Boxed Warning
Permanent vision loss:
Vigabatrin can cause permanent bilateral concentric visual field constriction, including tunnel vision that can result in disability. In some cases, vigabatrin also can damage the central retina and may decrease visual acuity.
The onset of vision loss from vigabatrin is unpredictable and can occur within weeks of starting treatment or sooner, or at any time after starting treatment, even after months or years.
Symptoms of vision loss from vigabatrin are unlikely to be recognized by the patients or caregivers before vision loss is severe. Vision loss of milder severity, while often unrecognized by the patient or caregiver, can still adversely affect function.
The risk of vision loss increases with increasing dose and cumulative exposure, but there is no dose or exposure known to be free of risk of vision loss.
Vision assessment is recommended at baseline (no later than 4 weeks after starting vigabatrin), at least every 3 months during therapy, and about 3 to 6 months after the discontinuation of therapy. Once detected, vision loss caused by vigabatrin is not reversible. It is expected that, even with frequent monitoring, some patients will develop severe vision loss.
Consider drug discontinuation, balancing benefit and risk, if vision loss is documented.
Risk of new or worsening vision loss continues as long as vigabatrin is used. It is possible that vision loss can worsen despite discontinuation of vigabatrin.
Because of the risk of vision loss, vigabatrin should be withdrawn from patients with refractory complex partial seizures who fail to show substantial clinical benefit within 3 months of initiation and within 2 to 4 weeks of initiation for patients with infantile spasms, or sooner if treatment failure becomes obvious. Patient response to and continued need for vigabatrin should be periodically reassessed.
Vigabatrin should not be used in patients with, or at high risk of, other types of irreversible vision loss unless the benefits of treatment clearly outweigh the risks.
Vigabatrin should not be used with other drugs associated with serious adverse ophthalmic effects such as retinopathy or glaucoma unless the benefits clearly outweigh the risks.
Use the lowest dosage and shortest exposure to vigabatrin that is consistent with clinical objectives.
Because of the risk of permanent vision loss, vigabatrin is available only through a restricted program under a risk evaluation and mitigation strategy (REMS) called the Vigabatrin REMS program. Further information is available at http://www.vigabatrinREMS.com or by calling 1-866-244-8175.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Packet, Oral:
Sabril: 500 mg (50 ea)
Vigadrone: 500 mg (1 ea, 50 ea)
Generic: 500 mg (1 ea, 50 ea)
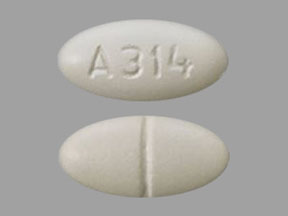
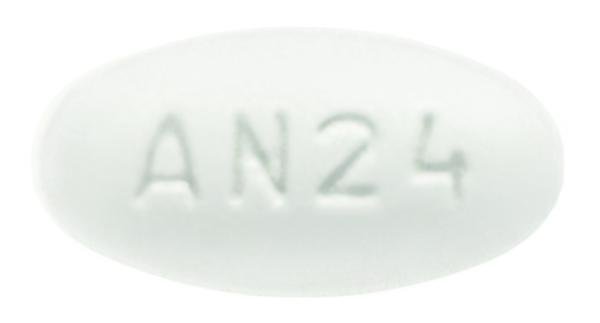
Tablet, Oral:
Sabril: 500 mg [scored]
Generic: 500 mg
Pharmacology
Mechanism of Action
Irreversibly inhibits gamma-aminobutyric acid transaminase (GABA-T), increasing the levels of the inhibitory compound gamma amino butyric acid (GABA) within the brain. Duration of effect is dependent upon rate of GABA-T resynthesis.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid, complete
Distribution
Vd: 1.1 L/kg
Metabolism
Insignificant
Excretion
Urine (80% as unchanged drug).
Clearance:
Pediatric patients: 5 months to 2 years: 2.4 L/hour; 3 to 9 years: 5.1 L/hour; 10 to 16 years: 5.8 L/hour.
Adults: 7 L/hour.
Time to Peak
Infants and Children 5 months to 2 years: 2.5 hours; Children and Adolescents 3 to 16 years and Adults: 1 hour (2 hours with food).
Duration of Action
Resynthesis of GABA-T dependent: Variable (not strictly correlated to serum concentrations)
Half-Life Elimination
Terminal: Prolonged in renal impairment.
Pediatric patients:
5 months to 2 years: ~5.7 hours.
3 to 9 years: ~6.8 hours.
10 to 16 years: ~9.5 hours.
Adult patients: ~10.5 hours.
Protein Binding
Does not bind to plasma proteins
Use in Specific Populations
Special Populations: Renal Function Impairment
AUC increased 30% and half-life increased 55% in patients with mild renal impairment (CrCl >50 to 80 mL/minute). AUC and half-life increased twofold in patients with moderate renal impairment (CrCl >30 to 50 mL/minute). In patients with severe renal impairment (CrCl >10 to 30 mL/minute), AUC increased 4.5-fold and half-life increased 3.5-fold.
Special Populations: Elderly
Renal clearance was 36% lower in elderly patients compared with younger patients.
Special Populations: Race
Renal clearance was 25% higher in white patients compared with Japanese patients.
Use: Labeled Indications
Infantile spasms: As monotherapy for pediatric patients 1 month to 2 years of age with infantile spasms for whom the potential benefits outweigh the potential risk of vision loss.
Refractory complex partial seizures: As adjunctive therapy for adults and pediatric patients ≥2 years of age with refractory complex partial seizures who have inadequately responded to several alternative treatments and for whom the potential benefits outweigh the risk of vision loss.
Contraindications
There are no contraindications listed in the manufacturer’s labeling.
Canadian labeling: Hypersensitivity to vigabatrin or any component of the formulation; pregnancy; breastfeeding
Dosage and Administration
Dosing: Adult
Refractory complex partial seizures: Oral: Initial: 500 mg twice daily; increase daily dose by 500 mg increments at weekly intervals based on response and tolerability. Recommended dose: 1.5 g twice daily. Note: To taper, decrease dose by 1 g daily on a weekly basis. Withdraw therapy if a substantial clinical benefit is not observed within 3 months of treatment initiation; discontinue therapy if evidence of treatment failure becomes obvious earlier than 3 months.
Dosing: Geriatric
Refractory complex partial seizures: Refer to adult dosing. Initiate at low end of dosage range; monitor closely for sedation and confusion.
Dosing: Pediatric
Note: Use the lowest effective and shortest exposure consistent with therapeutic objectives.
Infantile spasms: Infants and Children 1 month to 2 years of age: Oral: Powder for oral solution: Initial: 50 mg/kg/day divided twice daily; may titrate upwards by 25 to 50 mg/kg/day increments every 3 days based on response and tolerability; maximum daily dose: 150 mg/kg/day divided twice daily; Note: To taper, decrease dose by 25 to 50 mg/kg/day every 3 to 4 days. Withdraw therapy in 2 to 4 weeks if a substantial clinical benefit is not observed or discontinue treatment if evidence of treatment failure becomes obvious earlier than 2 to 4 weeks.
Refractory complex partial seizures; adjunctive treatment: Note: Dose dependent upon weight and/or age. Withdraw therapy if a substantial clinical benefit is not observed within 3 months of treatment initiation; discontinue therapy if evidence of treatment failure becomes obvious earlier than 3 months.
Fixed dosing: Children ≥10 years and Adolescents: Oral:
Patient weight 25 to 60 kg and age 10 to 16 years: Initial: 250 mg twice daily; increase daily dose in 500 mg increments at weekly intervals based on response and tolerability. Recommended maintenance dose: 1,000 mg twice daily; Note: To taper, decrease daily dose by one-third every week for 3 weeks.
Patient weight >60 kg (regardless of age), or age >16 years (regardless of weight): Initial: 500 mg twice daily; increase daily dose in 500 mg increments at weekly intervals based on response and tolerability. Recommended dose: 1,500 mg twice daily. Note: To taper, decrease dose by 1,000 mg daily on a weekly basis.
Weight-band dosing: Limited data available (Camposano 2008; Coppola 2004; Sabril prescribing information [Canada] 2018; Willmore 2009): Children ≥2 years and weighing ≥10 kg and Adolescents ≤16 years:
Initial: Oral: 40 mg/kg/day divided twice daily; maintenance dosages based on patient weight
Maintenance: Oral:
10 to 15 kg: 500 to 1,000 mg/day divided twice daily
16 to 30 kg: 1,000 to 1,500 mg/day divided twice daily
31 to 50 kg: 1,500 to 3,000 mg/day divided twice daily
>50 kg: 2,000 to 3,000 mg/day divided twice daily
Reconstitution
Powder for oral solution: Dissolve each 500 mg powder packet in 10 mL of cold or room temperature water to make a 50 mg/mL solution. Alternatively, the powder may be dissolved with 10 mL of fruit juice, milk, or infant formula (Sabril Canadian product monograph). After reconstitution, use immediately; discard any unused portion or if the resulting solution is not free of particles or colorless.
Administration
Administer without regard to meals.
Oral solution: Mix with water immediately prior to administration. Use a calibrated measuring device to measure dose (household teaspoon or tablespoon is not an adequate measuring device).
Storage
Store at 20°C to 25°C (68°F to 77°F).
Vigabatrin Images
Drug Interactions
Alcohol (Ethyl): CNS Depressants may enhance the CNS depressant effect of Alcohol (Ethyl). Monitor therapy
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Brexanolone: CNS Depressants may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
ClonazePAM: Vigabatrin may enhance the CNS depressant effect of ClonazePAM. Vigabatrin may increase the serum concentration of ClonazePAM. Monitor therapy
CNS Depressants: May enhance the adverse/toxic effect of other CNS Depressants. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Doxylamine: May enhance the CNS depressant effect of CNS Depressants. Management: The manufacturer of Diclegis (doxylamine/pyridoxine), intended for use in pregnancy, specifically states that use with other CNS depressants is not recommended. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Esketamine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosphenytoin: Vigabatrin may decrease the serum concentration of Fosphenytoin. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
HydrOXYzine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mefloquine: May diminish the therapeutic effect of Anticonvulsants. Mefloquine may decrease the serum concentration of Anticonvulsants. Management: Mefloquine is contraindicated for malaria prophylaxis in persons with a history of convulsions. Monitor anticonvulsant concentrations and treatment response closely with concurrent use. Consider therapy modification
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Mianserin: May diminish the therapeutic effect of Anticonvulsants. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Opioid Agonists: CNS Depressants may enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Orlistat: May decrease the serum concentration of Anticonvulsants. Monitor therapy
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Phenytoin: Vigabatrin may decrease the serum concentration of Phenytoin. Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Trimeprazine: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
Vigabatrin has been reported to decrease AST and ALT activity in the plasma in up to 90% of patients, causing the enzymes to become undetectable in some patients; this may preclude use of AST and ALT as markers for hepatic injury. Vigabatrin may increase amino acids in the urine leading to false-positive tests for rare genetic metabolic disorders
Adverse Reactions
>10%:
Central nervous system: Drowsiness (infants: 17% to 45%; adults: 22% to 24%; children and adolescents: 6%), headache (adults: 33%), fatigue (adults: 23% to 28%; children and adolescents: 10%), dizziness (adults: 24%), irritability (infants: 16% to 23%), sedated state (infants: 17% to 19%; adults: 4%), insomnia (infants: 10% to 12%)
Dermatologic: Skin rash (infants: 8% to 11%)
Endocrine & metabolic: Weight gain (children and adolescents: 47%; adults: 6% to 17%)
Gastrointestinal: Vomiting (infants: 14% to 20%; adults: 7%), constipation (infants: 12% to 14%; adults: 8%), diarrhea (10% to 13%)
Infection: Viral infection (infants: 19% to 20%)
Neuromuscular & skeletal: Tremor (adults: 15%)
Ophthalmic: Visual field loss (adults: ≥30%), blurred vision (13%), nystagmus disorder (adults: 13%)
Otic: Otitis media (infants: 10% to 44%), otic infection (infants: 7% to 14%)
Respiratory: Upper respiratory tract infection (infants: 46% to 51%; adults: 7%), bronchitis (infants: 30%), nasopharyngitis (adults: 14%), pneumonia (infants: 11% to 13%), nasal congestion (infants: 4% to 13%)
Miscellaneous: Fever (infants: 19% to 29%; adults: 4%)
1% to 10%:
Cardiovascular: Peripheral edema (adults: 2% to 5%), edema (adults: 1%)
Central nervous system: Disturbance in attention (adults: 9%), ataxia (adults: 7%), memory impairment (adults: 7%), paresthesia (adults: 7%), lethargy (4% to 7%), seizure (infants: 4% to 7%), depression (adults: 6%), hypotonia (infants: 4% to 6%), status epilepticus (infants: 4% to 6%; adults: 2%), abnormal sensory symptoms (adults: 4%), anxiety (adults: 4%), confusion (adults: 4%), hyperreflexia (adults: 4%), hypoesthesia (adults: 4%), hyporeflexia (adults: 4%), abnormal behavior (adults: 3%), abnormality in thinking (adults: 3%), dysarthria (adults: 2%), impaired consciousness (adults: 2%), vertigo (adults: 2%), peripheral neuropathy (adults: 1%)
Endocrine & metabolic: Increased thirst (adults: 2%)
Gastrointestinal: Nausea (adults: 10%), decreased appetite (infants: 7% to 9%), viral gastroenteritis (infants: 5% to 6%), upper abdominal pain (adults: 5%), dyspepsia (adults: 4%), stomach discomfort (adults: 4%), abdominal pain (adults: 3%), abdominal distention (adults: 2%)
Genitourinary: Dysmenorrhea (adults: 9%), urinary tract infection (adults: 4%)
Hematologic & oncologic: Anemia (adults: 6%), bruise (adults: 3%), decreased hemoglobin (adults: 3%)
Infection: Candidiasis (infants: 3% to 8%), influenza (3% to 5%)
Neuromuscular & skeletal: Arthralgia (adults: 10%), limb pain (adults: 6%), asthenia (adults: 5%), back pain (adults: 4%), muscle spasm (adults: 3%), myalgia (adults: 3%)
Ophthalmic: Diplopia (adults: 7%), strabismus (infants: 5%), conjunctivitis (infants: 2% to 5%), asthenopia (adults: 2%)
Otic: Tinnitus (adults: 2%)
Respiratory: Sinusitis (infants: 5% to 9%), cough (infants: 3% to 8%), pharyngolaryngeal pain (adults: 7%), sinus headache (adults: 6%), croup (infants: 1% to 5%)
Frequency not defined:
Central nervous system: Suicidal ideation, suicidal tendencies
Ophthalmic: Decreased visual acuity, permanent vision loss, tunnel vision, visual field defect (bilateral concentric visual field constriction; may be permanent)
<1%, postmarketing, and/or case reports: Acute psychosis, agitation (neonates), alopecia, angioedema, apathy, cerebral edema (infants: intramyelinic), cholestasis, deafness, delirium, developmental delay, dyskinesia, dystonia, encephalopathy, esophagitis, facial edema, gastrointestinal hemorrhage, hypertonia, hypomania, laryngeal edema, maculopapular rash, malignant hyperthermia, multiorgan failure, muscle spasticity, myoclonus, optic neuritis, pruritus, psychosis, pulmonary embolism, respiratory failure, sexual disorder (delayed puberty), Stevens-Johnson syndrome, stridor, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- Anemia: Use has been associated with decreased hemoglobin and hematocrit; cases of significantly reduced hemoglobin (<8 g/dL) and/or hematocrit (<24%) have been reported.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Edema: Peripheral edema and edema independent of hypertension, heart failure, weight gain, renal or hepatic dysfunction has been reported.
- Neurotoxicity: Intramyelinic edema has been reported (rarely) in infants. Patients must be closely monitored for potential neurotoxicity (observed in animal models but not established in adults).
- Peripheral neuropathy: Peripheral neuropathy manifesting as numbness or tingling in the toes or feet, reduced distal lower limb vibration or position sensation, or progressive loss of reflexes, starting at the ankles, has been reported in adult patients.
- Suicidal ideation: Pooled analysis of trials involving various antiepileptics (regardless of indication) showed an increased risk of suicidal thoughts/behavior (incidence rate: 0.43% treated patients compared to 0.24% of patients receiving placebo); risk observed as early as 1 week after initiation and continued through duration of trials (most trials ≤24 weeks). Monitor all patients for notable changes in behavior that might indicate suicidal thoughts or depression; notify healthcare provider immediately if symptoms occur.
- Vision loss: [US Boxed Warning]: Vigabatrin can cause permanent vision loss in infants, children, and adults. Due to the risk of vision loss and because vigabatrin provides an observable symptomatic benefit when it is effective, the patient who fails to show substantial clinical benefit within a short period of time after initiation of treatment (2 to 4 weeks for infantile spasms; <3 months for refractory complex partial seizures), should be withdrawn from therapy. If in the clinical judgment of the prescriber evidence of treatment failure becomes obvious earlier in treatment, vigabatrin should be discontinued at that time. Patient response to and continued need for treatment should be periodically assessed. The onset of vision loss is unpredictable, and can occur within weeks of starting treatment or sooner, or at any time during treatment, even after months or years. The risk of vision loss increases with increasing dose and cumulative exposure, but there is no dose or exposure known to be free of risk of vision loss. It is possible that vision loss can worsen despite discontinuation. Assessment of vision loss is difficult in children and the frequency and extent of vision loss in infants and children is poorly characterized. Most data are available in adult patients. Vigabatrin causes permanent bilateral concentric visual field constriction in >30% of patients ranging in severity from mild to severe, including tunnel vision to within 10 degrees of visual fixation, and can result in disability. In some cases, vigabatrin can damage the central retina and may decrease visual acuity. Symptoms of vision loss are unlikely to be recognized by the patient or caregiver before loss is severe. Vision loss of milder severity, although potentially unrecognized by the patient or caregiver, may still adversely affect function. Vision should be assessed to the extent possible at baseline (no later than 4 weeks after initiation), at least every 3 months during therapy and at 3 to 6 months after discontinuation. Once detected, vision loss is not reversible; even with frequent monitoring, it is expected that some patients will develop severe vision loss. In patients who cannot be tested, treatment may continue according to clinical judgement, with appropriate patient counseling. Vigabatrin should not be used in patients with, or at high risk of, other types of irreversible vision loss unless the benefits of treatment clearly outweigh the risks. The interaction of other types of irreversible vision damage with vision damage from vigabatrin has not been well-characterized, but is likely adverse. Vigabatrin should not be used with other drugs associated with serious adverse ophthalmic effects such as retinopathy or glaucoma unless the benefits clearly outweigh the risks. The lowest dose and shortest exposure should be used that is consistent with clinical objectives. The possibility that vision loss from vigabatrin may be more common, more severe or have more severe functional consequences in infants and children than in adults cannot be excluded.
- Weight gain: Use has been associated with an average weight gain of 3.5 kg in adults and ≥7% of baseline body weight in pediatric patients.
Disease-related concerns:
- Psychiatric behavior: Use with caution in patients with a history of psychosis (psychotic/agitated reactions may occur more frequently), depression, or behavioral problems.
- Renal impairment: Use with caution in patients with renal impairment; modify dose in children and adults with renal impairment (CrCl <80 mL/minute).
- Seizures: May cause an increase in seizure frequency in some patients; use with particular caution in patients with myoclonic seizures, which may be more prone to this effect.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in the elderly as moderate to severe sedation and confusion have been reported; consider dose and/or frequency adjustments as renal clearance may be decreased.
Other warnings/precautions:
- Appropriate use: Vigabatrin is not indicated as a first-line agent for complex partial seizures.
- MRI abnormalities: Abnormal MRI changes have been reported in some infants and children ≤6 years of age. Resolution of MRI changes usually occurs with discontinuation of therapy. MRI changes were not seen in older children (>6 years of age) and adult patients.
- REMS program: [US Boxed Warning]: Because of the risk of permanent vision loss, vigabatrin is only available through a restricted distribution program under a Risk Evaluation and Mitigation Strategy (REMS) program. Under the Vigabatrin REMS program, only prescribers and pharmacies registered with the program are able to prescribe and distribute vigabatrin. Vigabatrin may only be dispensed to patients who are enrolled in and meet all conditions of the Vigabatrin REMS program. Call 866-244-8175 or visit http://www.vigabatrinREMS.com for further information.
- Withdrawal: Anticonvulsants should not be discontinued abruptly because of the possibility of increasing seizure frequency; therapy should be withdrawn gradually to minimize the potential of increased seizure frequency, unless safety concerns require a more rapid withdrawal.
Monitoring Parameters
Ophthalmologic examination by an ophthalmic professional with expertise in visual field interpretation and the ability to perform dilated indirect ophthalmoscopy of the retina at baseline (no later than 4 weeks after therapy initiation), periodically during therapy (every 3 months), and 3 to 6 months after discontinuation of therapy; assessment should include visual acuity and visual field whenever possible including mydriatic peripheral fundus examination and visual field perimetry, preferably by automated threshold visual field testing. Observe patient for excessive sedation, especially when instituting or increasing therapy; hemoglobin and hematocrit; suicidality (eg, suicidal thoughts, depression, behavioral changes); weight gain/edema
Pregnancy
Pregnancy Considerations
Vigabatrin crosses the placenta (Tran 1998).
Birth defects have been reported following use in pregnancy and include: cardiac defects, limb defects, male genital malformations, fetal anticonvulsant syndrome, renal and ear abnormalities. Time of exposure or maternal dosage was not reported and information is not available relating to the incidence or types of these outcomes in comparison to the general epilepsy population. Visual field examinations have been conducted following in utero exposure in a limited number of children tested at ≥6 years of age; no visual field loss was observed in 4 children and results were inconclusive in 2 others (Lawthom 2009; Sorri 2005).
Data collection to monitor pregnancy and infant outcomes following exposure to vigabatrin is ongoing. Healthcare providers are encouraged to enroll women exposed to vigabatrin during pregnancy in the North American Antiepileptic Drug (NAAED) Pregnancy Registry by calling 1-888-233-2334. Additional information is available at www.aedpregnancyregistry.org.
Patient Education
What is this drug used for?
- It is used to help control certain kinds of seizures.
- It is used to treat infantile spasms.
Frequently reported side effects of this drug
- Fatigue
- Constipation
- Abdominal pain
- Cough
- Sore throat
- Stuffy nose
- Common cold symptoms
- Headache
- Trouble sleeping
- Joint pain
- Diarrhea
- Nausea
- Vomiting
- Lack of appetite
- Weight gain
- Tooth pain
- Back pain
- Increased appetite
- Tremors
- Flu-like symptoms
- Anxiety
- Nightmares
- Twitching
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Urinary tract infection like blood in the urine, burning or painful urination, passing a lot of urine, fever, lower abdominal pain, or pelvic pain
- Burning or numbness feeling
- Chest pain
- Change in balance
- Severe dizziness
- Passing out
- Confusion
- Trouble focusing
- Behavioral changes
- Ear pain
- Seizures
- Severe loss of strength and energy
- Vision changes
- Blurred vision
- Trouble controlling eye movements
- Clumsiness
- Blindness
- Severe muscle pain
- Severe muscle weakness
- Swelling
- Trouble with memory
- Abnormal gait
- Sexual dysfunction
- Painful periods
- Depression like thoughts of suicide, anxiety, emotional instability, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.