Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
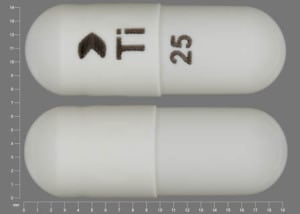
Capsule ER 24 Hour Sprinkle, Oral:
Qudexy XR: 25 mg, 50 mg, 100 mg, 150 mg, 200 mg
Generic: 25 mg, 50 mg, 100 mg, 150 mg, 200 mg
Capsule Extended Release 24 Hour, Oral:
Trokendi XR: 25 mg [contains brilliant blue fcf (fd&c blue #1), sodium benzoate]
Trokendi XR: 50 mg, 100 mg, 200 mg [contains brilliant blue fcf (fd&c blue #1), fd&c yellow #6 (sunset yellow), sodium benzoate]
Capsule Sprinkle, Oral:
Topamax Sprinkle: 15 mg, 25 mg
Generic: 15 mg, 25 mg
Tablet, Oral:
Topamax: 25 mg, 50 mg, 100 mg, 200 mg
Generic: 25 mg, 50 mg, 100 mg, 200 mg
Pharmacology
Mechanism of Action
Anticonvulsant activity may be due to a combination of potential mechanisms: Blocks neuronal voltage-dependent sodium channels, enhances GABA(A) activity, antagonizes AMPA/kainate glutamate receptors, and weakly inhibits carbonic anhydrase.
Pharmacokinetics/Pharmacodynamics
Absorption
Good, rapid; immediate release formulation is unaffected by food. A single Trokendi XR dose with a high-fat meal increased the Cmax by 37% and shortened the Tmax to approximately 8 hours; this effect is significantly reduced following repeat administrations. A single Qudexy XR dose with a high-fat meal delayed the Tmax by 4 hours.
Distribution
Vd: 0.6 to 0.8 L/kg
Metabolism
Not extensively metabolized. Minor amounts metabolized in liver via hydroxylation, hydrolysis, and glucuronidation; there is evidence of renal tubular reabsorption; percentage of dose metabolized in liver and clearance are increased in patients receiving enzyme inducers (eg, carbamazepine, phenytoin)
Excretion
Urine (~70% as unchanged drug); may undergo renal tubular reabsorption
Clearance:
Not receiving concomitant enzyme inducers or valproic acid:
Neonates (full-term) with hypothermia: 13.4 mL/kg/hour (Filippi 2009)
Infants and Children 9 months to <4 years: 46.5 mL/kg/hour (range: 30.5 to 70.9 mL/kg/hour) (Mikaeloff 2004)
Children 4 to 17 years: 27.6 mL/kg/hour (Rosenfeld 1999)
Receiving concomitant enzyme inducers:
Neonates (full-term) with hypothermia: 17.9 mL/kg/hour (Filippi 2009)
Infants and Children 9 months to <4 years: 85.4 mL/kg/hour (range: 46.2 to 135 mL/kg/hour) (Mikaeloff 2004)
Children and Adolescents 4 to 17 years: 60.6 mL/kg/hour (Rosenfeld 1999)
Receiving valproic acid: Infants and Children 9 months to <4 years: 49.6 mL/kg/hour (range: 26.6 to 60.2 mL/kg/h) (Mikaeloff 2004)
Adults: 20 to 30 mL/minute
Time to Peak
Immediate release:
Neonates (full-term) with hypothermia: 3.8 hours (Filippi 2009)
Infants and Children 9 months to <4 years: 3.7 hours (range: 1.5 to 10.2 hours) (Mikaeloff 2004)
Children 4 to 17 years: Mean range: 1 to 2.8 hours (Rosenfeld 1999)
Adults: 2 hours; range: 1.4 to 4.3 hours
Extended release: Qudexy XR: ~20 hours; Trokendi XR: ~24 hours
Half-Life Elimination
Immediate release:
Not receiving concomitant enzyme inducers or valproic acid:
Neonates (full-term) with hypothermia: ~43 hours (Filippi 2009)
Infants and Children 9 months to <4 years: 10.4 hours (range: 8.5 to 15.3 hours) (Mikaeloff 2004)
Children 4 to 7 years: Mean range: 7.7 to 8 hours (Rosenfeld 1999)
Children 8 to 11 years: Mean range: 11.3 to 11.7 hours (Rosenfeld 1999)
Children and Adolescents 12 to 17 years: Mean range: 12.3 to 12.8 hours (Rosenfeld 1999)
Receiving concomitant enzyme inducers (eg, carbamazepine, phenytoin, phenobarbital):
Neonates (full-term) with hypothermia: 26.5 hours (Filippi 2009)
Infants and Children 9 months to <4 years: 6.5 hours (range: 3.75 to 10.2 hours) (Mikaeloff 2004)
Children and Adolescents 4 to 17 years: 7.5 hours (Rosenfeld 1999)
Receiving valproic acid: Infants and Children 9 months to 4 years: 9.2 hours (range: 7.23 to 12 hours) (Mikaeloff 2004)
Adults: 19 to 23 hours (mean: 21 hours)
Adults with renal impairment: 59 ± 11 hours
Extended release: Qudexy XR: ~56 hours; Trokendi XR: ~31 hours
Protein Binding
15% to 41% (inversely related to plasma concentrations)
Use in Specific Populations
Special Populations: Renal Function Impairment
Clearance is reduced 42% in moderately impaired (creatinine clearance [CrCl] 30 to 69 mL/minute/1.73 m2) and 54% in severely impaired (CrCl <30 mL/minute/1.73 m2) patients. Significantly hemodialyzed; dialysis clearance is 120 mL/minute (4-6 times higher than in adults with normal renal function).
Special Populations: Hepatic Function Impairment
Clearance is reduced by a mean of 26% in patients with moderate to severe hepatic impairment.
Special Populations: Elderly
Half-life elimination is longer. Plasma and renal clearance were reduced 21% and 19%, respectively. Reduced clearance resulted in slightly higher Cmax (23% for immediate release; 30% for Trokendi XR) and AUC (25% for immediate release; 44% for Trokendi XR). Topiramate clearance is decreased only to the extent that renal function is reduced. Tmax for Trokendi XR is shorter (16 hours).
Use: Labeled Indications
Migraine (prevention): Prophylaxis of migraine headache in patients ≥12 years of age
Seizures: Monotherapy or adjunctive therapy in patients ≥2 years of age (immediate release and Qudexy XR) or ≥6 years of age (Trokendi XR) with focal (partial) onset or primary generalized tonic-clonic seizures; adjunctive therapy in patients ≥2 years of age (immediate release and Qudexy XR) or ≥6 years of age (Trokendi XR only) with seizures associated with Lennox-Gastaut syndrome
Use: Off Label
Antipsychotic-induced weight gainbyes
Data from multiple meta-analyses with varying degrees of heterogeneity support the use of topiramate in promoting modest weight loss and preventing weight gain associated with second-generation antipsychotics in patients with schizophrenia (evidence is more limited in patients with bipolar disorder) Correll 2016, Das 2012, Fiedorowicz 2012, Mahmood 2013, Mizuno 2014.
Based on the Canadian Network for Mood and Anxiety Treatments (CANMAT) recommendations for the management of patients with mood disorders and comorbid metabolic disorders, topiramate is recommended as a second-line option after nonpharmacologic strategies for managing weight gain in patients with bipolar and major depressive disorders, and is recognized as often being used as a secondary prevention strategy for antipsychotic-related weight gain
Binge eating disorderbyes
Data from 3 randomized, double-blind, placebo-controlled trials support the use of topiramate in the treatment of binge eating disorder for reduction of binge episode frequency and body weight Claudino 2007, McElroy 2003, McElroy 2007.
Based on the
Headache, cluster (prevention)c
Data from a limited number of preliminary clinical trials suggest that topiramate may be beneficial in the prevention of cluster headache Pascual 2007.
Based on the European Federation of Neurological Societies (EFNS) guidelines on the treatment of cluster headache and other trigeminal-autonomic cephalalgias, topiramate is probably effective for the prevention of cluster headache and may be considered as an alternative treatment option.
Headache, short-lasting unilateral neuralgiform attacks (prevention)c
Data from a limited number of patients studied suggest that topiramate may be beneficial for the prevention of short-lasting unilateral neuralgiform headache attacks Cohen 2007.
Tremor, essentialbyes
Data from a randomized, double-blind, controlled study and a pooled analysis of 3 double-blind, placebo-controlled, crossover studies support the use of topiramate in the treatment of essential tremor; however, many patients experienced treatment-limiting adverse effects including paresthesia, nausea, concentration/attention difficulty, and somnolence Connor 2008, Ondo 2006.
Based on the
Contraindications
Extended release: Recent alcohol use (ie, within 6 hours prior to and 6 hours after administration) (Trokendi XR only); patients with metabolic acidosis who are taking concomitant metformin (Qudexy XR only).
Immediate release: There are no contraindications listed in the manufacturer's labeling.
Canadian labeling: Hypersensitivity to topiramate or any component of the formulation or container; pregnancy and women in childbearing years not using effective contraception (migraine prophylaxis only).
Dosage and Administration
Dosing: Adult
Note: The dosing recommendations in this monograph are expressed as the total daily dose (ie, per 24 hours) unless stated otherwise. The total daily oral dose is given in 1 to 2 divided doses per day depending on the type of preparation. Available preparations include: Oral immediate release (IR) (dosed twice daily) and extended release (ER) (dosed once daily).
Binge-eating disorder (alternative agent) (off-label use):
Oral: Initial: 25 mg once daily; increase dose gradually in progressively larger increments of 25 to 100 mg at intervals ≥1 week based on response and tolerability up to 400 mg/day (McElroy 2007).
Headache, cluster (prevention) (alternative agent; adjunctive therapy) (off-label use):
Note: Some experts often use in combination with verapamil (May 2019).
Oral: Initial: 25 to 50 mg once daily; increase dose gradually in 25 to 50 mg increments at intervals ≥1 week based on response and tolerability, up to a recommended dose of 100 mg/day; a further increase up to 200 mg/day may be necessary in some patients for optimal response (EFNS [May 2006]; Pascual 2007).
Headache, short-lasting unilateral neuralgiform attacks (prevention) (alternative agent) (off-label use): Based on limited data:
Oral: Initial: 15 to 25 mg once daily; may increase dose based on response and tolerability in 25 mg increments every 2 weeks up to 100 mg/day in 2 divided doses, and thereafter in 50 mg increments every few weeks up to 400 mg/day (Cohen 2007; Matharu 2019).
Migraine (prevention):
Oral: Initial: 25 mg once daily; increase dose in 25 to 50 mg increments at intervals ≥1 week based on response and tolerability up to 100 mg/day. Some patients may require up to 200 mg/day for optimal response; however, adverse effects may increase (Linde 2013).
Seizures:
Note: FDA-approved as monotherapy and adjunctive therapy for focal (partial) onset seizures and primary generalized tonic-clonic seizures, or as adjunctive therapy for Lennox-Gastaut syndrome; may be used off label for other seizure types.
Monotherapy: Oral: Initial: 50 mg/day; increase dose in 50 mg increments at weekly intervals based on response and tolerability up to 200 mg/day; thereafter, may further increase in 100 mg increments at weekly intervals up to 400 mg/day.
Adjunctive therapy: Oral: Initial: 25 to 50 mg/day; increase in 25 to 50 mg increments at weekly intervals based on response and tolerability up to 400 mg/day.
Tremor, essential (alternative agent for patients who fail preferred therapies) (off-label use):
Oral: Initial: 25 mg once or twice daily; increase dose gradually in increments of 25 to 50 mg at intervals ≥1 week based on response and tolerability up to 400 mg/day (AAN [Zesiewicz 2011]; Connor 2008; Ondo 2006).
Weight gain, antipsychotic-induced (alternative agent; adjunct to behavioral and antipsychotic modifications) (off-label use):
Oral: Initial: 50 mg/day; increase in 25 to 50 mg increments at weekly intervals based on response and tolerability up to a recommended dose of 200 mg/day (Jarskog 2019; Ko 2005; WFSBP [Hasan 2013]).
Dosing conversion:
Between IR and ER formulations: Convert using same total daily dose but adjust frequency as indicated for the IR (2 times daily) and ER (once daily) products.
Between ER formulations: Bioequivalence has not been demonstrated between Trokendi XR and Qudexy XR.
Discontinuation of therapy: In patients receiving topiramate long-term, unless safety concerns require a more rapid withdrawal, topiramate should be withdrawn gradually over a few weeks to several months to minimize the potential of seizures or other withdrawal symptoms (Schachter 2019). In clinical trials, adult doses were decreased by 50 to 100 mg each week over 2 to 8 weeks for seizure treatment, and by 25 to 50 mg each week for migraine prophylaxis.
Dosing: Geriatric
Most older adults have creatinine clearances <70 mL/minute/1.73 m2; obtain a serum creatinine and calculate creatinine clearance prior to initiation of therapy. An initial dose of 25 mg/day may be recommended, followed by incremental increases of 25 mg at weekly intervals until an effective dose is reached; refer to adult dosing for titration schedule.
Dosing: Pediatric
Note: Do not abruptly discontinue therapy; taper dosage gradually to prevent rebound effects.
Infantile spasms: Oral: Limited data available; dosing regimens variable. Consider twice-daily therapy once dose titration begins:
Newly diagnosed infantile spasm: Weight-directed dosing: Infants and Children 3 to 24 months: Immediate release: Initial: 1 to 3 mg/kg/day administered as 1 or 2 daily doses; titrate every 3 to 7 days in 1 to 3 mg/kg/day increments as tolerated until seizures controlled; reported mean dose range: 9.1 to 14 mg/kg/day; reported range: 4 to 27 mg/kg/day. Dosing based on two small studies; first was an open-label trial of 15 pediatric patients (mean age: 8 months; age range: 4 to 14 months) with newly diagnosed infantile spasms which used an initial dose of 3 mg/kg/day in 2 divided doses; doses were increased by 3 mg/kg/day every 3 days until seizures were controlled or toxicity developed; mean dose required: 14 mg/kg/day (9 to 27 mg/kg/day); median rate of spasm reduction was 41% within the first 2 months of therapy with 20% of patients becoming spasm free (three of 15 patients) and 33% achieving a 50% reduction in spasm frequency (five of 15 patients) (Hosain, 2006). In another trial of 20 pediatric patients (median age: 6.5 months; range: 3 to 24 months) with newly diagnosed infantile spasms, an initial dose of 1 mg/kg/day was used; dose was increased by 1 mg/kg/day at weekly intervals until seizures were controlled up to a maximum daily dose: 12 mg/kg/day; reported mean stabilizing dose: 9.1 mg/kg/day (4 to 12 mg/kg/day); results showed 30% of patients became spasm free (six of 20 patients) and 70% achieved at least a 50% reduction in spasm frequency (Kwon, 2006)
Refractory: Fixed dosing: Infants ≥3 months to Children ≤4 years; weight ≥7 kg: Immediate release: Initial: 25 mg/day once daily; titrate in 25 mg/day increments every 2 to 3 days as tolerated until seizures controlled up to a maximum daily dose: 24 mg/kg/day; dosing is from an open-label trial of 11 pediatric patients (mean age: 24 months) which reported a mean stabilizing dose of 15 mg/kg/day (8.3 to 23.7 mg/kg/day); results showed statistically significant decrease in spasm frequency with 45% of patients becoming spasm free (Glauser, 1998). In an extension phase of this study in eight of the initial subjects, the mean dose was 29 mg/kg/day (maximum daily dose: 50 mg/kg/day); 50% of the remaining patients (four of eight) were seizure free and all patients except one maintained a ≥50% reduction in spasm frequency (Glauser, 2000)
Anticonvulsant, adjunctive therapy: Oral:
Children and Adolescents 2 to 16 years:
Partial onset seizures or Lennox-Gastaut syndrome:
Immediate release: Children and Adolescents 2 to 16 years: Initial: 1 to 3 mg/kg/day (maximum dose: 25 mg/dose) administered nightly for 1 week; increase at 1- to 2-week intervals in increments of 1 to 3 mg/kg/day in 2 divided doses; titrate dose to response; usual maintenance: 5 to 9 mg/kg/day in 2 divided doses
Extended release:
Qudexy XR: Children and Adolescents 2 to 16 years: Initial: 25 mg once daily (approximately 1 to 3 mg/kg/day) administered nightly for 1 week; increase at 1- to 2-week intervals in increments of 1 to 3 mg/kg/day rounded to the nearest appropriate capsule size administered once daily; titrate dose to response; usual maintenance: 5 to 9 mg/kg/dose once daily; range: 5 to 9 mg/kg/dose once daily
Trokendi XR: Children and Adolescents 6 to 16 years, able to swallow capsule whole: Initial: 25 mg once daily (approximately 1 to 3 mg/kg/day) administered nightly for 1 week; increase at 1- to 2-week intervals in increments of 1 to 3 mg/kg/day rounded to the nearest appropriate capsule size administered once daily; titrate dose to response; usual maintenance: 5 to 9 mg/kg/dose once daily
Primary generalized tonic-clonic seizures:
Immediate release: Children and Adolescents 2 to 16 years: Initial: 1 to 3 mg/kg/day (maximum dose: 25 mg/dose) administered nightly for 1 week; increase over 8 weeks in increments of 1 to 3 mg/kg/day in 2 divided doses to a target dose of 6 mg/kg/day in 2 divided doses
Extended release:
Qudexy XR: Children and Adolescents 2 to 16 years: Initial: 25 mg once daily (approximately 1 to 3 mg/kg/day) administered nightly for 1 week; increase over 8 weeks in increments of 1 to 3 mg/kg/day rounded to the nearest appropriate capsule size to a target dose of 6 mg/kg/day once daily; range: 5 to 9 mg/kg/dose once daily
Trokendi XR: Children and Adolescents 6 to 16 years, able to swallow capsule whole: Initial: 25 mg once daily (approximately 1 to 3 mg/kg/day) administered nightly for 1 week; increase over 8 weeks in increments of 1 to 3 mg/kg/day rounded to the nearest appropriate capsule size to a target dose of 6 mg/kg/day once daily
Adolescents ≥17 years:
Partial onset seizures or Lennox-Gastaut syndrome:
Immediate release: Initial: 25 to 50 mg/day administered daily for 1 week; increase at weekly intervals by 25 to 50 mg/day; administer in 2 divided doses; titrate dose to response; usual maintenance dose: 100 to 200 mg twice daily; maximum daily dose: 1600 mg/day; Note: Doses above 400 mg/day have not been shown to increase efficacy in dose-response studies in adults.
Extended release: Quedexy XR, Trokendi XR: Initial: 25 to 50 mg once daily for 1 week; increase at weekly intervals by 25 to 50 mg/day once daily; titrate dose to response; longer intervals between dosage adjustment may be used; usual maintenance dose: 200 to 400 mg once daily; maximum daily dose: 1600 mg/day; higher doses have not been studied
Primary generalized tonic-clonic seizures:
Immediate release: Initial: 25 to 50 mg/day once daily for 1 week; increase over 8 weeks in increments of 25 to 50 mg/day in 2 divided doses; titrate dose to response; usual maintenance dose: 200 mg twice daily; use slower initial titration rate (>2 week intervals); maximum daily dose: 1600 mg/day; Note: Doses above 400 mg/day have not been shown to increase efficacy in dose-response studies in adults.
Extended release: Qudexy XR, Trokendi XR: Initial: 25 mg to 50 mg once daily for 1 week; increase at weekly intervals by 25 to 50 mg/day increments once daily; titrate dose to response; usual maintenance dose: 400 mg once daily; maximum daily dose: 1600 mg/day; higher doses have not been studied
Anticonvulsant, monotherapy: Partial onset seizures or primary generalized tonic-clonic seizures: Oral:
Immediate release:
Children 2 to <10 years: Initial: 25 mg once daily (in evening); may increase if tolerated to 25 mg twice daily in week 2; thereafter, may increase by 25 to 50 mg/day at weekly intervals over 5 to 7 weeks up to the lower end of the target daily maintenance dosing range (ie, to the minimum recommended maintenance dose); if additional seizure control is needed and therapy is tolerated, may further increase by 25 to 50 mg/day at weekly intervals up to the upper end of the target daily maintenance dosing range (ie, to the maximum recommended maintenance dose):
Target daily maintenance dosing range:
≤11 kg: 150 to 250 mg/day in 2 divided doses
12 to 22 kg: 200 to 300 mg/day in 2 divided doses
23 to 31 kg: 200 to 350 mg/day in 2 divided doses
32 to 38 kg: 250 to 350 mg/day in 2 divided doses
>38 kg: 250 to 400 mg/day in 2 divided doses
Children ≥10 years and Adolescents: Initial: 25 mg twice daily; increase at weekly intervals by 50 mg/day increments up to a dose of 100 mg twice daily (week 4 dose); thereafter, may further increase at weekly intervals by 100 mg/day increments up to the recommended maximum dose of 200 mg twice daily
Extended release: Qudexy XR, Trokendi XR: Children ≥10 years and Adolescents: Initial: 50 mg once daily for 1 week; increase at weekly intervals by 50 mg/day increments up to a dose of 200 mg once daily (week 4 dose); thereafter, may increase at weekly intervals by 100 mg/day increments up to the recommended dose of 400 mg once daily
Migraine prophylaxis: Oral:
Children 6 to <12 years; weight: ≥20 kg: Limited data available: Immediate release: Initial: 15 mg once daily for 1 week; then increase to 15 mg twice daily for 1 week; then increase to 25 mg twice daily for 7 days; continue to gradually titrate to effect up to target dose of 2 to 3 mg/kg/day divided twice daily; maximum daily dose: 200 mg/day; dosing based on a double-randomized, placebo-controlled trial of 90 pediatric patients <12 years (treatment arm: n=59; mean age: 11.3 years as part of a larger trial with a total of 108 pediatric patients receiving topiramate compared to 49 receiving placebo) which showed a mean reduction in migraine days/month with topiramate and significantly more topiramate patients experienced ≥75% reduction in mean monthly migraine days compared to placebo (32% vs 14%) for overall study population; mean maintenance dose: 2 mg/kg/day; treatment duration of maintenance dose: 12 weeks (Winner, 2005)
Children ≥12 years and Adolescents: Initial: 25 mg/day once daily at night for 1 week; increase at weekly intervals in 25 mg/day increments as tolerated and indicated to recommended dose of 50 mg twice daily; in a double-blind, placebo-controlled, dose-finding trial of 103 pediatric patients ≥12 years (mean age: 14.2 years), the daily dose of 100 mg/day was shown to significantly decrease frequency of migraine attacks compared to a lower dose of 50 mg/day (Lewis, 2009)
Extemporaneously Prepared
20 mg/mL Oral Suspension (ASHP Standard Concentration) (ASHP 2017)
A 20 mg/mL oral suspension may be made with topiramate tablets or powder, Ora-Plus and Ora-Sweet. Measure out 2,000 mg of topiramate (equivalent tablets or powder). If using tablets, crush in a mortar and reduce to a fine powder. Add 10 mL of Ora-Plus and mix to a uniform paste; mix while adding an additional 40 mL of Ora-Plus in incremental proportions. Add a small amount of Ora-Sweet and mix. Transfer to a calibrated, amber bottle; rinse mortar with Ora-Sweet and add sufficient quantity to make 100 mL. Label "shake well." Stable for 90 days refrigerated or at room temperature (Allen 2017).
Allen LV Jr. Contemporary compounding: topiramate 20 mg/mL oral suspension. U.S. Pharmacist. 2017;42(5):46-47.
Administration
Administer without regard to meals. Administer the immediate release formulation in divided doses. It is not recommended to crush, break, or chew immediate release tablets due to bitter taste. Swallow extended release (ER) and sprinkle capsules whole. Sprinkle capsules and Qudexy XR capsules may also be opened to sprinkle the entire contents on a small amount (~1 teaspoon) of soft food; swallow immediately and do not chew. Do not store drug/food mixture for future use. Do not sprinkle Trokendi XR capsules on food, chew, or crush. Avoid alcohol use with Trokendi XR capsules within 6 hours prior to and 6 hours after administration.
Storage
Extended release capsules: Store at 15°C to 30°C (59°F to 86°F). Protect from moisture. Protect from light.
Sprinkle capsules: Store at or below 25°C (77°F). Protect from moisture.
Tablets: Store at 15°C to 30°C (59°F to 86°F). Protect from moisture.
Topiramate Images
Drug Interactions
Alcohol (Ethyl): May enhance the CNS depressant effect of Topiramate. Alcohol (Ethyl) may increase the serum concentration of Topiramate. This applies specifically to use with the extended-release topiramate capsules (Trokendi XR). Also, topiramate concentrations may be subtherapeutic in the later portion of the dosage interval. Management: Concurrent use of alcohol within 6 hours of ingestion of extended-release topiramate (Trokendi XR) is contraindicated. Any use of alcohol with topiramate should be avoided when possible and should only be undertaken with extreme caution. Avoid combination
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Alpha-/Beta-Agonists (Indirect-Acting): Carbonic Anhydrase Inhibitors may increase the serum concentration of Alpha-/Beta-Agonists (Indirect-Acting). Monitor therapy
Amantadine: Carbonic Anhydrase Inhibitors may increase the serum concentration of Amantadine. Monitor therapy
Amitriptyline: Topiramate may enhance the CNS depressant effect of Amitriptyline. Topiramate may increase serum concentrations of the active metabolite(s) of Amitriptyline. Topiramate may increase the serum concentration of Amitriptyline. Monitor therapy
Amphetamines: Carbonic Anhydrase Inhibitors may decrease the excretion of Amphetamines. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of Topiramate. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
CarBAMazepine: May decrease the serum concentration of Topiramate. Consider therapy modification
Carbonic Anhydrase Inhibitors: May enhance the adverse/toxic effect of other Carbonic Anhydrase Inhibitors. The development of acid-base disorders with concurrent use of ophthalmic and oral carbonic anhydrase inhibitors has been reported. Management: Avoid concurrent use of different carbonic anhydrase inhibitors if possible. Monitor patients closely for the occurrence of kidney stones and with regards to severity of metabolic acidosis. Avoid combination
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Estrogen Derivatives (Contraceptive): Topiramate may decrease the serum concentration of Estrogen Derivatives (Contraceptive). Contraceptive failure is possible. Management: Risk appears greatest for higher topiramate doses (200 mg/day or greater). Some have recommended using at least 50 mcg/day of ethinyl estradiol, but the effectiveness of this is unclear. Consider a nonhormonal form of contraception. Consider therapy modification
Flecainide: Carbonic Anhydrase Inhibitors may increase the serum concentration of Flecainide. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosphenytoin: May decrease the serum concentration of Topiramate. Topiramate may increase the serum concentration of Fosphenytoin. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lacosamide: Antiepileptic Agents (Sodium Channel Blockers) may enhance the adverse/toxic effect of Lacosamide. Specifically the risk for bradycardia, ventricular tachyarrhythmias, or a prolonged PR interval may be increased. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lithium: Topiramate may increase the serum concentration of Lithium. Monitor therapy
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Loop Diuretics: May enhance the hypokalemic effect of Topiramate. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Memantine: Carbonic Anhydrase Inhibitors may increase the serum concentration of Memantine. Monitor therapy
MetFORMIN: Topiramate may enhance the adverse/toxic effect of MetFORMIN. Monitor therapy
Methenamine: Carbonic Anhydrase Inhibitors may diminish the therapeutic effect of Methenamine. Management: Consider avoiding this combination. Monitor for decreased therapeutic effects of methenamine if used concomitant with a carbonic anhydrase inhibitor. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May diminish the therapeutic effect of Anticonvulsants. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Phenytoin: Topiramate may increase the serum concentration of Phenytoin. Phenytoin may decrease the serum concentration of Topiramate. Monitor therapy
Pioglitazone: Topiramate may decrease the serum concentration of Pioglitazone. Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Primidone: Carbonic Anhydrase Inhibitors may enhance the adverse/toxic effect of Primidone. Specifically, osteomalacia and rickets. Carbonic Anhydrase Inhibitors may decrease the serum concentration of Primidone. Monitor therapy
Progestins (Contraceptive): Topiramate may decrease the serum concentration of Progestins (Contraceptive). Management: Caution patients that this combination may be associated with reduced contraceptive effectiveness. Consider adding an additional (non-hormonal) contraceptive method. Consider therapy modification
QuiNIDine: Carbonic Anhydrase Inhibitors may decrease the excretion of QuiNIDine. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Salicylates: May enhance the adverse/toxic effect of Carbonic Anhydrase Inhibitors. Salicylate toxicity might be enhanced by this same combination. Management: Avoid these combinations when possible.Dichlorphenamide use with high-dose aspirin as contraindicated. If another combination is used, monitor patients closely for adverse effects. Tachypnea, anorexia, lethargy, and coma have been reported. Consider therapy modification
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Thiazide and Thiazide-Like Diuretics: May enhance the hypokalemic effect of Topiramate. Thiazide and Thiazide-Like Diuretics may increase the serum concentration of Topiramate. Management: Monitor for increased topiramate levels/adverse effects (e.g., hypokalemia) with initiation/dose increase of a thiazide diuretic. Closely monitor serum potassium concentrations with concomitant therapy. Topiramate dose reductions may be necessary. Consider therapy modification
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Ulipristal: Topiramate may decrease the serum concentration of Ulipristal. Avoid combination
Valproate Products: Topiramate may enhance the adverse/toxic effect of Valproate Products. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Adverse Reactions
Adverse events are reported for adult and pediatric patients for various indications and regimens. A wide range of dosages were studied. Incidence of adverse events was frequently lower in the pediatric population studied.
>10%:
Central nervous system: Paresthesia (adolescents and adults: 19% to 51%; children and adolescents: 3% to 12%), fatigue (8% to 15%), drowsiness (adolescents and adults: 6% to 15%), dizziness (adolescents and adults: 6% to 14%), memory impairment (1% to 11%)
Endocrine & metabolic: Decreased serum bicarbonate (adolescents and adults: 14% to 77%; children and adolescents: 9% to 25%; >5 mEq/L to <17 mEq/L: 1% to 11%), hyperammonemia (adolescents: 14% to 26%; ≥50% above ULN [adolescents]: 9%), weight loss (4% to 17%)
Gastrointestinal: Abdominal pain (adolescents and adults: 6% to 15%), anorexia (adolescents and adults: 4% to 15%), dysgeusia (adolescents and adults: 3% to 15%), nausea (adolescents and adults: 8% to 13%), diarrhea (2% to 11%)
Respiratory: Upper respiratory tract infection (13% to 26%)
Miscellaneous: Fever (1% to 12%)
1% to 10%:
Cardiovascular: Flushing (children and adolescents: ≤5%), chest pain (adults: 1% to 2%)
Central nervous system: Disturbance in attention (≤10%), lack of concentration (≤10%), depression (adults: 7% to 9%; children and adolescents: ≤3%), insomnia (adolescents and adults: 6% to 9%), mood disorder (1% to 8%), hypoesthesia (adolescents and adults 4% to 7%), anxiety (adolescents and adults: 4% to 6%), cognitive dysfunction (1% to 6%), psychomotor impairment (adolescents and adults: 2% to 5%), headache (children and adolescents: 4%), nervousness (adolescents and adults: 4%), ataxia (adolescents and adults: 1% to 4%), behavioral problems (children and adolescents: ≤3%), confusion (≤3%), hypertonia (adults: ≤3%), vertigo (children and adolescents: ≤3%), agitation (adolescents and adults: 2%), exacerbation of depression (adolescents and adults: 2%), speech disturbance (adolescents and adults: 1%)
Dermatologic: Alopecia (1% to 4%), pruritus (adolescents and adults: 1% to 4%), skin rash (1% to 4%), acne vulgaris (adults: 2% to 3%)
Endocrine & metabolic: Menstrual disease (adolescents and adults: 3%), intermenstrual bleeding (children and adolescents: ≤3%), increased gamma-glutamyl transferase (adults: 1% to 3%), increased thirst (adolescents and adults: 2%)
Gastrointestinal: Dyspepsia (adolescents and adults: 4% to 5%), constipation (adolescents and adults: 1% to 4%), gastroenteritis (adolescents and adults: 3%), gastritis (adults: ≤3%), xerostomia (adolescents and adults: 1% to 3%), gastroesophageal reflux disease (adults: 1% to 2%), ageusia (adolescents and adults: 1%)
Genitourinary: Urinary tract infection (adolescents and adults: 1% to 4%), premature ejaculation (adolescents and adults: 3%), decreased libido (adults: ≤3%), urinary frequency (≤3%), vaginal hemorrhage (adults: ≤3%), cystitis (adults: 1% to 3%), urinary incontinence (children and adolescents: 1% to 3%), dysuria (adults: ≤2%)
Hematologic & oncologic: Hemorrhage (4% to 5%), anemia (children and adolescents: 1% to 3%), neoplasm (adolescents and adults: 2%)
Hypersensitivity: Hypersensitivity reaction (adolescents and adults: 2% to 4%)
Infection: Viral infection (3% to 8%), infection (2% to 8%)
Neuromuscular & skeletal: Arthralgia (adolescents and adults: 3% to 7%), asthenia (≤6%), muscle spasm (≤3%), lower extremity pain (adolescents and adults: 2% to 3%)
Ophthalmic: Conjunctivitis (adolescents and adults: 2% to 7%), blurred vision (adolescents and adults: 4%), visual disturbance (adolescents and adults: 1% to 2%)
Otic: Otitis media (adolescents and adults: 1% to 2%)
Renal: Nephrolithiasis (adolescents and adults: ≤3%)
Respiratory: Sinusitis (1% to 10%), cough (adolescents and adults: 2% to 7%), rhinitis (2% to 7%), pharyngitis (adolescents and adults: 5% to 6%), bronchitis (1% to 5%), epistaxis (children and adolescents: ≤4%), dyspnea (adolescents and adults: 1% to 3%)
Miscellaneous: Accidental injury (adolescents and adults: 9%), language problems (adolescents and adults: 6% to 7%)
Frequency not defined:
Cardiovascular: Hypotension, orthostatic hypotension, syncope
Central nervous system: Suicidal ideation, suicidal tendencies
Endocrine & metabolic: Hyperchloremia, increased serum total protein, increased uric acid
Gastrointestinal: Gingival hemorrhage, hematuria
Hematologic & oncologic: Abnormal serum phosphorus level (decreased), decreased neutrophils, decreased white blood cell count, eosinophilia, quantitative disorders of platelets (increased)
Hepatic: Increased serum alkaline phosphatase
Neuromuscular & skeletal: Myalgia
Ophthalmic: Myopia, scotoma, visual field defect
Renal: Increased blood urea nitrogen, increased serum creatinine
<1%, postmarketing, and/or case reports: Acute myopia with secondary angle-closure glaucoma, bullous rash, calcium nephrolithiasis, erythema multiforme, hepatic failure, hepatitis, hyperammonemic encephalopathy, hyperchloremic metabolic acidosis (nonanion gap), hyperthermia, hypohidrosis, maculopathy, major hemorrhage (children), pancreatitis, pemphigus, Stevens-Johnson syndrome, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- CNS effects: Cognitive dysfunction (confusion, psychomotor slowing, difficulty with concentration/attention, difficulty with memory, speech or language problems), psychiatric disturbances (depression or mood disorders), and sedation (somnolence or fatigue) may occur with use; incidence may be related to rapid titration and higher doses; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving). May also cause paresthesia, dizziness, and ataxia.
- Hyperammonemia/encephalopathy: Hyperammonemia with or without encephalopathy may occur with monotherapy or in combination with valproic acid and has been documented in patients who have tolerated each drug alone; incidence may be dose-related. Risk may be increased in patients with inborn errors of metabolism or decreased hepatic mitochondrial activity. May be asymptomatic; monitor for lethargy, vomiting, or unexplained changes in mental status.
- Metabolic acidosis: May be associated with hyperchloremic nonanion gap metabolic acidosis due to inhibition of carbonic anhydrase and increased renal bicarbonate loss. Decreases in serum bicarbonate are relatively common (up to 67% of epilepsy patients and 77% of migraine patients) but usually mild-to-moderate (average decrease of 4 mEq/L at dose of 400 mg/day in adults and 6 mg/kg/day in children). However, risk may be increased in patients with a predisposing condition (renal, respiratory and/or hepatic impairment), diarrhea, ketogenic diet, status epilepticus, or concurrent treatment with other drugs which may cause acidosis. Metabolic acidosis may occur at dosages as low as 50 mg/day. Serum bicarbonate should be monitored, as well as potential complications of chronic acidosis (nephrolithiasis, nephrocalcinosis, osteomalacia/osteoporosis, and reduced growth rates and/or reduced weight in children). Dose reduction or discontinuation (by tapering dose) should be considered in patients with persistent or severe metabolic acidosis. If treatment is continued, alkali supplementation should be considered.
- Oligohidrosis/hyperthermia: May be associated with oligohidrosis and hyperthermia, most frequently in children; use caution and monitor closely during strenuous exercise, during exposure to high environmental temperature, or in patients receiving other carbonic anhydrase inhibitors and drugs with anticholinergic activity.
- Ophthalmic effects: Has been associated with acute myopia and secondary angle-closure glaucoma in adults and children, typically within 1 month of initiation; discontinue in patients with acute onset of decreased visual acuity and/or ocular pain.
- Renal calculus: Topiramate exhibits weak carbonic anhydrase inhibitory properties and may increase the risk of kidney stones about 2 to 4 times that of the untreated population. Kidney stones have been reported in children and adults (incidence higher in males). Consider avoiding use in patients on a ketogenic diet. The risk of kidney stones may be reduced by increasing fluid intake.
- Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; notify healthcare provider immediately if symptoms occur.
- Visual field defects: Has been reported independent of increased intraocular pressure; generally reversible upon discontinuation. Consider discontinuation if visual problems occur at any time during treatment.
Disease-related concerns:
- Depression: Use with caution in patients with depression or suicidal tendencies.
- Eating disorders: The exacerbation and development of eating disorders, including anorexia nervosa and bulimia, has been reported in case reports of adolescents receiving topiramate for migraines or chronic headaches and an adult receiving topiramate for epilepsy. Prior to initiation of topiramate screen for a history of eating disorder symptoms, eating disorder risk factors (eg, history of dieting behavior), cognitive symptoms of eating disorders (eg, weight or shape concerns, fear of gaining weight, drive for thinness), and any recent changes in social functioning including increased withdrawal or isolation. Inquire whether the patient has unrealistic or unhealthy weight goals. Evaluate exercise habits (eg, look for over-exercising or compulsive exercising above that of similarly athletic peers) and dietary intake; assess rigid patterns or avoidance of specific categories of foods and preoccupation with maintaining a “healthy diet” or experimentation with fad diets. In adolescents assess developmental weight history with growth curves. Monitor eating behaviors and weight closely in patients receiving topiramate who have eating disorder symptoms or risk factors (Lebow 2015; Rosenow 2002).
- Hepatic impairment: Use caution with hepatic impairment; clearance may be reduced. Dosage adjustment may be required.
- Renal impairment: Use caution with renal impairment; clearance may be reduced. Dosage adjustment may be required.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution; dosage adjustment may be necessary. Weight loss, cognitive impairment, sedation, and gait/balance disturbances may be more pronounced in the older adult cohort (Sommer 2010).
Other warnings/precautions:
- Withdrawal: Do not discontinue abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal. Doses were also gradually withdrawn in migraine prophylaxis studies (decreased in weekly intervals by 25-50 mg/day).
Monitoring Parameters
Seizure frequency, hydration status; electrolytes (recommended monitoring includes serum bicarbonate at baseline and periodically during treatment), serum creatinine; monitor for symptoms of acute acidosis and complications of long-term acidosis (nephrolithiasis, nephrocalcinosis, osteomalacia/osteoporosis, and reduced growth rates and/or weight in children); ammonia level in patients with unexplained lethargy, vomiting, or mental status changes; intraocular pressure, symptoms of secondary angle closure glaucoma; suicidality (eg, suicidal thoughts, depression, behavioral changes); weight and eating behaviors in patients with eating disorder symptoms or risk factors; sedation
Pregnancy
Pregnancy Considerations
Based on limited data (n=5), topiramate was found to cross the placenta and could be detected in neonatal serum (Ohman 2002).
Topiramate may cause fetal harm if administered to a pregnant woman. An increased risk of oral clefts (cleft lip and/or palate) and for being small for gestational age (SGA) has been observed following in utero exposure. Data from the North American Antiepileptic Drug (NAAED) Pregnancy Registry reported that the prevalence of oral clefts was 1.1% for infants exposed to topiramate during the first trimester of pregnancy, versus 0.36% for infants exposed to a reference antiepileptic drug, and 0.12% for infants with no exposure born to mothers without epilepsy; the relative risk of oral clefts in infants exposed to topiramate was calculated to be 9.6 (95% CI: 4 to 23). Data from the NAAED Pregnancy Registry reported that the prevalence of small for gestational age newborns was 19.7% for newborns exposed to topiramate in utero, versus 7.9% for newborns exposed to a reference antiepileptic drug, and 5.4% for newborns with no exposure born to mothers without epilepsy. Although not evaluated during pregnancy, metabolic acidosis may be induced by topiramate. Metabolic acidosis during pregnancy may result in adverse effects and fetal death. Pregnant women and their newborns should be monitored for metabolic acidosis. In general, maternal polytherapy with antiepileptic drugs may increase the risk of congenital malformations; monotherapy with the lowest effective dose is recommended. Newborns of women taking antiepileptic medications may be at an increased risk of a 1 minute Apgar score <7 (Harden 2009).
Maternal serum concentrations may decrease during the second and third trimesters of pregnancy; therefore, therapeutic drug monitoring should be considered during pregnancy and postpartum in patients who require therapy (Ohman 2009; Westin 2009).
Effective contraception should be used in females of reproductive potential who are not planning a pregnancy; consider use of alternative medications in women who wish to become pregnant.
Data collection to monitor pregnancy and infant outcomes following exposure to topiramate is ongoing. Patients may enroll themselves into the NAAED Pregnancy Registry by calling 1-888-233-2334. Additional information is available at www.aedpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used to treat seizures.
- It is used to prevent migraine headaches.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Weight loss
- Change in taste
- Diarrhea
- Anxiety
- Fatigue
- Loss of strength and energy
- Common cold symptoms
- Joint pain
- Headache
- Dry mouth
- Flushing
- Hair loss
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Acidosis like confusion, fast breathing, fast heartbeat, abnormal heartbeat, severe abdominal pain, nausea, vomiting, fatigue, shortness of breath, or loss of strength and energy.
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- High ammonia levels like abnormal heartbeat, abnormal breathing, confusion, pale skin, slow heartbeat, seizures, sweating, vomiting, or twitching.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Kidney stone like back pain, abdominal pain, or blood in the urine.
- Confusion
- Difficulty focusing
- Change in balance
- Severe dizziness
- Passing out
- Inability to eat
- Unable to pass urine
- Seizures
- Burning or numbness feeling
- Bone pain
- Chest pain
- Trouble with memory
- Muscle pain
- Muscle weakness
- Difficulty speaking
- Trouble sleeping
- Tremors
- Abnormal gait
- Involuntary eye movements
- Agitation
- Irritability
- Panic attacks
- Mood changes
- Blurred vision
- Eye redness
- Vision changes
- Eye pain
- Eye irritation
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.