaluate if retitration is clinically indicated.
Extemporaneously Prepared
A 1 mg/mL tiagabine hydrochloride oral suspension may be made with tablets and a 1:1 mixture of Ora-Sweet® and Ora-Plus®. Crush ten 12 mg tablets in a mortar and reduce to a fine powder. Add small portions of the vehicle and mix to a uniform paste; mix while adding the vehicle in incremental proportions to almost 120 mL; transfer to a graduated cylinder; rinse mortar with vehicle, and add quantity of vehicle sufficient to make 120 mL. Label "shake well" and "refrigerate". Store in amber plastic prescription bottles; stable for 70 days at room temperature or 91 days refrigerated (preferred) (Nahata 2004).
A 1 mg/mL oral suspension may be made with tablets and a 6:1 mixture of simple syrup, NF and methylcellulose 1%. Crush ten 12 mg tablets in a mortar and reduce to a fine powder. Add 17 mL of methylcellulose 1% gel and mix to a uniform paste; mix while adding simple syrup, NF in incremental proportions to almost 120 mL; transfer to a graduated cylinder, rinse mortar with syrup, and add quantity of syrup sufficient to make 120 mL. Label "shake well" and "refrigerate". Store in amber plastic prescription bottles; stable for 42 days at room temperature or 91 days refrigerated (preferred) (Nahata 2004).
Administration
Oral: Administer with food.
Storage
Store at controlled room temperature of 20°C to 25°C (68°F to 77°F). Protect from moisture and light.
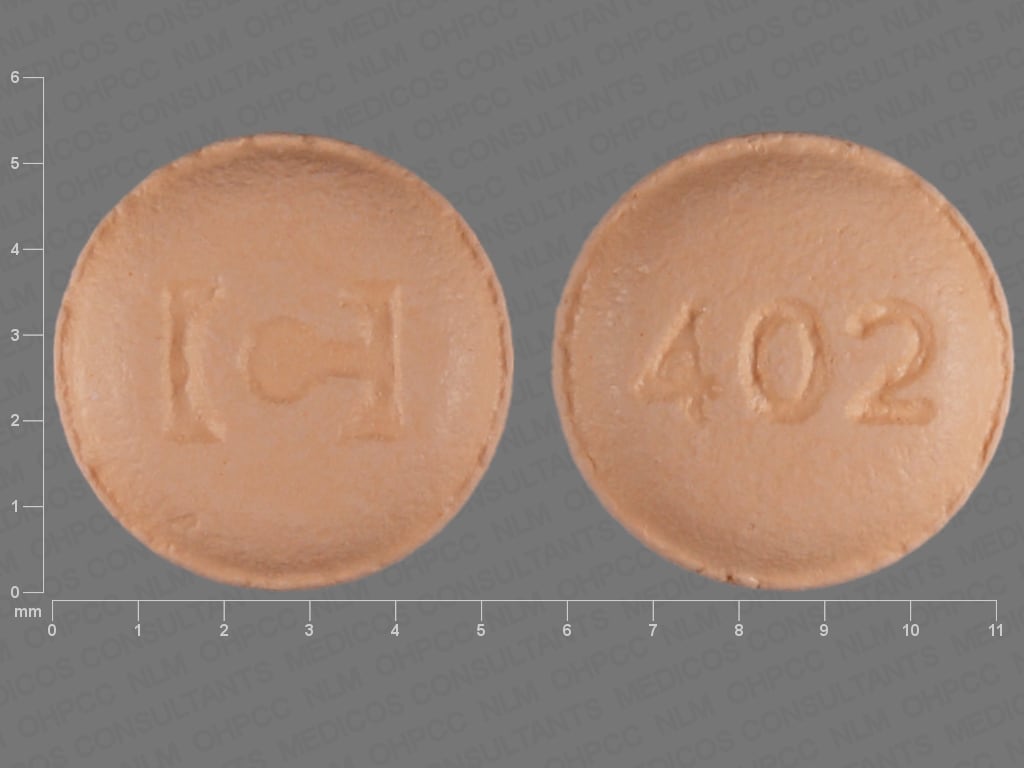
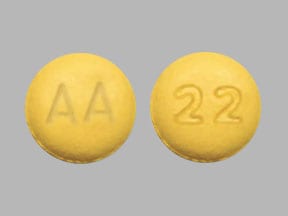
TiaGABine Images
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Aprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Clofazimine: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Conivaptan: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of TiaGABine. Management: Approximately 2-fold higher tiagabine doses and a more rapid dose titration will likely be required in patients concomitantly taking a strong CYP3A4 inducer. Consider therapy modification
CYP3A4 Inhibitors (Moderate): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
CYP3A4 Inhibitors (Strong): May decrease the metabolism of CYP3A4 Substrates (High risk with Inhibitors). Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Duvelisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Erdafitinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosaprepitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fosnetupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Idelalisib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Avoid combination
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Larotrectinib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May diminish the therapeutic effect of Anticonvulsants. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Minimize doses of CYP3A4 substrates, and monitor for increased concentrations/toxicity, during and 2 weeks following treatment with mifepristone. Avoid cyclosporine, dihydroergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, and tacrolimus. Consider therapy modification
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Netupitant: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Palbociclib: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Simeprevir: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Stiripentol: May increase the serum concentration of CYP3A4 Substrates (High risk with Inhibitors). Management: Use of stiripentol with CYP3A4 substrates that are considered to have a narrow therapeutic index should be avoided due to the increased risk for adverse effects and toxicity. Any CYP3A4 substrate used with stiripentol requires closer monitoring. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
>10%:
Central nervous system: Dizziness (27% to 31%), drowsiness (18% to 21%), nervousness (10% to 14%), lack of concentration (7% to 14%)
Gastrointestinal: Nausea (11%)
Infection: Infection (19%)
Neuromuscular & skeletal: Weakness (18% to 23%), tremor (9% to 21%)
Miscellaneous: Accidental injury (21%)
1% to 10%:
Cardiovascular: Vasodilation (2%), chest pain (≥1%), edema (≥1%), hypertension (≥1%), palpitations (≥1%), peripheral edema (≥1%), syncope (≥1%), tachycardia (≥1%)
Central nervous system: Ataxia (5% to 9%), pain (5% to 7%), depression (1% to 7%), insomnia (5% to 6%), confusion (5%), status epilepticus (5%), abnormal gait (3% to 5%), hostility (2% to 5%), memory impairment (4%), paresthesia (4%), speech disturbance (4%), emotional lability (3%), chills (≥1%), depersonalization (≥1%), dysarthria (≥1%), euphoria (≥1%), hallucination (≥1%), hypertonia (≥1%), hypoesthesia (≥1%), hyporeflexia (≥1%), hypotonia (≥1%), malaise (≥1%), migraine (≥1%), myoclonus (≥1%), paranoia (≥1%), personality disorder (≥1%), stupor (≥1%), twitching (≥1%), vertigo (≥1%), agitation (1%), myasthenia (1%)
Dermatologic: Bruise (6%), skin rash (5%), pruritus (2%), alopecia (≥1%), xeroderma (≥1%)
Gastrointestinal: Diarrhea (7% to 10%), vomiting (7%), abdominal pain (5% to 7%), increased appetite (2%), gingivitis (≥1%), stomatitis (≥1%), oral mucosa ulcer (1%)
Endocrine & metabolic: Weight gain (≥1%), weight loss (≥1%)
Genitourinary: Urinary tract infection (5%), abnormal uterine bleeding (≥1%), dysmenorrhea (≥1%), dysuria (≥1%), urinary incontinence (≥1%), vaginitis (≥1%)
Hematologic & oncologic: Lymphadenopathy (≥1%)
Hypersensitivity: Hypersensitivity reaction (≥1%)
Neuromuscular & skeletal: Myalgia (5%), arthralgia (≥1%), hyperkinesia (≥1%), hypokinesia (≥1%), neck pain (≥1%)
Ophthalmic: Amblyopia (9%), nystagmus (2%), visual disturbance (≥1%)
Otic: Otalgia (≥1%), otitis media (≥1%), tinnitus (≥1%)
Respiratory: Flu-like symptoms (6% to 9%), pharyngitis (7% to 8%), increased cough (4%), bronchitis (≥1%), dyspnea (≥1%), epistaxis (≥1%), pneumonia (≥1%)
Miscellaneous: Language problems (2%), cyst (≥1%), diaphoresis (≥1%)
<1%, postmarketing, and/or case reports: Abnormal dreams, abnormal electroencephalogram, abnormal erythrocytes, abnormal hepatic function tests, abnormal pap smear, abnormal stools, abscess, ageusia, altered sense of smell, amenorrhea, anemia, angina pectoris, apathy, aphthous stomatitis, apnea, arthritis, asthma, benign skin neoplasm, blepharitis, blindness, blurred vision, brain disease, breast hypertrophy, bullous dermatitis, bursitis, cellulitis, cerebral ischemia, cholecystitis, cholelithiasis, CNS neoplasm, coma, contact dermatitis, cutaneous nodule, cystitis, deafness, dehydration, delusions, dental caries, dermal ulcer, dysgeusia, dysphagia, dystonia, ECG abnormality, eczema, eructation, esophagitis, exfoliative dermatitis, eye pain, facial edema, fecal incontinence, fibrocystic breast disease, furunculosis, gastritis, gastrointestinal hemorrhage, gingival hyperplasia, glossitis, goiter, halitosis, hematuria, hemiplegia, hemoptysis, hemorrhage, hepatomegaly, hernia, herpes simplex infection, herpes zoster, hiccups, hirsutism, hyperacusis, hypercholesteremia, hyperglycemia, hyperlipemia, hypermenorrhea, hyperreflexia, hyperventilation, hypoglycemia, hypokalemia, hyponatremia, hypotension, hypothyroidism, impotence, increased libido, increased thirst, keratoconjunctivitis, laryngitis, leg cramps, leukopenia, maculopapular rash, mastalgia, melena, movement disorder, muscle spasm, myocardial infarction, neck stiffness, neoplasm, neuritis, nocturia, oral paresthesia, orthostatic hypotension, osteoarthrosis, otitis externa, pallor, paralysis, pelvic pain, periodontal abscess, peripheral neuritis, peripheral vascular disease, petechia, phlebitis, photophobia, polyuria, psoriasis, psychoneurosis, psychosis, pyelonephritis, rectal hemorrhage, renal failure, salpingitis, seizure (in patients with or without underlying seizure disorder), sepsis, sialorrhea, skin carcinoma, skin discoloration, skin photosensitivity, status epilepticus, Stevens-Johnson syndrome, subcutaneous nodule, suicidal ideation, suicidal tendencies, tendinous contracture, thrombocytopenia, thrombophlebitis, urethritis, urinary retention, urinary urgency, urticaria, vaginal hemorrhage, vesiculobullous dermatitis, visual field defect, voice disorder, withdrawal syndrome (seizures with abrupt withdrawal), xerostomia
Warnings/Precautions
Concerns related to adverse effects:
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Dermatologic reactions: Severe reactions, including Stevens-Johnson syndrome, although rarely reported, have resulted in fatalities.
- Generalized weakness: Moderately severe to incapacitating generalized weakness has been reported after administration of tiagabine. The weakness resolved in all cases after a reduction in dose or discontinuation of tiagabine.
- Ophthalmic effects: Evidence of residual binding of tiagabine in the retina and uvea after 3 weeks has been observed in animal studies; although not directly measured, melanin binding is suggested. Long-term (up to 1 year) toxicological studies of tiagabine in animals showed no treatment-related ophthalmoscopic changes and macro- and microscopic examinations of the eye were unremarkable. The ability of available tests to detect potentially adverse consequences, if any, of the binding of tiagabine to melanin-containing tissue is unknown, and there was no systematic monitoring for relevant ophthalmological changes during the clinical development of tiagabine. Prescribers should be aware of the possibility of long-term ophthalmologic effects.
- Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; notify health care provider immediately if symptoms occur.
Disease-related concerns:
- Hepatic impairment: Use with caution in patients with hepatic impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Enzyme-inducing drugs: Experience in patients not receiving enzyme-inducing drugs has been limited; caution should be used in treating any patient who is not receiving one of these medications (decreased dose and slower titration may be required).
Other warnings/precautions:
- Off-label use: New-onset seizures and status epilepticus have been associated with tiagabine use when taken for off-label indications. Seizures have occurred with doses as low as 4 mg/day and shortly after a dosage increase, even after stable therapy. In most cases, patients were using concomitant medications (eg, antidepressants, antipsychotics, stimulants, opioids). In these instances, the discontinuation of tiagabine, followed by an evaluation for an underlying seizure disorder, is suggested. Use for unapproved indications, however, has not been proven to be safe or effective and is not recommended.
- Withdrawal: Anticonvulsants should not be discontinued abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal.
Monitoring Parameters
Seizure frequency, liver function tests (periodically), suicidality (eg, suicidal thoughts, depression, behavioral changes)
Pregnancy
Pregnancy Considerations
Adverse events were observed in animal reproduction studies. Information specific to the use of tiagabine in pregnancy is limited (Leppik 1999; Neppe 2000). Patients exposed to tiagabine during pregnancy are encouraged to enroll themselves into the North American Antiepileptic Drug (NAAED) Pregnancy Registry by calling 1-888-233-2334. Additional information is available at www.aedpregnancyregistry.org.
Patient Education
- Discuss specific use of drug and side effects with patient as it relates to treatment. (HCAHPS: During this hospital stay, were you given any medicine that you had not taken before? Before giving you any new medicine, how often did hospital staff tell you what the medicine was for? How often did hospital staff describe possible side effects in a way you could understand?)
- Patient may experience dizziness, nausea, vomiting, abdominal pain, anxiety, diarrhea, trouble sleeping, sore throat, flu-like signs, muscle pain, or tremors. Have patient report immediately to prescriber signs of depression (thoughts of suicide, anxiety, emotional instability, or confusion), seizures, change in balance, confusion, vision changes, change in color vision, severe loss of strength and energy, severe fatigue, difficulty focusing, difficulty speaking, abnormal gait, agitation, irritability, panic attacks, mood changes, restlessness, or signs of Stevens-Johnson syndrome/toxic epidermal necrolysis (red, swollen, blistered, or peeling skin [with or without fever]; red or irritated eyes; or sores in mouth, throat, nose, or eyes) (HCAHPS).
- Educate patient about signs of a significant reaction (eg, wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat). Note: This is not a comprehensive list of all side effects. Patient should consult prescriber for additional questions.
Intended Use and Disclaimer: Should not be printed and given to patients. This information is intended to serve as a concise initial reference for health care professionals to use when discussing medications with a patient. You must ultimately rely on your own discretion, experience, and judgment in diagnosing, treating, and advising patients.