Boxed Warning
Bleeding risk:
Warfarin can cause major or fatal bleeding. Perform regular monitoring of international normalized ratio (INR) on all treated patients. Drugs, dietary changes, and other factors affect INR levels achieved with warfarin therapy. Instruct patients about prevention measures to minimize the risk of bleeding and to report immediately to their health care provider signs and symptoms of bleeding.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
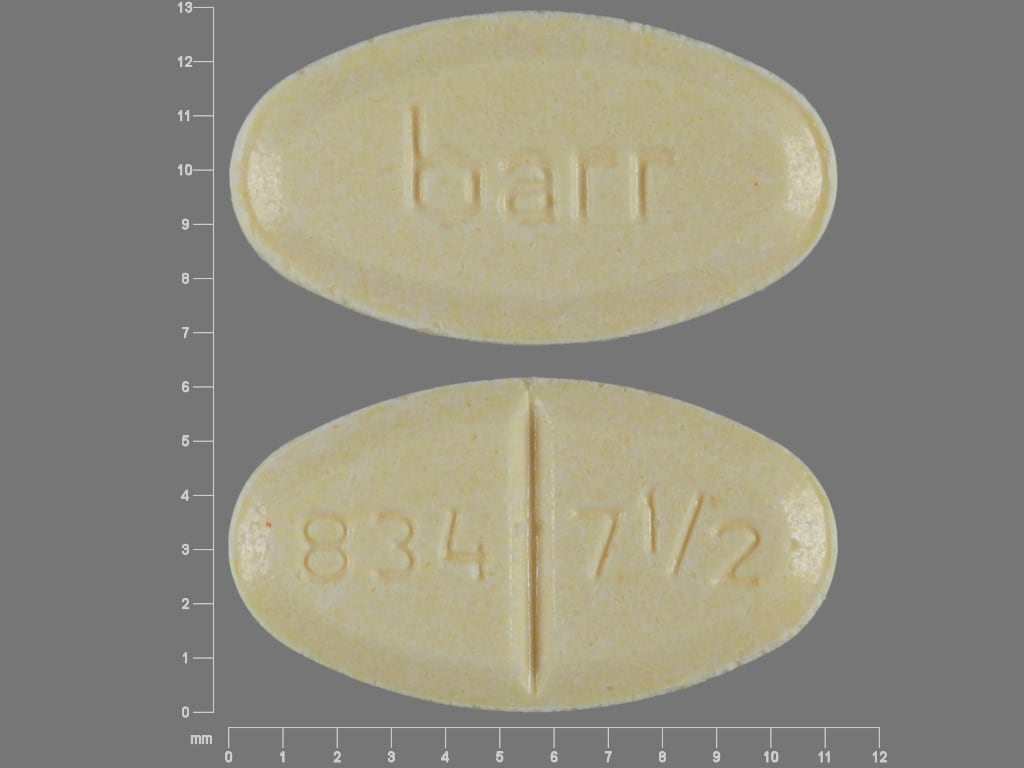
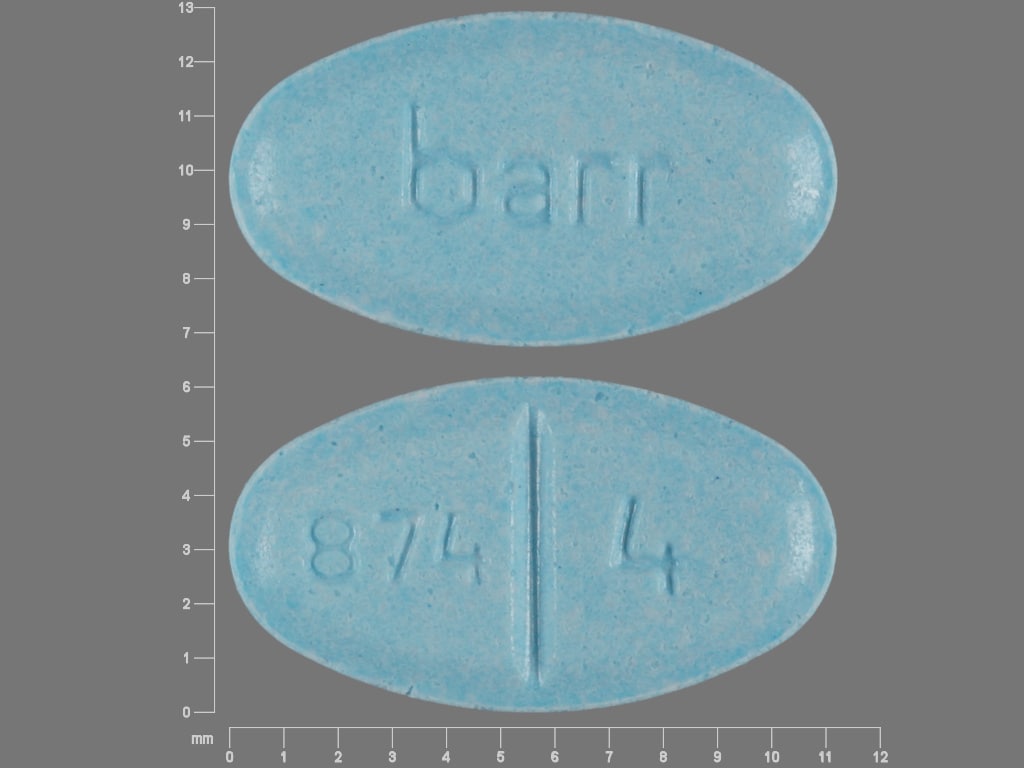
Tablet, Oral, as sodium:
Coumadin: 1 mg [scored]
Coumadin: 2 mg [scored; contains fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake]
Coumadin: 2.5 mg [scored; contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake]
Coumadin: 3 mg [scored; contains fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake, fd&c yellow #6 aluminum lake]
Coumadin: 4 mg [scored; contains fd&c blue #1 aluminum lake]
Coumadin: 5 mg [scored; contains fd&c yellow #6 aluminum lake]
Coumadin: 6 mg [scored; contains fd&c blue #1 aluminum lake, fd&c yellow #6 aluminum lake]
Coumadin: 7.5 mg [scored; contains fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Coumadin: 10 mg [scored; dye free]
Jantoven: 1 mg [scored; contains fd&c red #40 aluminum lake]
Jantoven: 2 mg [scored; contains fd&c blue #2 aluminum lake, fd&c red #40 aluminum lake]
Jantoven: 2.5 mg [scored; contains fd&c blue #1 aluminum lake, fd&c yellow #10 aluminum lake]
Jantoven: 3 mg [scored]
Jantoven: 4 mg [scored; contains fd&c blue #1 aluminum lake]
Jantoven: 5 mg [scored; contains fd&c yellow #6 aluminum lake]
Jantoven: 6 mg [scored; contains fd&c blue #1 aluminum lake]
Jantoven: 7.5 mg [scored; contains fd&c yellow #10 aluminum lake, fd&c yellow #6 aluminum lake]
Jantoven: 10 mg [scored]
Generic: 1 mg, 2 mg, 2.5 mg, 3 mg, 4 mg, 5 mg, 6 mg, 7.5 mg, 10 mg
Pharmacology
Mechanism of Action
Hepatic synthesis of coagulation factors II (half-life 42 to 72 hours), VII (half-life 4 to 6 hours), IX, and X (half-life 27 to 48 hours), as well as proteins C and S, requires the presence of vitamin K. These clotting factors are biologically activated by the addition of carboxyl groups to key glutamic acid residues within the proteins’ structure. In the process, “active” vitamin K is oxidatively converted to an “inactive” form, which is then subsequently reactivated by vitamin K epoxide reductase complex 1 (VKORC1). Warfarin competitively inhibits the subunit 1 of the multi-unit VKOR complex, thus depleting functional vitamin K reserves and hence reduces synthesis of active clotting factors.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid, complete
Distribution
0.14 L/kg
Metabolism
Hepatic, primarily via CYP2C9; minor pathways include CYP2C8, 2C18, 2C19, 1A2, and 3A4
Genomic variants: Approximately 37% reduced clearance of S-warfarin in patients heterozygous for 2C9 (*1/*2 or *1/*3), and ~70% reduced in patients homozygous for reduced function alleles (*2/*2, *2/*3, or *3/*3)
Excretion
Urine (92%), primarily as metabolites; minimal as unchanged drug)
Onset of Action
Initial anticoagulant effect on INR may be seen as soon as 24 to 72 hours (Harrison 1997; O’Reilly 1968).
Note: Full therapeutic effect generally seen between 5 and 7 days after initiation; dependent on reduction in vitamin K-dependent coagulation factors, especially prothrombin (factor II), which has a half-life of 60 to 72 hours (ACCP [Ageno 2012]; Crowther 1999; Kovacs 2003; manufacturer's labeling).
Time to Peak
~4 hours
Duration of Action
2 to 5 days
Half-Life Elimination
20-60 hours; Mean: 40 hours; highly variable among individuals
Protein Binding
99%
Use in Specific Populations
Special Populations: Renal Function Impairment
Renal Cl is a minor determinant of anticoagulant response to warfarin.
Special Populations: Hepatic Function Impairment
Hepatic impairment can potentiate the response to warfarin through impaired synthesis of clotting factors and decreased metabolism of warfarin.
Special Populations: Elderly
Patients 60 years and older appear to exhibit greater than expected INR response to warfarin.
Special Populations: Race
Asian patients may require lower initiation and maintenance doses.
Special Populations Note
Pharmacogenetics: Vitamin K epoxide reductase (VKORC1) and CYP2C9 gene variants generally explain the largest proportion of known variability in warfarin dose requirements.
Use: Labeled Indications
Myocardial infarction: Adjunct to reduce risk of systemic embolism (eg, recurrent myocardial infarction, stroke) after myocardial infarction.
Thromboembolic complications: Prophylaxis and treatment of thromboembolic disorders (eg, venous, pulmonary) and embolic complications arising from atrial fibrillation or cardiac valve replacement.
Limitations of use: Warfarin has no direct effect on an established thrombus and does not reverse ischemic tissue damage. The goal of anticoagulant therapy is to prevent further extension of an already formed thrombus and to prevent secondary thromboembolic complications that may result in serious and potentially fatal sequelae.
Contraindications
Hypersensitivity to warfarin or any component of the formulation; hemorrhagic tendencies (eg, active GI ulceration, patients bleeding from the GI, respiratory, or GU tract; cerebral aneurysm; CNS hemorrhage; dissecting aortic aneurysm; spinal puncture and other diagnostic or therapeutic procedures with potential for significant bleeding); recent or potential surgery of the eye or CNS; major regional lumbar block anesthesia or traumatic surgery resulting in large, open surfaces; blood dyscrasias; malignant hypertension; pericarditis or pericardial effusion; bacterial endocarditis; unsupervised patients with conditions associated with a high potential for noncompliance; eclampsia/preeclampsia, threatened abortion, pregnancy (except in women with mechanical heart valves at high risk for thromboembolism)
Dosage and Administration
Dosing: Adult
Note: Dosing must be individualized and use of an institutional protocol is recommended (ACCP [Holbrook 2012]; Nutescu 2013). Response to warfarin is influenced by numerous factors (eg, age, organ function) as described below. Genetic variations in metabolism (eg, CYP2C9 and/or VKORC1 genes) can impact warfarin sensitivity; however, routine genetic testing is not recommended (ACCP [Holbrook 2012]; CPIC [Johnson 2017]).
Oral:
Initial: 5 mg once daily for most patients. A lower or higher starting dose may be used depending upon patient-specific factors (see example warfarin initiation nomogram below). Although an elevation in INR can be seen as soon as 24 to 48 hours after the first dose due to depletion of factor VII, this does not represent therapeutic anticoagulation because other vitamin K–dependent clotting factors with longer half-lives (eg, factors II, IX, and X) must also be depleted. Accordingly, in patients at high risk for thromboembolism, overlap (“bridging”) with a parenteral anticoagulant may be necessary during initiation of warfarin until a stable therapeutic INR is attained (Wittkowsky 2018).
|
Standard dosing for patients who are not expected to be sensitive to warfarinb |
Reduced dosing for patients expected to be more sensitive to warfarinc |
|
|---|---|---|
| aDosing nomograms offer a reasonable starting point for estimating an initial warfarin dose and subsequent adjustments but should not serve as a substitute for clinical judgment. If the patient received warfarin previously, history of prior dose requirement is useful for guiding reinitiation of therapy. | ||
| bPatients who are generally started using “standard dosing” include otherwise healthy adults who are not receiving interacting medications. | ||
| cPatients expected to be more sensitive to warfarin include adults who are frail, elderly, or undernourished; have liver disease, kidney disease, heart failure, or acute illness; or are receiving a medication known to decrease warfarin metabolism. | ||
| dSome experts suggest starting select younger, otherwise healthy patients at 7.5 or 10 mg for the first 2 days (ACCP [Holbrook 2012]). A higher initial dose may also be appropriate in a patient who was previously treated with warfarin and required high doses or is receiving a medication that increases warfarin metabolism. However, this nomogram has not been validated for starting doses >5 mg/day. | ||
|
Initial dose |
5 mg daily for 3 daysd |
2.5 mg daily for 3 days |
|
Check INR the morning of day 4 |
||
|
<1.5 |
7.5 to 10 mg daily for 2 to 3 days |
5 to 7.5 mg daily for 2 to 3 days |
|
1.5 to 1.9 |
5 mg daily for 2 to 3 days |
2.5 mg daily for 2 to 3 days |
|
2 to 3 |
2.5 mg daily for 2 to 3 days |
1.25 mg daily for 2 to 3 days |
|
3.1 to 4 |
1.25 mg daily for 2 to 3 days |
0.5 mg daily for 2 to 3 days |
|
>4 |
Hold until INR <3 |
Hold until INR <3 |
Maintenance: Usual maintenance dose: 2 to 10 mg once daily. Once INR is therapeutic and stable following initiation, subsequent dosage requirements may be guided with the use of a maintenance dosing nomogram (see example warfarin maintenance dosing nomogram below). INR should be checked at least weekly when it is out of range and approximately every 4 weeks once therapeutic and stable. In chronic therapy, INR values are most affected by the doses administered 2 to 3 days prior to INR measurement.
| aAs with initiation therapy nomograms, maintenance therapy nomograms must be used in conjunction with clinical judgment. | ||
| bAs an example, a patient with an INR goal of 2 to 3 and receiving 30 mg of warfarin per week (eg, administered as 5 mg on 5 days and 2.5 mg on 2 days) has an INR result of 1.4. The weekly dose should be increased by 10% to 20% (eg, increase to 35 mg per week by administering 5 mg once daily). A one-time supplemental dose of 7.5 mg may be considered on the day INR was checked, then start new maintenance dose (eg, 5 mg daily) the following day. | ||
|
Regular-intensity anticoagulation: INR goal 2 to 3 |
High-intensity anticoagulation: INR goal 2.5 to 3.5 |
Suggested adjustment(s) to warfarin dose |
|
Adjustment(s) for subtherapeutic (low) INR – Note: If the factor causing subtherapeutic INR is transient (eg, missed warfarin dose or temporary change in vitamin K intake), consider resumption of prior maintenance dose following a one-time supplemental dose, if indicated. |
||
|
INR <1.5 |
INR <2 |
|
|
INR 1.5 to 1.7 |
INR 2 to 2.2 |
|
|
INR 1.8 to 1.9 |
INR 2.3 to 2.4 |
|
|
INR within therapeutic range |
||
|
INR 2 to 3 |
INR 2.5 to 3.5 |
Desired range; no adjustment needed |
|
Adjustment(s) for supratherapeutic (high) INR – Note: If the factor causing elevated INR is transient (eg, temporary change in vitamin K intake, acute illness, acute alcohol ingestion), consider resumption of prior maintenance dose following dose(s) held and low-dose oral vitamin K, if indicated. |
||
|
INR 3.1 to 3.2 |
INR 3.6 to 3.7 |
|
|
INR 3.3 to 3.4 |
INR 3.8 to 3.9 |
|
|
INR 3.5 to 3.9 |
INR 4 to 4.4 |
|
|
INR >4 but ≤10 and no bleeding |
INR >4.5 but ≤10 and no bleeding |
|
|
INR >10 and no bleeding |
INR >10 and no bleeding |
|
|
Indication |
Targeted INR range |
Treatment duration |
|---|---|---|
|
Cardiac |
||
|
Myocardial infarction with left ventricular thrombus or high risk for left ventricular thrombus (eg, ejection fraction <40% and severe anteroapical wall motion abnormality on imaging 48 hours after reperfusion) (ACCF/AHA [O’Gara 2013]; ACCP [Vandvik 2012]). Note: Antiplatelet selection and duration of therapy for treatment of myocardial infarction may vary when used in combination with anticoagulation; consider risks of bleeding and thrombotic events when choosing antithrombotic therapy (ACCP [Vandvik 2012]; Lip 2019). |
2 to 3 |
3 months after myocardial infarction |
|
Atrial fibrillation or atrial flutter (AHA/ACC/HRS [January 2014, January 2019]). Note: For eligible patients with nonvalvular atrial fibrillation, a direct oral anticoagulant is recommended over warfarin (AHA/ACC/HRS [January 2014, January 2019]). |
2 to 3 |
Indefinite |
|
Stress (takotsubo) cardiomyopathy with acute left ventricular thrombus (ACCP [Vandvik 2012]) |
2 to 3 |
3 months |
|
Valvular – Note: For mechanical valves, aspirin in combination with warfarin is recommended indefinitely. For surgically placed bioprosthetic valves, aspirin therapy is recommended indefinitely and concurrent warfarin is suggested for the first 3 to 6 months. When choosing antithrombotic therapy, additional risk factors for thromboembolism (eg, atrial fibrillation, previous thromboembolism, left ventricular systolic dysfunction, hypercoagulable conditions) should be considered. The goal INR is generally the central value in the indicated acceptable range, especially for patients with a mechanical valve (AHA/ACC [Nishimura 2014, Nishimura 2017]). |
||
|
On-X mechanical bileaflet aortic valve with no additional risk factors for thromboembolism (AHA/ACC [Nishimura 2017]; Puskas 2014) |
Months 1 to 3: 2 to 3 Month 4 and after: 1.5 to 2 |
Indefinite |
|
Mechanical bileaflet aortic valve (other than On-X) or current-generation single-tilting disc aortic valve with no additional risk factors for thromboembolism (AHA/ACC [Nishimura 2014, Nishimura 2017]) |
2 to 3 |
Indefinite |
|
Mechanical aortic valve with additional risk factors for thromboembolism or an older-generation mechanical aortic valve or mechanical mitral valve (including On-X valve) (AHA/ACC [Nishimura 2014, Nishimura 2017]) |
2.5 to 3.5 |
Indefinite |
|
Surgically placed bioprosthetic aortic or mitral valve at low risk of bleeding (AHA/ACC [Nishimura 2014, Nishimura 2017]) |
2 to 3 |
3 to 6 months |
|
Rheumatic mitral stenosis with atrial fibrillation, previous systemic embolism, or left atrial thrombus (AHA/ACC [Nishimura 2014]) |
2 to 3 |
Indefinite |
|
Acute venous thromboembolism treatment – Note: For eligible patients, a direct oral anticoagulant is recommended over warfarin. When warfarin is selected for long-term treatment, a parenteral anticoagulant must be used initially as a bridge until INR measurements are therapeutic and stable. Start warfarin on the first or second day of parenteral anticoagulation and overlap until INR is ≥2 for at least 2 days. Duration of overlap is usually 4 to 5 days (ACCP [Ageno 2012]). The optimal duration of warfarin therapy is dependent on several factors, such as presence of provoking events, patient risk factors for recurrence or bleeding, and patient preferences. If indefinite treatment is suggested, reassess need for anticoagulation at periodic intervals (ACCP [Kearon 2012, Kearon 2016]). |
||
|
Venous thromboembolism, provoked (ACCP [Kearon 2012, Kearon 2016]) |
2 to 3 |
Minimum of 3 months |
|
Venous thromboembolism, unprovoked (ACCP [Kearon 2012, Kearon 2016]; ISTH [Baglin 2012]) |
2 to 3 |
Minimum of 3 months and up to indefinite |
|
Thromboprophylaxis |
||
|
Idiopathic or inherited pulmonary artery hypertension (ACCF/AHA [McLaughlin 2009]; ACCP [Klinger 2019]; ESC/ERS [Galiè 2016]; Olsson 2014) – Note: Anticoagulation should be considered on an individual basis for patients with idiopathic or inherited pulmonary arterial hypertension after considering risks and benefits. Avoid anticoagulation in patients with scleroderma-associated pulmonary arterial hypertension (Hopkins 2019; Khan 2018; Olsson 2014). |
1.5 to 2.5 |
Indefinite |
|
Chronic thromboembolic pulmonary arterial hypertension (ACCF/AHA [McLaughlin 2009]; ESC/ERS [Galiè 2016]) |
2 to 3 |
Indefinite |
|
Antiphospholipid syndrome (ACCP [Holbrook 2012]; Erkan 2019) – Note: Antiphospholipid syndrome is an autoimmune syndrome characterized by venous or arterial thrombosis and/or pregnancy loss in the presence of persistent antiphospholipid antibodies. Patients with antiphospholipid antibodies alone, without a history of thromboembolism, should not receive anticoagulation unless another indication exists. The PT/INR may be prolonged at baseline, in the absence of anticoagulation, in a small percentage of patients due to the presence of antiphospholipid antibodies. This should not be considered a therapeutic effect. An alternative method for monitoring warfarin may be necessary (Erkan 2019). |
2 to 3 |
Indefinite |
|
Total hip arthroplasty or hip fracture surgery – Note: May be used as an alternative to low-molecular-weight heparin or low-dose SubQ heparin (ACCP [Falck-Ytter 2012]). |
2 to 3 |
Minimum of 10 to 14 days and up to 35 days |
|
Total knee arthroplasty – Note: May be used as an alternative to low-molecular-weight heparin or low-dose SubQ heparin (ACCP [Falck-Ytter 2012]). |
2 to 3 |
Typically, 10 to 14 days, but consider up to 35 days if there are multiple or persistent risk factors |
|
Heparin-induced thrombocytopenia – Note: If a patient is taking warfarin at the time of diagnosis, it should be discontinued, and vitamin K should be administered to reverse its effect. Initial therapy should be with a parenteral nonheparin anticoagulant. Warfarin may be initiated after the patient has been stably anticoagulated with a parenteral nonheparin anticoagulant and the platelet count has recovered (eg, ≥150 × 109/L or at the patient's baseline). Starting dose should be ≤5 mg once daily. Overlap the parenteral nonheparin anticoagulant with warfarin for ≥5 days and until INR is therapeutic. Some nonheparin anticoagulants may elevate INR, complicating interpretation. Recheck INR after effects of the nonheparin anticoagulant have worn off to ensure INR remains therapeutic (ACCP [Linkins 2012]; ASH [Cuker 2018]). |
||
|
Heparin-induced thrombocytopenia without thrombosis (ACCP [Linkins 2012]; ASH [Cuker 2018]) |
2 to 3 |
4 weeks to 3 months (ACCP [Linkins 2012]). Some experts allow for discontinuation of anticoagulation after platelet count recovery, potentially resulting in a shorter duration (ASH [Cuker 2018]). |
|
Heparin-induced thrombocytopenia with thrombosis (ACCP [Linkins 2012]; ASH [Cuker 2018]) |
2 to 3 |
Optimal duration not well established. Typically, 3 to 6 months (ACCP [Linkins 2012]; ASH [Cuker 2018]). |
Transitioning between anticoagulants:
Transitioning from another anticoagulant to warfarin: Note: Apixaban, dabigatran, edoxaban, and rivaroxaban can elevate INR, complicating interpretation if overlapped with warfarin. To minimize interference, check INR near end of direct oral anticoagulant dosing interval.
Transitioning from apixaban to warfarin: Some experts suggest overlapping apixaban with warfarin for ≥2 days until INR is therapeutic. An alternative is to stop apixaban, start warfarin the same day, and bridge with a parenteral anticoagulant until the desired INR is reached (Leung 2019).
Transitioning from dabigatran to warfarin: One option is to stop dabigatran, start warfarin the same day, and bridge with a parenteral anticoagulant until the desired INR is reached (Leung 2019). An alternative option is to overlap the 2 agents. If this is done, the timing of warfarin initiation is based on CrCl as outlined below:
CrCl >50 mL/minute: Initiate warfarin 3 days before discontinuing dabigatran.
CrCl 30 to 50 mL/minute: Initiate warfarin 2 days before discontinuing dabigatran.
CrCl 15 to 30 mL/minute: Initiate warfarin 1 day before discontinuing dabigatran.
CrCl <15 mL/minute: Dosing recommendations cannot be provided. Dabigatran is not recommended for use in patients with severe renal impairment.
Transitioning from edoxaban to warfarin:
Oral option: For patients taking edoxaban 60 mg once daily, reduce the dose to 30 mg once daily and begin warfarin concomitantly. For patients taking edoxaban 30 mg once daily, reduce the dose to 15 mg once daily and begin warfarin concomitantly. Discontinue edoxaban once a stable INR ≥2 is achieved; continue warfarin (Leung 2019).
Parenteral option: Discontinue edoxaban and initiate a parenteral anticoagulant and warfarin at the time of the next scheduled edoxaban dose. Discontinue the parenteral anticoagulant once a stable INR ≥2 is achieved; continue warfarin.
Transitioning from rivaroxaban to warfarin: Some experts suggest overlapping rivaroxaban with warfarin for ≥2 days until INR is therapeutic. An alternative is to stop rivaroxaban, start warfarin the same day, and bridge with a parenteral anticoagulant until the desired INR is reached (Leung 2019).
Transitioning from therapeutic-dose parenteral anticoagulant to warfarin: Start warfarin and continue parenteral anticoagulant until INR is within therapeutic range (Hull 2019a; Wittkowsky 2018). Note: For the treatment of venous thromboembolism, overlap parenteral anticoagulant with warfarin until INR is ≥2 for at least 2 days (duration of overlap is usually 4 to 5 days) (ACCP [Ageno 2012]; Hull 2019b).
Transitioning from warfarin to another anticoagulant:
Note: In general, it is reasonable to discontinue warfarin and initiate another anticoagulant as soon as INR is ≤2 depending on the indication and risks of thrombosis and bleeding (Leung 2019). Specific recommendations from manufacturers include:
Transitioning from warfarin to apixaban: Discontinue warfarin and initiate apixaban as soon as INR falls to <2 (US labeling).
Transitioning from warfarin to dabigatran: Discontinue warfarin and initiate dabigatran as soon as INR falls to <2 (US labeling).
Transitioning from warfarin to edoxaban: Discontinue warfarin and initiate edoxaban as soon as INR falls to ≤2.5 (US labeling).
Transitioning from warfarin to rivaroxaban: Discontinue warfarin and initiate rivaroxaban as soon as INR falls to <3 (US labeling) or ≤ 2.5 (Canadian labeling).
Transitioning from warfarin to parenteral anticoagulation: Stop warfarin and start the parenteral anticoagulant when INR is as close as possible to the lower end of the targeted INR range (Wittkowsky 2018).
Dosing: Geriatric
Patients >60 years of age tend to require lower dosages to produce a therapeutic level of anticoagulation (due to changes in the pattern of warfarin metabolism).
Dosing: Pediatric
Note: Labeling identifies genetic factors which may increase patient sensitivity to warfarin based on experience in adult patients. Specifically, genetic variations in the proteins CYP2C9 and VKORC1, responsible for warfarin’s primary metabolism and pharmacodynamic activity, respectively, have been identified as predisposing factors associated with decreased dose requirement and increased bleeding risk. Genotyping tests are available, and may provide guidance on initiation of anticoagulant therapy. The American College of Chest Physicians recommends against the use of routine pharmacogenomic testing to guide dosing (Guyatt 2012). For management of elevated INRs as a result of warfarin therapy, see phytonadione monograph or ACCP Guidelines for additional information (ACCP [Monagle 2012]).
Thromboembolic complications; prophylaxis and treatment: Limited data available (ACCP [Monagle 2012]): Individualize dose to achieve target INR based on indication; INRs are primarily extrapolated from adult experience; although there may be some exceptions, for most indications the therapeutic target INR is 2.5 (range: 2 to 3), and for low-dose prophylaxis, a target INR is 1.7 (range: 1.5 to 1.9); see Reference Range for more information and consult expert guidelines. Infants, Children, and Adolescents: Oral:
Target International Normalized Ratio (INR) between 2 to 3 (eg, treatment):
Day 1: Initial loading dose (if baseline INR is 1 to 1.3): 0.2 mg/kg/day once daily; maximum dose: 10 mg/dose; use a reduced initial loading dose of 0.1 mg/kg if patient has undergone a Fontan procedure (AHA [Giglia 2013]) or has liver dysfunction (Streif 1999)
Days 2 to 4: Additional loading doses are dependent upon patient's INR:
INR 1.1 to 1.3: Repeat the initial loading dose
INR 1.4 to 1.9: Dose is 50% of the initial loading dose
INR 2 to 3: Dose is 50% of the initial loading dose
INR 3.1 to 3.5: Dose is 25% of the initial loading dose
INR >3.5: Hold the drug until INR <3.5, then restart at 50% of previous dose
Days ≥5: Maintenance doses are dependent upon patient's INR
INR 1.1 to 1.4: Increase dose by 20% of previous dose
INR 1.5 to 1.9: Increase dose by 10% of previous dose
INR 2 to 3: No change
INR 3.1 to 3.5: Decrease dose by 10% of previous dose
INR >3.5: Hold the drug until INR <3.5, then restart at 20% less than the previous dose
Usual maintenance dose: ~0.1 mg/kg/day once daily; range: 0.05 to 0.34 mg/kg/day; the dose in mg/kg/day is inversely related to age. In the largest pediatric study (n=319) (Streif 1999), infants <12 months required a mean dose of 0.33 mg/kg/day, but children 13 to 18 years required a mean dose of 0.09 mg/kg/day; a target INR of 2 to 3 was used for a majority of these patients (75% of warfarin courses). Overall, children required a mean dose of 0.16 mg/kg/day to achieve a target INR of 2 to 3. In another study (Andrew 1994), to attain an INR of 1.3 to 1.8, infants <12 months (n=2) required 0.24 and 0.27 mg/kg/day, but children >1 year required a mean of 0.08 mg/kg/day (range: 0.03 to 0.17 mg/kg/day). Consistent anticoagulation may be difficult to maintain in children <5 years. Children receiving phenobarbital, carbamazepine, or enteral nutrition may require higher maintenance doses (Streif 1999).
Administration
Oral: Administer with or without food. Warfarin should be administered orally once a day at approximately the same time. In clinical practice, patients are often encouraged to take their dose later in the day to facilitate implementation of needed dose changes identified at daytime monitoring visits (Wittkowsky 2018).
Dietary Considerations
Foods high in vitamin K (eg, leafy green vegetables) inhibit anticoagulant effect. The list of usual foods with high vitamin K content is well known, however, some unique ones include green tea (Camellia sinensis), chewing tobacco, a variety of oils (canola, corn, olive, peanut, safflower, sesame seed, soybean, and sunflower) (Booth 1999; Kuykendall 2004; Nutescu 2011). Snack foods containing Olestra have 80 mcg of vitamin K added to each ounce (Harrell 1999). Some natural products may contain hidden sources of vitamin K (Nutescu 2006). Avoid drastic changes in diet (eg, intake of large amounts of alfalfa, asparagus, broccoli, Brussels sprouts, cabbage, cauliflower, green teas, kale, lettuce, spinach, turnip greens, watercress) which decrease efficacy of warfarin. A balanced diet with a consistent intake of vitamin K is essential. The recommended dietary allowance for vitamin K in adults is 75 to 120 mcg/day (USDA Dietary Reference Intake).
Storage
Store at 15°C to 30°C (59°F to 86°F). Protect from light.
Warfarin Images
Drug Interactions
Acalabrutinib: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Acetaminophen: May enhance the anticoagulant effect of Vitamin K Antagonists. This appears most likely with daily acetaminophen doses exceeding 1.3 or 2 g/day for multiple consecutive days. Monitor therapy
Adalimumab: May decrease the serum concentration of Warfarin. Monitor therapy
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Alcohol (Ethyl): May decrease the serum concentration of Vitamin K Antagonists. More specifically, this effect has been described in heavy drinking alcoholic patients (over 250 g alcohol daily for over 3 months). The role of alcohol itself is unclear. Monitor therapy
Allopurinol: May enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Alpelisib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Amiodarone: May enhance the anticoagulant effect of Vitamin K Antagonists. Amiodarone may increase the serum concentration of Vitamin K Antagonists. Management: Monitor patients extra closely for evidence of increased anticoagulant effects if amiodarone is started. Consider empiric reduction of 30% to 50% in warfarin dose, though no specific guidelines on dose adjustment have been published. Consider therapy modification
Androgens: May enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Anticoagulants: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Antithyroid Agents: May diminish the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Apalutamide: May decrease the serum concentration of Warfarin. Monitor therapy
Aprepitant: May decrease the serum concentration of Warfarin. Monitor therapy
Atazanavir: May increase the serum concentration of Warfarin. Monitor therapy
AzaTHIOprine: May diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Barbiturates: May increase the metabolism of Vitamin K Antagonists. Management: Monitor INR more closely. An anticoagulant dose increase may be needed after a barbiturate is initiated or given at an increased dose. Anticoagulant dose decreases may be needed following barbiturate discontinuation or dose reduction. Consider therapy modification
Benzbromarone: May increase the serum concentration of Warfarin. Monitor therapy
Bicalutamide: May increase the serum concentration of Vitamin K Antagonists. Specifically, free concentrations of the vitamin K antagonists may be increased. Monitor therapy
Bifonazole: May enhance the anticoagulant effect of Warfarin. Monitor therapy
Bile Acid Sequestrants: May decrease the absorption of Vitamin K Antagonists. Monitor therapy
Bosentan: May increase the metabolism of Vitamin K Antagonists. Monitor therapy
Bromperidol: May enhance the adverse/toxic effect of Anticoagulants. Monitor therapy
Cannabinoid-Containing Products: May increase the serum concentration of Warfarin. Monitor therapy
Caplacizumab: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
CarBAMazepine: May decrease the serum concentration of Vitamin K Antagonists. Management: Monitor for decreased INR and effects of vitamin K antagonists if carbamazepine is initiated/dose increased, or increased INR and effects if carbamazepine is discontinued/dose decreased. Warfarin dose adjustments will likely be required. Consider therapy modification
Cephalosporins: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Ceritinib: May increase the serum concentration of Warfarin. Monitor therapy
Chenodiol: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Chloral Betaine: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Chloral Hydrate: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Chloramphenicol (Systemic): May enhance the anticoagulant effect of Vitamin K Antagonists. Chloramphenicol (Systemic) may increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Chondroitin Sulfate: May enhance the anticoagulant effect of Warfarin. Monitor therapy
Cimetidine: May enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Clopidogrel: May enhance the anticoagulant effect of Warfarin. Consider therapy modification
Cloxacillin: May diminish the anticoagulant effect of Vitamin K Antagonists. Cloxacillin may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Cobicistat: May increase the serum concentration of Warfarin. Monitor therapy
Coenzyme Q-10: May diminish the anticoagulant effect of Vitamin K Antagonists. Coenzyme Q-10 may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Collagenase (Systemic): Anticoagulants may enhance the adverse/toxic effect of Collagenase (Systemic). Specifically, the risk of injection site bruising and/or bleeding may be increased. Monitor therapy
Corticosteroids (Systemic): May enhance the anticoagulant effect of Warfarin. Monitor therapy
Cranberry: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
CYP2C9 Inducers (Moderate): May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
CYP2C9 Inhibitors (Moderate): May decrease the metabolism of CYP2C9 Substrates (High risk with Inhibitors). Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP2C9 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Darunavir: May decrease the serum concentration of Warfarin. Darunavir may increase the serum concentration of Warfarin. Monitor therapy
Dasatinib: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Deferasirox: Anticoagulants may enhance the adverse/toxic effect of Deferasirox. Specifically, the risk for GI ulceration/irritation or GI bleeding may be increased. Monitor therapy
Deoxycholic Acid: Anticoagulants may enhance the adverse/toxic effect of Deoxycholic Acid. Specifically, the risk for bleeding or bruising in the treatment area may be increased. Monitor therapy
Desirudin: Anticoagulants may enhance the anticoagulant effect of Desirudin. Consider therapy modification
Desvenlafaxine: May enhance the adverse/toxic effect of Vitamin K Antagonists. Specifically, the risk for bleeding may be increased. Monitor therapy
Dexmethylphenidate: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Dicloxacillin: May diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Direct Acting Antiviral Agents (HCV): May diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Disulfiram: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Dronabinol: May increase the serum concentration of Warfarin. Specifically, dronabinol may displace warfarin from its protein-binding sites, leading to an increased concentration of active, unbound drug. Monitor therapy
Dronedarone: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Econazole: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Efavirenz: May decrease the serum concentration of Vitamin K Antagonists. Efavirenz may increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Elexacaftor, Tezacaftor, and Ivacaftor: May increase the serum concentration of Warfarin. Monitor therapy
Enzalutamide: May decrease the serum concentration of Warfarin. More specifically, enzalutamide may decrease concentrations of the S-warfarin enantiomer. Management: Avoid concurrent use of warfarin and enzalutamide whenever possible. If the combination must be used, conduct additional INR monitoring as serum concentrations may be decreased. Consider therapy modification
Erlotinib: May increase the serum concentration of Warfarin. Monitor therapy
Erythromycin (Ophthalmic): May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Eslicarbazepine: May decrease the serum concentration of Warfarin. Specifically, S-warfarin serum concentrations may be decreased. Monitor therapy
Esomeprazole: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Estrogen Derivatives: May diminish the anticoagulant effect of Anticoagulants. More specifically, the potential prothrombotic effects of some estrogens and progestin-estrogen combinations may counteract anticoagulant effects. Management: Carefully weigh the prospective benefits of estrogens against the potential increased risk of procoagulant effects and thromboembolism. Use is considered contraindicated under some circumstances. Refer to related guidelines for specific recommendations. Exceptions: Tibolone. Consider therapy modification
Estrogen Derivatives (Contraceptive): May diminish the anticoagulant effect of Vitamin K Antagonists. In contrast, enhanced anticoagulant effects have also been noted with some products. Consider therapy modification
Ethacrynic Acid: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Ethotoin: May enhance the anticoagulant effect of Vitamin K Antagonists. Vitamin K Antagonists may increase the serum concentration of Ethotoin. Management: Anticoagulant dose adjustment will likely be necessary when ethotoin is initiated or discontinued. Monitor patients extra closely (INR and signs/symptoms of bleeding) when using this combination. Consider therapy modification
Etoposide: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Etoposide Phosphate: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Exenatide: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Fat Emulsion (Fish Oil and Plant Based): May diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Fat Emulsion (Fish Oil Based): May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Fenofibrate and Derivatives: May enhance the anticoagulant effect of Warfarin. Fenofibrate and Derivatives may increase the serum concentration of Warfarin. Consider therapy modification
Fenugreek: May enhance the anticoagulant effect of Vitamin K Antagonists. Management: Seek alternatives to fenugreek in patients receiving vitamin K antagonists. Monitor patients receiving these combinations closely for increases in INR and systemic effects of the vitamin K antagonist (particularly easy bruising and bleeding). Consider therapy modification
Fibric Acid Derivatives: May enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Flucloxacillin: May diminish the anticoagulant effect of Vitamin K Antagonists. Flucloxacillin may decrease the serum concentration of Vitamin K Antagonists. Monitor therapy
Fluconazole: May increase the serum concentration of Vitamin K Antagonists. Consider therapy modification
Fluorouracil (Topical): May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Fluorouracil Products: May increase the serum concentration of Vitamin K Antagonists. Management: Monitor INR and for signs/symptoms of bleeding closely when a fluorouracil product is combined with a vitamin K antagonist (eg, warfarin). Anticoagulant dose adjustment will likely be necessary. Consider therapy modification
Fosamprenavir: May increase the serum concentration of Warfarin. Monitor therapy
Fosaprepitant: May decrease the serum concentration of Warfarin. The active metabolite aprepitant is likely responsible for this effect. Monitor therapy
Fosphenytoin: May enhance the anticoagulant effect of Vitamin K Antagonists. Vitamin K Antagonists may increase the serum concentration of Fosphenytoin. Management: Anticoagulant dose adjustment will likely be necessary when phenytoin is initiated or discontinued. Monitor patients extra closely (INR and signs/symptoms of bleeding) when using this combination. Consider therapy modification
Frankincense, Indian: May enhance the anticoagulant effect of Warfarin. Monitor therapy
Fusidic Acid (Systemic): May increase the serum concentration of Vitamin K Antagonists. Management: Vitamin K antagonist dose adjustments may be required when used with systemic fusidic acid. Patients using this combination should be monitored extra closely for evidence of bleeding and to determine appropriate dose. Consider therapy modification
Gefitinib: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Gemcitabine: May enhance the anticoagulant effect of Warfarin. Monitor therapy
Ginkgo Biloba: May enhance the adverse/toxic effect of Vitamin K Antagonists. Management: Consider avoiding the use of this combination of agents. Monitor for signs and symptoms of bleeding if vitamin K antagonists and Ginkgo biloba are used concomitantly. Consider therapy modification
Ginseng (American): May decrease the serum concentration of Warfarin. Monitor therapy
Glucagon: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Glucosamine: May enhance the anticoagulant effect of Warfarin. Monitor therapy
Glutethimide: May increase the metabolism of Vitamin K Antagonists. Consider therapy modification
Green Tea: May enhance the adverse/toxic effect of Warfarin. Particularly, the risk of bleeding may be increased due to possible antiplatelet effects of green tea. Green Tea may diminish the anticoagulant effect of Warfarin. Monitor therapy
Griseofulvin: May decrease the serum concentration of Vitamin K Antagonists. Monitor therapy
Hemin: May enhance the anticoagulant effect of Anticoagulants. Avoid combination
Herbs (Anticoagulant/Antiplatelet Properties) (eg, Alfalfa, Anise, Bilberry): May enhance the adverse/toxic effect of Anticoagulants. Bleeding may occur. Management: Avoid such combinations when possible. If used concomitantly, increase diligence in monitoring for adverse effects (eg, bleeding, bruising, altered mental status due to CNS bleeds). Consider therapy modification
HMG-CoA Reductase Inhibitors (Statins): May enhance the anticoagulant effect of Vitamin K Antagonists. Exceptions: AtorvaSTATin. Monitor therapy
Ibritumomab Tiuxetan: Anticoagulants may enhance the adverse/toxic effect of Ibritumomab Tiuxetan. Both agents may contribute to an increased risk of bleeding. Monitor therapy
Ibrutinib: May enhance the adverse/toxic effect of Anticoagulants. Monitor therapy
Ifosfamide: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Imatinib: May enhance the anticoagulant effect of Warfarin. Imatinib may decrease the metabolism of Warfarin. Consider therapy modification
Inotersen: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Interferons (Alfa): May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Itraconazole: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Ivermectin (Systemic): May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Ketoconazole (Systemic): May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Lansoprazole: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Leflunomide: May enhance the anticoagulant effect of Vitamin K Antagonists. Leflunomide may diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Letermovir: May decrease the serum concentration of Warfarin. Monitor therapy
LevOCARNitine: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Levomilnacipran: May enhance the adverse/toxic effect of Vitamin K Antagonists. Specifically, the risk for bleeding may be increased. Monitor therapy
Limaprost: May enhance the adverse/toxic effect of Anticoagulants. The risk for bleeding may be increased. Monitor therapy
Lomitapide: May increase the serum concentration of Warfarin. Monitor therapy
Lopinavir: May decrease the serum concentration of Warfarin. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Lumacaftor and Ivacaftor may increase the serum concentration of CYP2C9 Substrates (High Risk with Inhibitors or Inducers). Monitor therapy
Macrolide Antibiotics: May increase the serum concentration of Vitamin K Antagonists. Exceptions: Fidaxomicin; Roxithromycin; Spiramycin. Monitor therapy
Maitake: May increase the serum concentration of Warfarin. Monitor therapy
Menadiol Diphosphate: May diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Menatetrenone: May diminish the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Mercaptopurine: May diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Methylphenidate: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Metreleptin: May decrease the serum concentration of Warfarin. Metreleptin may increase the serum concentration of Warfarin. Monitor therapy
MetroNIDAZOLE (Systemic): May increase the serum concentration of Vitamin K Antagonists. Management: Consider alternatives to concomitant therapy with these agents. If concomitant therapy cannot be avoided, consider reducing the dose of the vitamin K antagonist and monitor for increased INR/bleeding. Consider therapy modification
Miconazole (Oral): May increase the serum concentration of Warfarin. Monitor therapy
Miconazole (Topical): May increase the serum concentration of Vitamin K Antagonists. Consider therapy modification
MiFEPRIStone: May enhance the adverse/toxic effect of Anticoagulants. Specifically, the risk of bleeding may be increased. Avoid combination
Milnacipran: May enhance the adverse/toxic effect of Vitamin K Antagonists. Specifically, the risk for bleeding may be increased. Monitor therapy
Mirtazapine: May enhance the anticoagulant effect of Warfarin. Monitor therapy
Multivitamins/Fluoride (with ADE): May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the anticoagulant effect of Vitamin K Antagonists. Multivitamins/Minerals (with ADEK, Folate, Iron) may diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Nafcillin: May diminish the anticoagulant effect of Vitamin K Antagonists. Management: Consider choosing an alternative antibiotic. Monitor for decreased therapeutic effects and need for dose adjustments of oral anticoagulants if nafcillin is initiated/dose increased, or increased effects if nafcillin is discontinued/dose decreased. Consider therapy modification
Nelfinavir: May decrease the serum concentration of Warfarin. Nelfinavir may increase the serum concentration of Warfarin. Monitor therapy
Neomycin: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Nevirapine: May diminish the anticoagulant effect of Warfarin. Monitor therapy
Nintedanib: Anticoagulants may enhance the adverse/toxic effect of Nintedanib. Specifically, the risk for bleeding may be increased. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (COX-2 Selective): May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents (Nonselective): May enhance the anticoagulant effect of Vitamin K Antagonists. Management: Consider alternatives to this combination when possible. If the combination must be used, monitor coagulation status closely and advise patients to promptly report any evidence of bleeding or bruising. Consider therapy modification
Obeticholic Acid: May diminish the anticoagulant effect of Warfarin. Monitor therapy
Obinutuzumab: Anticoagulants may enhance the adverse/toxic effect of Obinutuzumab. Specifically, the risk of serious bleeding-related events may be increased. Monitor therapy
Omacetaxine: Anticoagulants may enhance the adverse/toxic effect of Omacetaxine. Specifically, the risk for bleeding-related events may be increased. Management: Avoid concurrent use of anticoagulants with omacetaxine in patients with a platelet count of less than 50,000/uL. Avoid combination
Omega-3 Fatty Acids: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Omeprazole: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Oritavancin: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Oritavancin: May diminish the therapeutic effect of Anticoagulants. Specifically, oritavancin may artificially increase the results of laboratory tests commonly used to monitor anticoagulant effectiveness, which could lead to incorrect decisions to decrease anticoagulant doses. Monitor therapy
Orlistat: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Oxatomide: May enhance the anticoagulant effect of Vitamin K Antagonists. Avoid combination
Penicillins: May enhance the anticoagulant effect of Vitamin K Antagonists. Exceptions: Dicloxacillin; Nafcillin. Monitor therapy
Pentosan Polysulfate Sodium: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Pentoxifylline: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Phenytoin: May enhance the anticoagulant effect of Vitamin K Antagonists. Vitamin K Antagonists may increase the serum concentration of Phenytoin. Management: Anticoagulant dose adjustment will likely be necessary when phenytoin is initiated or discontinued. Monitor patients extra closely (INR and signs/symptoms of bleeding) when using this combination. Consider therapy modification
Phytonadione: May diminish the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Posaconazole: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Progestins: May diminish the therapeutic effect of Anticoagulants. More specifically, the potential prothrombotic effects of some progestins and progestin-estrogen combinations may counteract anticoagulant effects. Management: Carefully weigh the prospective benefits of progestins against the potential increased risk of procoagulant effects and thromboembolism. Use is considered contraindicated under some circumstances. Refer to related guidelines for specific recommendations. Consider therapy modification
Progestins (Contraceptive): May diminish the anticoagulant effect of Vitamin K Antagonists. In contrast, enhanced anticoagulant effects have also been noted with some products. Management: When possible, concomitant hormonal contraceptives and coumarin derivatives should be avoided in order to eliminate the risk of thromboembolic disorders. Consider using an alternative, nonhormonal contraceptive. Consider therapy modification
Proguanil: May enhance the anticoagulant effect of Warfarin. Monitor therapy
Propacetamol: May enhance the anticoagulant effect of Vitamin K Antagonists. This appears most likely with higher doses (equivalent to acetaminophen doses exceeding 1.3 to 2 g/day) for multiple consecutive days. Monitor therapy
Propafenone: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Prostacyclin Analogues: May enhance the adverse/toxic effect of Anticoagulants. Specifically, the antiplatelet effects of these agents may lead to an increased risk of bleeding with the combination. Monitor therapy
QuiNIDine: May enhance the anticoagulant effect of Vitamin K Antagonists. Note that the INR/PT might be unchanged in the face of increased bleeding. Monitor therapy
QuiNINE: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Quinolones: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
RaNITIdine: May increase the serum concentration of Warfarin. Monitor therapy
Regorafenib: Warfarin may enhance the adverse/toxic effect of Regorafenib. Specifically, the risk for bleeding may be increased. Monitor therapy
Revaprazan: May diminish the anticoagulant effect of Warfarin. Monitor therapy
Ribavirin (Systemic): May diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Rifamycin Derivatives: May increase the metabolism of Vitamin K Antagonists. Monitor therapy
Rifapentine: May decrease the serum concentration of CYP2C9 Substrates (High risk with Inducers). Monitor therapy
Ritonavir: May decrease the serum concentration of Warfarin. Monitor therapy
RomiDEPsin: May enhance the anticoagulant effect of Warfarin. Monitor therapy
Roxithromycin: May enhance the anticholinergic effect of Warfarin. Monitor therapy
Rucaparib: May increase the serum concentration of Warfarin. Monitor therapy
Salicylates: May enhance the anticoagulant effect of Vitamin K Antagonists. Exceptions: Salsalate. Consider therapy modification
Salicylates: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Salicylates (Topical): May enhance the anticoagulant effect of Warfarin. Monitor therapy
Saquinavir: May increase the serum concentration of Warfarin. Monitor therapy
Selective Serotonin Reuptake Inhibitors: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Sodium Zirconium Cyclosilicate: May increase the serum concentration of Warfarin. Management: Separate the administration of sodium zirconium cyclosilicate and warfarin by at least 2 hours. If simultaneous administration is required, monitor for signs and symptoms of warfarin toxicity (eg, elevated INR, bleeding). Consider therapy modification
SORAfenib: May enhance the anticoagulant effect of Warfarin. SORAfenib may increase the serum concentration of Warfarin. Management: Warfarin dose adjustment will likely be necessary. Increase frequency of INR monitoring during sorafenib therapy (particularly when starting or stopping therapy), and increase monitoring for signs and symptoms of bleeding. Consider therapy modification
St John's Wort: May increase the metabolism of Vitamin K Antagonists. Consider therapy modification
Streptokinase: May enhance the anticoagulant effect of Vitamin K Antagonists. Avoid combination
Sucralfate: May diminish the anticoagulant effect of Vitamin K Antagonists. Sucralfate may decrease the serum concentration of Vitamin K Antagonists. Specifically, sucralfate may decrease the absorption of Vitamin K Antagonists. Management: Administer vitamin K antagonists at least 2 hours before sucralfate. Consider therapy modification
Sugammadex: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Sulfinpyrazone: May decrease the metabolism of Vitamin K Antagonists. Sulfinpyrazone may decrease the protein binding of Vitamin K Antagonists. Consider therapy modification
Sulfonamide Antibiotics: May enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Sulfonylureas: May enhance the anticoagulant effect of Vitamin K Antagonists. Vitamin K Antagonists may enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Sulodexide: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Tamoxifen: May increase the serum concentration of Vitamin K Antagonists. Avoid combination
Telavancin: May diminish the therapeutic effect of Anticoagulants. Specifically, telavancin may artificially increase the results of laboratory tests commonly used to monitor anticoagulant effectiveness, which could lead to incorrect decisions to decrease anticoagulant doses. Monitor therapy
Teriflunomide: May decrease the serum concentration of Warfarin. Monitor therapy
Tetracyclines: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Tezacaftor and Ivacaftor: May increase the serum concentration of Warfarin. Monitor therapy
Thrombolytic Agents: May enhance the anticoagulant effect of Anticoagulants. Management: See full drug monograph for guidelines for the use of alteplase for acute ischemic stroke during treatment with oral anticoagulants. Monitor therapy
Thyroid Products: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Tibolone: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Tigecycline: May increase the serum concentration of Warfarin. Monitor therapy
Tipranavir: May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Tobacco (Smoked): May decrease the serum concentration of Warfarin. Monitor therapy
Tolterodine: May enhance the anticoagulant effect of Warfarin. Monitor therapy
Toremifene: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Torsemide: May increase the serum concentration of Warfarin. Monitor therapy
TraMADol: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Tranilast (Systemic): May enhance the adverse/toxic effect of Warfarin. Tranilast (Systemic) may diminish the therapeutic effect of Warfarin. Monitor therapy
TraZODone: May diminish the anticoagulant effect of Warfarin. Monitor therapy
Tricyclic Antidepressants: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Urokinase: May enhance the anticoagulant effect of Anticoagulants. Avoid combination
Valproate Products: May decrease the protein binding of Warfarin. Monitor therapy
Vemurafenib: May increase the serum concentration of Warfarin. Monitor therapy
Venetoclax: May increase the serum concentration of Warfarin. Monitor therapy
Venlafaxine: May enhance the adverse/toxic effect of Vitamin K Antagonists. Specifically, the risk for bleeding may be increased. Monitor therapy
Vitamin E (Systemic): May enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Vorapaxar: May enhance the adverse/toxic effect of Anticoagulants. More specifically, this combination is expected to increase the risk of bleeding. Avoid combination
Voriconazole: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Vorinostat: May enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Zafirlukast: May increase the serum concentration of Vitamin K Antagonists. Monitor therapy
Zanubrutinib: May enhance the adverse/toxic effect of Anticoagulants. Monitor therapy
Zileuton: May increase the serum concentration of Warfarin. Monitor therapy
Adverse Reactions
Bleeding is the major adverse effect of warfarin. Hemorrhage may occur at virtually any site. Risk is dependent on multiple variables, including the intensity of anticoagulation and patient susceptibility.
1% to 10%:
Hematologic & oncologic: Major hemorrhage (≤5%; INR 2.5 to 4.0 generally associated with more bleeding)
Frequency not defined:
Cardiovascular: Purple-toe syndrome, systemic cholesterol micro-embolism, vasculitis
Central nervous system: Chills
Dermatologic: Alopecia, bullous rash, dermatitis, pruritus, skin necrosis, urticaria
Gastrointestinal: Abdominal pain, bloating, diarrhea, dysgeusia, flatulence, nausea, vomiting
Hematologic & oncologic: Minor hemorrhage
Hepatic: Hepatitis
Hypersensitivity: Anaphylaxis, hypersensitivity reaction
Renal: Acute renal failure (in patients with altered glomerular integrity or with a history of kidney disease)
Respiratory: Tracheobronchial calcification
<1%, postmarketing, and/or case reports: Gangrene of skin or other tissue, skin necrosis, vascular calcification (calcium uremic arteriolopathy and calciphylaxis)
Warnings/Precautions
Concerns related to adverse effects:
- Acute kidney injury: Acute kidney injury, possibly as a result of episodes of excessive anticoagulation and hematuria, may occur in patients with a history of kidney disease or in patients with altered glomerular integrity.
- Anaphylaxis/hypersensitivity: May cause hypersensitivity reactions, including anaphylaxis; use with caution in patients with anaphylactic disorders.
- Bleeding: [US Boxed Warning]: May cause major or fatal bleeding. Perform regular INR monitoring in all treated patients. INR levels achieved with warfarin therapy may be affected by concomitant medication, dietary modifications and/or other factors (eg, smoking). Risk factors for bleeding include high intensity anticoagulation (INR >4), age (≥65 years), variable INRs, history of GI bleeding, hypertension, cerebrovascular disease, serious heart disease, anemia, severe diabetes, malignancy, trauma, renal insufficiency, polycythemia vera, vasculitis, open wound, history of PUD, indwelling catheters, menstruating and postpartum women, drug-drug interactions, long duration of therapy, or known genetic deficiency in CYP2C9 activity. Patient must be instructed to report bleeding, accidents, or falls as well as any new or discontinued medications, herbal or alternative products used, or significant changes in smoking or dietary habits. Unrecognized bleeding sites (eg, colon cancer) may be uncovered by anticoagulation.
- Calciphylaxis: Fatal and serious calciphylaxis (calcium uremic arteriolopathy) has been reported in patients with and without end-stage renal disease. If calciphylaxis is diagnosed, discontinue therapy and treat calciphylaxis as appropriate. Consider alternative anticoagulation therapy.
- Skin necrosis/gangrene: Necrosis or gangrene of the skin and other tissue can occur (rarely, <0.1%) due to paradoxical local thrombosis; onset is usually within the first few days of therapy and is frequently localized to the limbs, breast, or penis. The risk of this effect is increased in patients with protein C or S deficiency. Consider alternative therapies if anticoagulation is necessary.
- Atheroemboli/cholesterol microemboli: Warfarin therapy may release atheromatous plaque emboli; symptoms depend on site of embolization, most commonly kidneys, pancreas, liver, and spleen. In some cases may lead to necrosis or death. “Purple toe” syndrome, due to cholesterol microembolization, has been rarely described with coumarin-type anticoagulants. Typically, this occurs after several weeks of therapy, and may present as a dark, purplish, mottled discoloration of the plantar and lateral surfaces. Other manifestations of cholesterol microembolization may include rash; livedo reticularis; gangrene; abrupt and intense pain in lower extremities; abdominal, flank, or back pain; hematuria, renal insufficiency; hypertension; cerebral ischemia; spinal cord infarction; or other symptoms of vascular compromise.
Disease-related concerns:
- Bariatric surgery: High risk for hemorrhage postsurgery: Avoid warfarin if possible immediately after gastric bypass and sleeve gastrectomy; significant risk for hemorrhage, readmission, and mortality (Bechtel 2013). Several studies have observed warfarin dose reduction postoperatively with a subsequent return to preoperative doses 6 to 12 months after surgery (Irwan 2013; Schullo-Feulner 2014; Steffen 2015; Strong 2018). The change in dose requirement may be multifactorial but is most likely due to attributable variation in the time to resuming full solid intake and the consequent alteration in the intake of vitamin K-containing foods. Monitor INR closely in the early postoperative period and up to 1 year after surgery or when significant nutritional or supplementation changes occur.
- Dietary insufficiency: Use with caution in patients with prolonged dietary insufficiencies (vitamin K deficiency).
- Heparin-induced thrombocytopenia: Use with caution in patients with heparin-induced thrombocytopenia and venous thromboembolism; limb ischemia, necrosis, and gangrene have occurred when warfarin was started or continued after heparin was stopped. Warfarin monotherapy is contraindicated in the initial treatment of heparin-induced thrombocytopenia; warfarin initially inhibits the synthesis of protein C, potentially accelerating the underlying active thrombotic process.
- Hepatic impairment: Reduced liver function, regardless of etiology, may impair synthesis of coagulation factors leading to increased warfarin sensitivity.
- Infection: Use with caution in patients with acute infection or active TB or any disruption of normal GI flora; antibiotics and fever may alter response to warfarin.
- Renal impairment: Use with caution in patients with renal impairment. Patients with renal impairment are at increased risk for bleeding diathesis; frequent INR monitoring is recommended.
- Thyroid disease: Use with caution in patients with thyroid disease; warfarin responsiveness may increase (ACCP [Ageno 2012]).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: The elderly may be more sensitive to anticoagulant therapy.
- Patients with genomic variants in CYP2C9 and/or VKORC1: Presence of the CYP2C9*2 or *3 allele and/or polymorphism of the vitamin K oxidoreductase (VKORC1) gene may have increased sensitivity to warfarin (eg, lower doses needed to achieve therapeutic anticoagulation). The *2 allele is reported to occur with a frequency of 4% to 11% in African-Americans and Caucasians, respectively, while the *3 allele frequencies are 2% to 7% respectively. Other variant 2C9 alleles (eg, *5, *6, *9, and *11) are also associated with reduced warfarin metabolism and thus may increase sensitivity to warfarin, but are much less common. Lower doses may be required in these patients. Genetic testing may help determine appropriate dosing.
Other warnings/precautions:
- Appropriate use: Surgical patients: When temporary interruption is necessary before surgery, discontinue for approximately 5 days before surgery; when there is adequate hemostasis, may reinstitute warfarin therapy ~12 to 24 hours after surgery. Decision to safely continue warfarin therapy through the procedure and whether or not bridging of anticoagulation is necessary is dependent upon risk of perioperative bleeding and risk of thromboembolism. If risk of thromboembolism is elevated, consider bridging warfarin therapy with an alternative anticoagulant (eg, unfractionated heparin or low-molecular-weight heparin) (ACCP [Ageno 2012]).
- Patient selection: Use care in the selection of patients appropriate for this treatment; ensure patient cooperation especially from the alcoholic, illicit drug user, demented, or psychotic patient; ability to comply with routine laboratory monitoring is essential.
Monitoring Parameters
Prothrombin time, INR; hematocrit; may consider genotyping of CYP2C9 and VKORC1 prior to initiation of therapy; however, routine genetic testing is not recommended (ACCP [Holbrook 2012]; CPIC [Johnson 2017]).
Frequency of INR monitoring: During warfarin initiation, monitor INR daily for hospitalized patients and every 1 to 3 days for nonhospitalized patients. After initiating warfarin therapy, INR should be monitored every 2 to 3 days during the first week of therapy. Once a stable response to therapy is achieved, INR monitoring may be performed less frequently: once a week for the first 1 to 2 weeks, then every 2 weeks, and eventually monthly thereafter. Very stable and reliable patients may have their monitoring extended up to every 12 weeks (Wittkowsky 2018).
|
Initiation of therapy |
Frequency of monitoring |
|---|---|
|
aThese example suggestions should not replace clinical judgment; more frequent monitoring may be necessary. |
|
|
Inpatient initiation |
Daily. |
|
After hospital discharge |
If stable, within 3 to 5 days. If unstable, within 1 to 3 days. |
|
Outpatient flexible initiation |
Daily through day 4, then within 3 to 5 days. |
|
Outpatient average daily dosing method |
Every 3 to 5 days until INR reaches lower limit of therapeutic range, then within 1 week. |
|
First month of therapy |
At least weekly. |
|
Maintenance therapy |
Frequency of monitoring |
|
Medically stable inpatients |
Every 1 to 3 days. |
|
Medically unstable inpatients |
Daily. |
|
After hospital discharge |
If stable, within 3 to 5 days. If unstable, within 1 to 3 days. |
|
Routine follow-up in medically stable and reliable patients |
Every 4 to 12 weeks. |
|
Routine follow-up in medically unstable or unreliable patients |
Every 1 to 2 weeks. |
|
Dose held today for significant over-anticoagulation |
Recheck in 1 to 2 days. |
|
Dosage adjustment today |
Recheck within 1 to 2 weeks. |
|
Dosage adjustment ≤2 weeks ago |
Recheck within 2 to 4 weeks. |
Pregnancy
Pregnancy Considerations
Warfarin crosses the placenta; concentrations in the fetal plasma are similar to maternal values. Teratogenic effects have been reported following first trimester exposure and may include coumarin embryopathy (nasal hypoplasia and/or stippled epiphyses; limb hypoplasia may also be present). Adverse CNS events to the fetus have also been observed following exposure during any trimester and may include CNS abnormalities (including ventral midline dysplasia, dorsal midline dysplasia). Spontaneous abortion, fetal hemorrhage, and fetal death may also occur. Use is contraindicated during pregnancy except in women with mechanical heart valves who are at high risk for thromboembolism; use is also contraindicated in women with threatened abortion, eclampsia, or preeclampsia. Frequent pregnancy tests are recommended for women who are planning to become pregnant and adjusted-dose heparin or low molecular weight heparin (LMWH) should be substituted as soon as pregnancy is confirmed or adjusted-dose heparin or LMWH should be used instead of warfarin prior to conception.
In pregnant women with high-risk mechanical heart valves, the benefits of warfarin therapy should be discussed with the risks of available treatments (ACCP [Bates 2012]; AHA/ACC [Nishimura 2014]); when possible avoid warfarin use during the first trimester (ACCP [Bates 2012]) and close to delivery (ACCP [Bates 2012]; AHA/ACC [Nishimura 2014]). Use of warfarin during the first trimester may be considered if the therapeutic INR can be achieved with a dose ≤5 mg/day (AHA/ACC [Nishimura 2014]). Adjusted-dose LMWH or adjusted-dose heparin may be used throughout pregnancy or until week 13 of gestation when therapy can be changed to warfarin. LMWH or heparin should be resumed close to delivery. In women who are at a very high risk for thromboembolism (older generation mechanical prosthesis in mitral position or history of thromboembolism), warfarin can be used throughout pregnancy and replaced with LMWH or heparin near term; the use of low-dose aspirin is also recommended (ACCP [Bates 2012] AHA/ACC [Nishimura 2014]). Women who require long-term anticoagulation with warfarin and who are considering pregnancy, LMWH substitution should be done prior to conception when possible. If anti-Xa monitoring cannot be done, do not use LMWH therapy in pregnant patients with a mechanical prosthetic valve (AHA/ACC [Nishimura 2014]). When choosing therapy, fetal outcomes (ie, pregnancy loss, malformations), maternal outcomes (ie, VTE, hemorrhage), burden of therapy, and maternal preference should be considered (ACCP [Bates 2012]).
Evaluate pregnancy status prior to use in females of reproductive potential. Females of reproductive potential should use effective contraception during therapy and for 1 month after the last dose.
Patient Education
What is this drug used for?
- It is used to treat blood clots.
- It is used to thin the blood so that clots will not form.
- It is used to lower the chance of heart attack, stroke, and death in some people.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes.
- DVT like edema, warmth, numbness, change in color, or pain in the extremities.
- Chest pain
- Severe dizziness
- Passing out
- Edema
- Severe headache
- Skin discoloration to black or purple
- Body temperature change
- Pain
- Severe loss of strength and energy
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.
Patient Education
What is this drug used for?
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.