What is depression?
Depression is a common mood disorder, which has a negative impact on the way you think, feel and act. It can affect your ability to function in everyday life and can also have a significant impact on you and those around you.
Types of depression
Depression is also known as major depressive disorder or clinical depression. There are also several other subtypes or types of depressive disorders including:
- Persistent depressive disorder (dysthymia) - is a depressive mood that lasts for more than two years. Symptoms can vary and include major depressive episodes and periods of less severe symptoms.
- Atypical depression (major depression or dysthymia with atypical features) - is a type of major depressive disorder that is associated with atypical symptoms of depression.
- Melancholic depression (major depression with melancholic features) - is a type of major depressive disorder that is associated with melancholic symptoms.
- Catatonic depression - is a type of major depressive disorder that affects motor skills, resulting in changes in the way you speak or move. A person in a catatonic state usually lacks the ability to speak or move.
- Postpartum depression - episodes of major depression during pregnancy or following delivery.
- Psychotic depression - episodes of severe depression experienced alongside some form of psychosis, such as hallucinations or delusions of guilt, poverty or illness.
- Seasonal affective disorder - episodes of depressive symptoms that begin during winter when there is less natural sunlight. Symptoms typically lift during the warmer, sunnier months.
- Bipolar disorder (manic depression) - strictly speaking this is not just a type of depression. People with bipolar disorder experience episodes of major depression, referred to as bipolar depression, but also have episodes of extreme highs associated with a manic mood.
- Disruptive mood dysregulation disorder - affects children and adolescents, causing chronic irritability associated with frequent and severe temper tantrums that seem out of proportion for the situation.
- Premenstrual dysphoric disorder (PMDD) - similar to premenstrual syndrome (PMS), but PMDD is associated with severe depression, anxiety and irritability in the week or two before a period starts and for the first two to three days.
What causes depression?
Depression can affect anyone and a variety of factors may contribute to the development of this medical condition. Some factors may simply make you more susceptible to this condition, while others are stressors or triggers that may cause actual symptoms to develop.
It is not uncommon for several factors to play a role in the development of depression, including factors in these 4 key areas:
- Environmental and lifestyle factors - people exposed to ongoing abuse, poverty, violence or neglect can be more at risk. Overwork, poor diet, lack of exercise and sleep, as well as alcohol and drug abuse problems can also contribute. Factors, such as a bereavement, job loss, divorce or other traumatic events and natural disasters may also trigger this condition in vulnerable individuals
- Genetics - depression is well-known to run in families and is 1.5-3 times more common in first-degree biological relatives of affected individuals than it is among those less closely related. If one identical twin has this condition then 76 percent of the time the other twin will too. In fraternal twins this figure drops to 19 percent.
- Biochemistry - certain chemicals in the brain can play a role in the development of depression. Chemicals called neurotransmitters act as messengers in the brain allowing different areas to communicate with each other via a system of neurons or nerve cells. This process is essential for the brain to function. Problems or an imbalance in certain neurotransmitters, such as serotonin, norepinephrine (noradrenaline), dopamine and glutamate, has been associated with this condition.
- Personality - Certain personality traits are known to contribute to the development of depression. Traits associated with neurotic or extrovert behavior, or conscientiousness have been linked to this condition.
Other factors that put you at risk include:
- Having certain illnesses, especially chronic conditions, including sleep disorders, anxiety, chronic pain, arthritis, cancer, diabetes, heart disease and others
- Taking certain medications including some drugs used to treat high blood pressure, acne, and migraines. Use of corticosteroids, hormone-based medications, certain smoking cessation aids and other medications may also put a person at increased risk
- Being female - depression is more common in women
- Having a low level of education
- Living without a partner
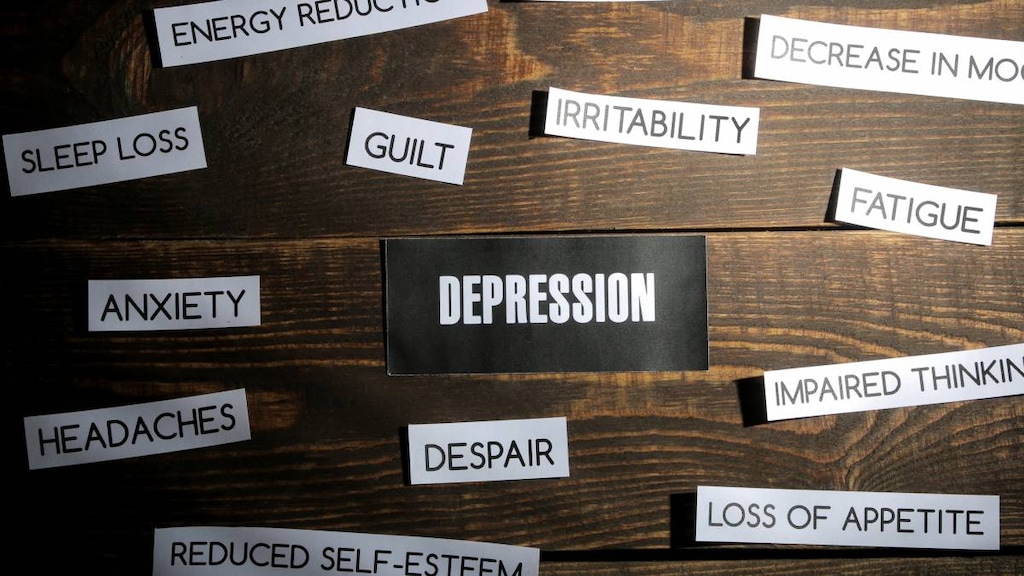
What are the symptoms of depression?
Signs and symptoms of depression range from mild to severe and include:
- Depressed mood or feeling sad
- Loss of interest or pleasure in activities that were enjoyable
- Changes in appetite or weight - weight loss or gain unrelated to dieting
- Sleeping troubles including having trouble falling asleep and/or staying asleep (insomnia), feeling excessively sleepy during the day (hypersomnia), or sleeping too much
- Increased purposeless physical activity or slowed movements and thoughts including restless symptoms, inability to sit still, pacing, handwringing, a slowing down of thoughts, actions or speech
- Fatigue or loss of energy
- Feeling worthless and guilty
- Difficulty concentrating, thinking or making decisions
- Thoughts of suicide or death
Other atypical symptoms of this condition include overeating, sleeping too much (hypersomnia), limbs feeling heavy and weighed down (leaden paralysis) and being very sensitive to rejection.
Depression, sadness and grief
Depression is more than just feelings of sadness or grief. It should not be confused with sadness and grief, which are common feelings people experience after losing a loved one or a job, for example.
Grief and depression do share some of the same symptoms, but there are important differences. People suffering from grief may find that painful feelings come in waves - as the sadness at remembering a loss is interspersed with happy memories of a person or event - whereas people suffering from depression experience their symptoms much of the time. Self-esteem is usually unaffected by grief, whereas feelings of worthlessness are commonly felt by those with depression. People suffering from grief may also think about death, but rather than thinking about how they can end their life, they may imagine ‘joining’ a loved one who has died.
A person can suffer from grief, sadness and depression all at the same time.
How is depression diagnosed?
The Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) is a handbook used by healthcare professionals that helps them to diagnose this condition and other mental disorders. It lists the criteria for assessing and diagnosing patients.
To be diagnosed with depression you must suffer from five or more of the symptoms in the bulleted list above and these must have been present during the same two-week period and be a change from previous functioning. At least one of the symptoms needs to be a depressed mood or loss of interest or pleasure.
The symptoms must cause clinically significant distress or impairments in social, work (occupational), or other important areas of functioning and must not be due to another medical condition or disorder.
How is depression treated?
Depression is treated using medication, psychotherapy and other options. A combination of different approaches is commonly used including:
- Antidepressant medications. Antidepressants are thought to work by changing the levels of neurotransmitters - chemical messengers in the brain. It may take 6-12 weeks of treatment before it feels as though an antidepressant medication is fully working, although some people will start to feel a benefit after 1-2 weeks. Most antidepressants come in tablet form.
A number of different types or classes of antidepressant medications are available including:- Selective Serotonin Reuptake Inhibitors (SSRI). Examples include Celexa (citalopram), Lexapro (escitalopram), Paxil (paroxetine), Prozac (fluoxetine) and Zoloft (sertraline).
- Serotonin and Norepinephrine Reuptake Inhibitors (SNRI). Examples include Cymbalta (duloxetine) and Effexor XR (venlafaxine).
- Tricyclic and Tetracyclic Antidepressants. Examples include amoxapine, amitriptyline, maprotiline, doxepin and Tofranil (imipramine).
- Atypical Antidepressants. Examples include trazodone, nefazodone, Remeron (mirtazapine), Wellbutrin SR and Wellbutrin XL (bupropion).
- Monoamine Oxidase Inhibitors (MAOIs). Examples include Emsam skin patch (selegiline), Marplan (isocarboxazid), Nardil (phenelzine) and Parnate (tranylcypromine).
- N-methyl D-aspartate (NMDA) Antagonist. Examples include Spravato nasal spray (esketamine).
- Neuroactive Steroid Gamma-Aminobutyric Acid (GABA)-A Receptor Positive Modulator. Examples include Zulresso intravenous (IV) infusion (brexanolone).
- Psychotherapies or interventions. A range of therapy options can be used including cognitive-behavioral therapy (CBT), mindfulness-based cognitive therapy, behavioral therapy, interpersonal psychotherapy (IPT), psychodynamic therapies and supportive therapy.
- Electroconvulsive therapy (ECT). ECT is a medical treatment used to treat severe depression that does not respond to other treatments. It involves brief electrical stimulation of the brain and it is performed on patients while they are under anesthesia.
- Complementary and alternative therapies. Add-on therapies, such as yoga and other types of exercise may help people with depression. Herbal remedies, such as St John’s Wort are also used. Consult your healthcare professional before taking herbal remedies.
- Light therapy. Light therapy is another treatment option that is used to help people with seasonal affective disorder.
Medication is usually recommended for at least six months after symptoms have improved and longer term treatment may be needed in some people. Treatments may cause side effects. Talk to your healthcare professional about the best treatment options for you.
What is the prognosis for depression?
The expected prognosis following a diagnosis varies from person to person.
An early diagnosis and response to treatment, mild symptoms, sticking to the treatment plan, having a good support network and previously good health are all associated with better outcomes.
Not receiving treatment, having a personality or psychiatric disorder, being admitted to hospital multiple times and advanced age when symptoms begin are all associated with worse outcomes.
Approximately two-thirds of people with depression will consider suicide and 10-15 percent of people with this condition will commit suicide.
This is a chronic condition that can recur. The recurrence rates after the first, second and third episodes are 50, 70 and 90 percent, respectively. Bipolar disorder may also eventually develop in 5-10 percent of people diagnosed with depression.
How is depression prevented?
A number of different strategies are used for prevention including educational interventions, support groups and psychotherapies, such as cognitive-behavioral therapy, mindfulness-based cognitive therapy and interpersonal psychotherapy. Psychotherapies have been found to have longer lasting effects than medications and are preferred by many people.
Taking care of yourself by getting adequate sleep, exercising, eating well and learning to manage stress also play an important role in preventing depression.
Where to get help
Contact your healthcare professional if you think you may have depression. Reach out to family and friends for support.
Lifeline network also provides free and confidential support 24/7 for people in distress. Call 988, text 988 or chat with the Suicide & Crisis Lifeline from anywhere in the US.
Article references
- American Psychiatric Association (APA). What Is Depression? October 2020. Available at: https://www.psychiatry.org/patients-families/depression/what-is-depression. [Accessed April 6, 2021].
- Anxiety & Depression Association of America (ADAA). Depression. Available at: https://adaa.org/understanding-anxiety/depression. [Accessed April 6, 2021].
- National Institute of Mental Health (NIMH). Depression. February 2018. Available at: https://www.nimh.nih.gov/health/topics/depression/index.shtml. [Accessed April 6, 2021].
- Child Mind Institute. Disruptive Mood Dysregulation Disorder Basics. Available at: https://childmind.org/guide/guide-to-disruptive-mood-dysregulation-disorder/. [Accessed April 6, 2021].
- Office on Women’s Health (OAWH), US Department of Health & Human Services. Premenstrual dysphoric disorder (PMDD). Available at: https://www.womenshealth.gov/menstrual-cycle/premenstrual-syndrome/premenstrual-dysphoric-disorder-pmdd. [Accessed April 6, 2021].
- Łojko D, Rybakowski JK. Atypical depression: current perspectives. Neuropsychiatr Dis Treat. 2017;13:2447-2456. Published 2017 Sep 20. doi:10.2147/NDT.S147317.
- MentalHelp.net. Lifestyle Factors and Environmental Causes of Major Depression. Available at: https://www.mentalhelp.net/depression/environmental-causes/. [Accessed April 6, 2021].
- MentalHelp.net. Biology of Depression - Genetics and Imaging. Available at: https://www.mentalhelp.net/depression/biology-genetics-and-imaging/. [Accessed April 6, 2021].
- Resources to Recover. Catatonic Depression: Signs, Causes, and Recovery. August 7, 2019. Available at: https://www.rtor.org/2019/08/07/catatonic-depression-signs-and-causes/. [Accessed April 6, 2021].
- MentalHelp.net. Biology of Depression - Neurotransmitters. Available at: https://www.mentalhelp.net/depression/biology-of-depression-neurotransmitters/. [Accessed April 6, 2021].
- Klein DN, Kotov R, Bufferd SJ. Personality and depression: explanatory models and review of the evidence. Annu Rev Clin Psychol. 2011;7:269-295. doi:10.1146/annurev-clinpsy-032210-104540.
- Quitkin FM. Depression With Atypical Features: Diagnostic Validity, Prevalence, and Treatment. Prim Care Companion J Clin Psychiatry. 2002;4(3):94-99. doi:10.4088/pcc.v04n0302.
- American Psychological Association (APA). Clinical Practice Guideline for the Treatment of Depression Across Three Age Cohorts. American Psychological Association. Guideline Development Panel for the Treatment of Depressive Disorders. February 16, 2019. Available at: https://www.apa.org/depression-guideline/guideline.pdf. [Accessed April 6, 2021].
- Food and Drug Administration (FDA). Depression Medicines. November 18, 2019. Available at: https://www.fda.gov/consumers/free-publications-women/depression-medicines#. [Accessed April 6, 2021].
- Cipriani A, Furukawa TA, Salanti G, et al. Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis. Lancet. 2018;391(10128):1357-1366. doi:10.1016/S0140-6736(17)32802-7.
- Cuijpers P, Quero S, Dowrick C, Arroll B. Psychological Treatment of Depression in Primary Care: Recent Developments. Curr Psychiatry Rep. 2019;21(12):129. Published 2019 Nov 23. doi:10.1007/s11920-019-1117-x.
- American Psychiatric Association (APA). What is Electroconvulsive therapy (ECT). Available at: https://www.psychiatry.org/patients-families/ect. [Accessed April 6, 2021].
- Cochrane. Exercise for depression. September 12, 2013. Available at: https://www.cochrane.org/CD004366/DEPRESSN_exercise-for-depression. [Accessed April 6, 2021].
- Kvam S, Kleppe CL, Nordhus IH, Hovland A. Exercise as a treatment for depression: A meta-analysis. J Affect Disord. 2016;202:67-86. doi:10.1016/j.jad.2016.03.063.
- American Psychiatric Association (APA). Seasonal Affective Disorder (SAD). Available at: https://www.psychiatry.org/patients-families/depression/seasonal-affective-disorder. [Accessed April 6, 2021].
- National Institute of Mental Health, NIH. Depression. Available at: https://www.nimh.nih.gov/health/topics/depression/index.shtml. [Accessed April 6, 2021].
- Kraus C, Kadriu B, Lanzenberger R, Zarate CA Jr, Kasper S. Prognosis and improved outcomes in major depression: a review. Transl Psychiatry. 2019;9(1):127. Published 2019 Apr 3. doi:10.1038/s41398-019-0460-3.
- Dagnino P, Ugarte MJ, Morales F, González S, Saralegui D, Ehrenthal JC. Risk Factors for Adult Depression: Adverse Childhood Experiences and Personality Functioning. Front Psychol. 2020;11:594698. Published 2020 Dec 9. doi:10.3389/fpsyg.2020.594698.
- Hammen C. Risk Factors for Depression: An Autobiographical Review. Annu Rev Clin Psychol. 2018 May 7;14:1-28. doi: 10.1146/annurev-clinpsy-050817-084811. Epub 2018 Jan 12. PMID: 29328780.
- Semenkovich K, Chockalingam R, Scherrer JF, et al. Prescription Opioid Analgesics Increase Risk of Major Depression: New Evidence, Plausible Neurobiological Mechanisms and Management to Achieve Depression Prophylaxis. Mo Med. 2014;111(2):148-154.
- Rogers D, Pies R. General medical with depression drugs associated. Psychiatry (Edgmont). 2008;5(12):28-41.
- Global Consortium for the Prevention of Depression. Risk Factors. Available at: https://preventionofdepression.org/risk-factors/. [Accessed April 6, 2021].
- Global Consortium for the Prevention of Depression. List of Trials. Available at: https://preventionofdepression.org/list-of-trials/. [Accessed April 6, 2021].
- Bains N, Abdijadid S. Major Depressive Disorder. [Updated 2020 Oct 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559078/. [Accessed April 6, 2021].
- 999 Suicide & Crisis Lifeline. Home page. Available at: https://988lifeline.org/. [Accessed July 21, 2022].