Boxed Warning
Addiction, abuse, and misuse:
Tramadol/acetaminophen exposes patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient's risk prior to prescribing tramadol/acetaminophen, and monitor all patients regularly for the development of these behaviors and conditions.
Opioid analgesic risk evaluation and mitigation strategy (REMS)
To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the FDA has required a REMS for these products. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS-compliant education programs available to health care providers. Health care providers are strongly encouraged to complete a REMS-compliant education program; counsel patients and/or their caregivers, with every prescription, on safe use, serious risks, storage, and disposal of these products; emphasize to patients and their caregivers the importance of reading the Medication Guide every time it is provided by their pharmacist; and consider other tools to improve patient, household, and community safety.
Life-threatening respiratory depression:
Serious, life-threatening, or fatal respiratory depression may occur with use of tramadol. Monitor for respiratory depression, especially during initiation of tramadol/acetaminophen or following a dose increase.
Accidental ingestion:
Accidental ingestion of even one dose of tramadol/acetaminophen, especially by children, can result in a fatal overdose of tramadol.
Ultra-rapid metabolism of tramadol and other risk factors for life-threatening respiratory depression in children
Life-threatening respiratory depression and death have occurred in children who received tramadol. Some of the reported cases occurred following tonsillectomy and/or adenoidectomy; in at least 1 case, the child had evidence of being an ultra-rapid metabolizer of tramadol due to a CYP-450 2D6 polymorphism. Tramadol/acetaminophen is contraindicated in pediatric patients <12 years and in pediatric patients <18 years following tonsillectomy and/or adenoidectomy. Avoid the use of tramadol/acetaminophen in pediatric patients 12 to 18 years of age who have other risk factors that may increase their sensitivity to the respiratory depressant effects of tramadol.
Neonatal opioid withdrawal syndrome:
Prolonged use of tramadol/acetaminophen during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available.
Cytochrome P450 interactions:
The effects of concomitant use or discontinuation of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with tramadol are complex. Use of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with tramadol/acetaminophen requires careful consideration of the effects on the parent drug, tramadol, and the active metabolite, M1.
Hepatotoxicity:
Acetaminophen has been associated with cases of acute liver failure, at times resulting in liver transplant and death. Most of the cases of liver injury are associated with the use of acetaminophen at doses that exceed 4 g/day, and often involve more than one acetaminophen-containing product.
Risks from concomitant use with benzodiazepines or other CNS depressants:
Concomitant use of opioids with benzodiazepines or other CNS depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of tramadol/acetaminophen and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Ultracet: Acetaminophen 325 mg and tramadol hydrochloride 37.5 mg [contains corn starch]
Generic: Acetaminophen 325 mg and tramadol hydrochloride 37.5 mg
Pharmacology
Mechanism of Action
Acetaminophen: Although not fully elucidated, the analgesic effects are believed to be due to activation of descending serotonergic inhibitory pathways in the CNS. Interactions with other nociceptive systems may be involved as well (Smith 2009). Antipyresis is produced from inhibition of the hypothalamic heat-regulating center.
Tramadol: Binds to μ-opiate receptors in the CNS causing inhibition of ascending pain pathways, altering the perception of and response to pain; also inhibits the reuptake of norepinephrine and serotonin, which also modifies the ascending pain pathway
Use: Labeled Indications
Pain management: Short-term (≤5 days) management of acute pain severe enough to require an opioid analgesic and for which alternative treatments are inadequate.
Limitations of use: Reserve tramadol/acetaminophen for use in patients for whom alternative treatment options (eg, nonopioid analgesics) are ineffective, not tolerated, or would be otherwise inadequate to provide sufficient management of pain.
Contraindications
Hypersensitivity to acetaminophen, tramadol, or any component of the formulation; pediatric patients <12 years; postoperative management in pediatric patients <18 years who have undergone tonsillectomy and/or adenoidectomy; significant respiratory depression; acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment; GI obstruction, including paralytic ileus (known or suspected); concomitant use with or within 14 days following MAO inhibitor therapy.
Documentation of allergenic cross-reactivity for opioids is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): Known or suspected mechanical GI obstruction (eg, bowel obstruction, strictures) or any disease/condition that affects bowel transit; suspected surgical abdomen (eg, acute appendicitis, pancreatitis); severe renal impairment (creatinine clearance <30 mL/minute); severe hepatic impairment (Child-Pugh class C); mild pain that can be managed with other pain medications; acute or severe bronchial asthma, chronic obstructive airway, or status asthmaticus; acute respiratory depression, hypercapnia, or cor pulmonale; acute alcoholism, delirium tremens, or seizure disorder; severe CNS depression, increased cerebrospinal or intracranial pressure, or head injury; any situation where opioids are contraindicated (eg, acute intoxication with alcohol, hypnotics, centrally acting analgesics, opioids or psychotropic drugs); breastfeeding; pregnancy; use during labor and delivery.
Dosage and Administration
Dosing: Adult
Pain management: Oral: Acetaminophen 325 mg/tramadol 37.5 mg: Two tablets every 4 to 6 hours as needed for pain relief (maximum: 8 tablets/day [acetaminophen 2,600 mg/tramadol 300 mg per day]); do not exceed 5 days of therapy
Discontinuation of therapy: If discontinuing in a physically dependent patient, decrease the dose by no more than 10% to 25% and use a gradual downward titration. If patient displays withdrawal symptoms, temporarily interrupt the taper or increase dose to previous dose and then reduce dose more slowly by increasing interval between dose reductions, decreasing amount of daily dose reduction, or both.
Dosing: Geriatric
Refer to adult dosing. Use with caution.
Storage
Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
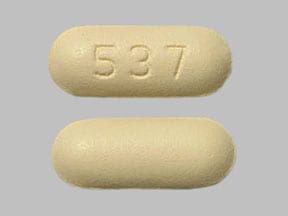
Acetaminophen and Tramadol Images
Drug Interactions
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Almotriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Alvimopan: Opioid Agonists may enhance the adverse/toxic effect of Alvimopan. This is most notable for patients receiving long-term (i.e., more than 7 days) opiates prior to alvimopan initiation. Management: Alvimopan is contraindicated in patients receiving therapeutic doses of opioids for more than 7 consecutive days immediately prior to alvimopan initiation. Consider therapy modification
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Amphetamines: May enhance the analgesic effect of Opioid Agonists. Monitor therapy
Amphetamines: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Anticholinergic Agents: May enhance the adverse/toxic effect of Opioid Agonists. Specifically, the risk for constipation and urinary retention may be increased with this combination. Monitor therapy
Antiemetics (5HT3 Antagonists): May enhance the serotonergic effect of TraMADol. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Ondansetron. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
BuPROPion: May enhance the neuroexcitatory and/or seizure-potentiating effect of Agents With Seizure Threshold Lowering Potential. Monitor therapy
BusPIRone: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Busulfan: Acetaminophen may increase the serum concentration of Busulfan. Monitor therapy
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
CarBAMazepine: TraMADol may enhance the CNS depressant effect of CarBAMazepine. TraMADol may diminish the therapeutic effect of CarBAMazepine. CarBAMazepine may decrease the serum concentration of TraMADol. Avoid combination
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
CNS Depressants: May enhance the CNS depressant effect of Opioid Agonists. Management: Avoid concomitant use of opioid agonists and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
CYP2D6 Inhibitors (Moderate): May diminish the therapeutic effect of TraMADol. These CYP2D6 inhibitors may prevent the metabolic conversion of tramadol to its active metabolite that accounts for much of its opioid-like effects. Exceptions: DULoxetine; Lorcaserin. Monitor therapy
CYP2D6 Inhibitors (Strong): May diminish the therapeutic effect of TraMADol. CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of TraMADol. CYP2D6 Inhibitors (Strong) may increase the serum concentration of TraMADol. Exceptions: FLUoxetine; PARoxetine. Monitor therapy
CYP3A4 Inducers (Moderate): May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of TraMADol. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of TraMADol. Exceptions: Nefazodone. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Dapoxetine: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Do not use serotonergic agents (high risk) with dapoxetine or within 7 days of serotonergic agent discontinuation. Do not use dapoxetine within 14 days of monoamine oxidase inhibitor use. Dapoxetine labeling lists this combination as contraindicated. Avoid combination
Dapsone (Topical): May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Monitor therapy
Dasatinib: Acetaminophen may enhance the hepatotoxic effect of Dasatinib. Dasatinib may increase the serum concentration of Acetaminophen. Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Desmopressin: Opioid Agonists may enhance the adverse/toxic effect of Desmopressin. Monitor therapy
Dexmethylphenidate-Methylphenidate: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Dextromethorphan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Diuretics: Opioid Agonists may enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
DULoxetine: May enhance the adverse/toxic effect of TraMADol. The risk for serotonin syndrome/serotonin toxicity and seizures may be increased with this combination. DULoxetine may diminish the therapeutic effect of TraMADol. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes), reduced tramadol effectiveness and seizures if these agents are combined. Monitor therapy
Eletriptan: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Eluxadoline: Opioid Agonists may enhance the constipating effect of Eluxadoline. Avoid combination
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Ergot Derivatives: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Nicergoline. Monitor therapy
Flucloxacillin: May enhance the adverse/toxic effect of Acetaminophen. Specifically, the risk for high anion gap metabolic acidosis may be increased. Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
Fosphenytoin-Phenytoin: May decrease the serum concentration of Acetaminophen. Specifically, serum concentrations of acetaminophen may be decreased (leading to decreased efficacy), but the formation of the toxic N-acetyl-p-benzoquinone imine (NAPQI) metabolite may be increased (leading to increased hepatotoxicity). Monitor therapy
Gastrointestinal Agents (Prokinetic): Opioid Agonists may diminish the therapeutic effect of Gastrointestinal Agents (Prokinetic). Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Imatinib: Acetaminophen may enhance the hepatotoxic effect of Imatinib. Monitor therapy
Iobenguane Radiopharmaceutical Products: TraMADol may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer tramadol until at least 7 days after each iobenguane dose. Avoid combination
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Isoniazid: May enhance the adverse/toxic effect of Acetaminophen. Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Linezolid: May enhance the serotonergic effect of Serotonergic Opioids (High Risk). This could result in serotonin syndrome. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes). Consider therapy modification
Local Anesthetics: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Local Anesthetics. Specifically, the risk for methemoglobinemia may be increased. Monitor therapy
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lorcaserin: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
Methylene Blue: May enhance the serotonergic effect of Serotonergic Opioids (High Risk). This could result in serotonin syndrome. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes). Consider therapy modification
MetyraPONE: May increase the serum concentration of Acetaminophen. More importantly, by inhibiting the conjugative metabolism of acetaminophen, metyrapone may shift the metabolism towards the oxidative route that produces a hepatotoxic metabolite. Monitor therapy
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mipomersen: Acetaminophen may enhance the hepatotoxic effect of Mipomersen. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Monoamine Oxidase Inhibitors (Antidepressant): May enhance the adverse/toxic effect of TraMADol. Specifically, the risk for serotonin syndrome/serotonin toxicity and seizures may be increased.. Avoid combination
Monoamine Oxidase Inhibitors (Type B): Serotonergic Opioids (High Risk) may enhance the serotonergic effect of Monoamine Oxidase Inhibitors (Type B). This could result in serotonin syndrome. Avoid combination
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Nalmefene: May diminish the therapeutic effect of Opioid Agonists. Management: Avoid the concomitant use of nalmefene and opioid agonists. Discontinue nalmefene 1 week prior to any anticipated use of opioid agonistss. If combined, larger doses of opioid agonists will likely be required. Consider therapy modification
Naltrexone: May diminish the therapeutic effect of Opioid Agonists. Management: Seek therapeutic alternatives to opioids. See full drug interaction monograph for detailed recommendations. Consider therapy modification
Nefazodone: May enhance the adverse/toxic effect of TraMADol. Specifically, the risk for serotonin syndrome/serotonin toxicity and seizures may be increased. Nefazodone may increase the serum concentration of TraMADol. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes), seizures, and tramadol adverse effects when these agents are combined. Monitor therapy
Nitric Oxide: May enhance the adverse/toxic effect of Methemoglobinemia Associated Agents. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Ondansetron: May enhance the serotonergic effect of TraMADol. This could result in serotonin syndrome. Ondansetron may diminish the therapeutic effect of TraMADol. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and diminished tramadol efficacy when these agents are combined. Monitor therapy
Opioids (Mixed Agonist / Antagonist): May diminish the analgesic effect of Opioid Agonists. Management: Seek alternatives to mixed agonist/antagonist opioids in patients receiving pure opioid agonists, and monitor for symptoms of therapeutic failure/high dose requirements (or withdrawal in opioid-dependent patients) if patients receive these combinations. Avoid combination
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxitriptan: Serotonergic Agents (High Risk) may enhance the serotonergic effect of Oxitriptan. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Pegvisomant: Opioid Agonists may diminish the therapeutic effect of Pegvisomant. Monitor therapy
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
PHENobarbital: May enhance the CNS depressant effect of TraMADol. PHENobarbital may decrease the serum concentration of TraMADol. Management: Avoid use of tramadol and phenobarbital when possible. Monitor for respiratory depression/sedation. Because phenobarbital is also a strong CYP3A4 inducer, monitor for decreased tramadol efficacy and withdrawal if combined. Consider therapy modification
Phenylephrine (Systemic): Acetaminophen may increase the serum concentration of Phenylephrine (Systemic). Monitor therapy
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
Prilocaine: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Prilocaine. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Management: Monitor patients for signs of methemoglobinemia (e.g., hypoxia, cyanosis) when prilocaine is used in combination with other agents associated with development of methemoglobinemia. Avoid lidocaine/prilocaine in infants receiving such agents. Monitor therapy
Primidone: May enhance the CNS depressant effect of TraMADol. Primidone may decrease the serum concentration of TraMADol. Management: Avoid use of tramadol and primidone when possible. Monitor for respiratory depression/sedation. Because primidone is also a strong CYP3A4 inducer, monitor for decreased tramadol efficacy and withdrawal if combined. Consider therapy modification
Probenecid: May increase the serum concentration of Acetaminophen. Probenecid may also limit the formation of at least one major non-toxic metabolite, possibly increasing the potential for formation of the toxic NAPQI metabolite. Consider therapy modification
Ramosetron: Opioid Agonists may enhance the constipating effect of Ramosetron. Monitor therapy
Ritonavir: May decrease serum concentrations of the active metabolite(s) of TraMADol. Ritonavir may increase the serum concentration of TraMADol. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: TraMADol may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk for serotonin syndrome/serotonin toxicity and seizures may be increased. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and seizures when these agents are combined. Exceptions: Dapoxetine; FLUoxetine; PARoxetine. Monitor therapy
Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors): May enhance the adverse/toxic effect of TraMADol. Specifically, the risk for serotonin syndrome/serotonin toxicity and seizures may be increased. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may diminish the therapeutic effect of TraMADol. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes), seizures, and decreased tramadol efficacy when these agents are combined. Monitor therapy
Serotonergic Agents (High Risk, Miscellaneous): Serotonergic Opioids (High Risk) may enhance the serotonergic effect of Serotonergic Agents (High Risk, Miscellaneous). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) if these agents are combined. Monitor therapy
Serotonergic Non-Opioid CNS Depressants: May enhance the CNS depressant effect of Serotonergic Opioids (High Risk). Serotonergic Non-Opioid CNS Depressants may enhance the serotonergic effect of Serotonergic Opioids (High Risk). This could result in serotonin syndrome. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity and CNS depression. Consider therapy modification
Serotonergic Opioids (High Risk): May enhance the CNS depressant effect of TraMADol. Serotonergic Opioids (High Risk) may enhance the serotonergic effect of TraMADol. This could result in serotonin syndrome. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity and CNS depression. Exceptions: TraMADol. Consider therapy modification
Serotonin 5-HT1D Receptor Agonists (Triptans): May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Almotriptan; Eletriptan. Monitor therapy
Serotonin/Norepinephrine Reuptake Inhibitors: May enhance the adverse/toxic effect of TraMADol. Specifically, the risk for serotonin syndrome/serotonin toxicity and seizures may be increased. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and seizures when these agents are combined. Exceptions: DULoxetine. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Sincalide: Drugs that Affect Gallbladder Function may diminish the therapeutic effect of Sincalide. Management: Consider discontinuing drugs that may affect gallbladder motility prior to the use of sincalide to stimulate gallbladder contraction. Consider therapy modification
Sodium Nitrite: Methemoglobinemia Associated Agents may enhance the adverse/toxic effect of Sodium Nitrite. Combinations of these agents may increase the likelihood of significant methemoglobinemia. Monitor therapy
Sodium Oxybate: May enhance the CNS depressant effect of CNS Depressants. Management: Consider alternatives to combined use. When combined use is needed, consider minimizing doses of one or more drugs. Use of sodium oxybate with alcohol or sedative hypnotics is contraindicated. Consider therapy modification
SORAfenib: Acetaminophen may enhance the hepatotoxic effect of SORAfenib. SORAfenib may increase the serum concentration of Acetaminophen. Consider therapy modification
St John's Wort: May enhance the serotonergic effect of TraMADol. This could result in serotonin syndrome. St John's Wort may decrease the serum concentration of TraMADol. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity and reduced tramadol effects (including withdrawal symptoms) when combined. Monitor for increased tramadol effects if St John's wort is discontinued. Monitor therapy
Succinylcholine: May enhance the bradycardic effect of Opioid Agonists. Monitor therapy
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Syrian Rue: May enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Monitor therapy
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Tricyclic Antidepressants: May enhance the CNS depressant effect of Serotonergic Opioids (High Risk). Serotonergic Opioids (High Risk) may enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Management: Consider alternatives to this drug combination. If combined, monitor for signs and symptoms of serotonin syndrome/serotonin toxicity and CNS depression. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Acetaminophen may enhance the anticoagulant effect of Vitamin K Antagonists. This appears most likely with daily acetaminophen doses exceeding 1.3 or 2 g/day for multiple consecutive days. Monitor therapy
Vitamin K Antagonists (eg, warfarin): TraMADol may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Zolpidem: CNS Depressants may enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
Test Interactions
See individual agents.
Adverse Reactions
Also see individual agents.
1% to 10%:
Central nervous system: Drowsiness (6%), dizziness (3%), insomnia (2%), anxiety, confusion, euphoria, fatigue, headache, nervousness
Dermatologic: Diaphoresis (4%), pruritus (2%), skin rash
Endocrine & metabolic: Hot flash
Gastrointestinal: Constipation (6%), anorexia (3%), diarrhea (3%), nausea (3%), xerostomia (2%), abdominal pain, dyspepsia, flatulence, vomiting
Genitourinary: Prostatic disease (2%)
Neuromuscular & skeletal: Tremor, weakness
<1%, postmarketing, and/or case reports: Abnormality in thinking, albuminuria, amnesia, anemia, ataxia, cardiac arrhythmia, changes in liver function, chest pain, convulsions, depersonalization, depression, drug abuse, dysphagia, dyspnea, emotional lability, exacerbation of migraine headache, exacerbation of hypertension, hallucination, hypertension, hypertonia, hypotension, impotence, melena, migraine, muscle spasm, nightmares, oliguria, palpitations, paresthesia, rigors, stupor, syncope, tachycardia, tinnitus, tongue edema, urinary retention, urination disorder, vertigo, visual disturbance, weight loss, withdrawal syndrome (with abrupt discontinuation; includes anxiety, diarrhea, hallucinations [rare], nausea, pain, piloerection, rigors, sweating, and tremor; uncommon discontinuation symptoms may include severe anxiety, panic attacks, or paresthesia)
Warnings/Precautions
Concerns related to adverse effects:
- Anaphylactoid reactions: Serious anaphylactoid reactions (including rare fatalities) often following initial dosing have been reported. Pruritus, hives, bronchospasm, angioedema, toxic epidermal necrolysis (TEN), and Stevens-Johnson syndrome have also been reported with use. Previous anaphylactoid reactions to opioids may increase risks for similar reactions to tramadol. If anaphylaxis or other hypersensitivity occurs, discontinue permanently; do not rechallenge.
- CNS depression: May cause CNS depression, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Hepatotoxicity: [US Boxed Warning]: Acetaminophen has been associated with cases of acute liver failure, at times resulting in liver transplant and death. Most of the cases of liver injury are associated with the use of acetaminophen at doses that exceed >4 g/day, and often involve more than 1 acetaminophen-containing product. Risk is increased with alcohol use, preexisting liver disease, and intake of more than one source of acetaminophen-containing medications. Chronic daily dosing in adults has also resulted in liver damage in some patients.
- Hypotension: May cause severe hypotension (including orthostatic hypotension and syncope); use with caution in patients with hypovolemia, cardiovascular disease (including acute MI), or drugs which may exaggerate hypotensive effects (including phenothiazines or general anesthetics). Monitor for symptoms of hypotension following initiation or dose titration. Avoid use in patients with circulatory shock.
- Respiratory depression: [US Boxed Warning]: Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely for respiratory depression, especially during initiation or dose increase. Carbon dioxide retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids.
- Seizures: Even when taken within the recommended dosage seizures may occur; risk is increased in patients receiving serotonin reuptake inhibitors (SSRIs or anorectics), other opioids, tricyclic antidepressants or other cyclic compounds (including cyclobenzaprine, promethazine), neuroleptics, MAO inhibitors, drugs which may lower seizure threshold, or drugs which impair metabolism of tramadol (ie, CYP2D6 and 3A4 inhibitors). Patients with a history of seizures, or with a risk of seizures (head trauma, metabolic disorders, CNS infection, malignancy, or during alcohol/drug withdrawal) are also at increased risk.
- Serotonin syndrome: May occur with concomitant use of serotonergic agents (eg, SSRIs, SNRIs, triptans, TCAs), lithium, St John's wort, agents that impair metabolism of serotonin (eg, MAO inhibitors), or agents that impair metabolism of tramadol (eg, CYP2D6 and 3A4 inhibitors). Monitor patients for serotonin syndrome such as mental status changes (eg, agitation, hallucinations, coma); autonomic instability (eg, tachycardia, labile blood pressure, hyperthermia); neuromuscular changes (eg, hyperreflexia, incoordination); and/or GI symptoms (eg, nausea, vomiting, diarrhea).
- Skin reactions: Rarely, acetaminophen may cause serious and potentially fatal skin reactions such as acute generalized exanthematous pustulosis, Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN). Discontinue treatment if severe skin reactions develop.
Disease-related concerns:
- Abdominal conditions: May obscure diagnosis or clinical course of patients with acute abdominal conditions.
- Adrenocortical insufficiency: Use with caution in patients with adrenal insufficiency, including Addison disease.
- Biliary tract impairment: Use caution in patients with biliary tract dysfunction or acute pancreatitis; opioids may cause spasm of the sphincter of Oddi.
- CNS depression/coma: Avoid use in patients with impaired consciousness or coma as these patients are susceptible to intracranial effects of CO2 retention.
- Delirium tremens: Use with caution in patients with delirium tremens.
- G6PD deficiency: Use with caution in patients with known G6PD deficiency.
- Head trauma: Use with extreme caution in patients with head injury, intracranial lesions, or elevated intracranial pressure (ICP); exaggerated elevation of ICP may occur.
- Hepatic impairment: Use is not recommended; acetaminophen and tramadol undergo extensive hepatic metabolism.
- Obesity: Use with caution in patients who are morbidly obese.
- Prostatic hyperplasia/urinary stricture: Use with caution in patients with prostatic hyperplasia and/or urinary stricture.
- Psychosis: Use with caution in patients with toxic psychosis.
- Renal impairment: Use with caution in patients with renal impairment.
- Respiratory disease: Use with caution and monitor for respiratory depression in patients with significant chronic obstructive pulmonary disease or cor pulmonale, and those with a substantially decreased respiratory reserve, hypoxia, hypercapnia, or preexisting respiratory depression, particularly when initiating and titrating therapy; critical respiratory depression may occur, even at therapeutic dosages. Consider the use of alternative nonopioid analgesics in these patients.
- Sleep-related disorders: Opioid use increases the risk for sleep-related disorders (eg, central sleep apnea [CSA], hypoxemia) in a dose-dependent fashion. Use with caution for chronic pain and titrate dosage cautiously in patients with risk factors for sleep-disordered breathing (eg, heart failure, obesity). Consider dose reduction in patients presenting with CSA. Avoid opioids in patients with moderate to severe sleep-disordered breathing (CDC [Dowell 2016]).
- Suicide risk: Avoid use in patients who are suicidal; use with caution in patients taking tranquilizers and/or antidepressants, or those with an emotional disturbance including depression. Consider the use of alternative nonopioid analgesics in these patients.
- Thyroid dysfunction: Use with caution in patients with thyroid dysfunction.
Concurrent drug therapy issues:
- Benzodiazepines or other CNS depressants: [US Boxed Warning]: Concomitant use of opioids with benzodiazepines or other CNS depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of tramadol/acetaminophen and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate. Limit dosage and durations to the minimum required and follow patients for signs and symptoms of respiratory depression and sedation.
- CYP P450 interactions: [US Boxed Warning]: The effects of concomitant use or discontinuation of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with tramadol are complex. Use of cytochrome P450 3A4 inducers, 3A4 inhibitors, or 2D6 inhibitors with tramadol/acetaminophen requires careful consideration of the effects on the parent drug, tramadol, and the active metabolite, M1.
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information
Special populations:
- Cachectic or debilitated patients: Use with caution in cachectic or debilitated patients; there is a greater potential for critical respiratory depression, even at therapeutic dosages. Consider the use of alternative nonopioid analgesics in these patients.
- CYP2D6 “ultrarapid metabolizers”: Avoid use in patients who are ultra-rapid metabolizers because of a specific CYP2D6 genotype (gene duplications donated as *1/*1xN or *1/*2xN); these patients may have extensive conversion of tramadol to its active metabolite and thus increased opioid-mediated effects. The occurrence of this phenotype is seen in approximately 1% to 2% of East Asians (Chinese, Japanese, Korean), 1% to 10% of Caucasians, 3 to 4% of African-Americans, and may be >10% in certain racial/ethnic groups (ie, Oceanian, Northern African, Middle Eastern, Ashkenazi Jews, Puerto Rican).
- Elderly: Use with caution in the elderly; may be more sensitive to adverse effects. Clearance may be reduced in older adults (with or without renal impairment) resulting in a narrow therapeutic window and increasing the risk for respiratory depression or overdose (Dowell [CDC 2016]). Consider the use of alternative nonopioid analgesics in these patients.
- Neonates: Neonatal withdrawal syndrome: [US Boxed Warning]: Prolonged use of opioids during pregnancy can cause neonatal withdrawal syndrome, which may be life-threatening if not recognized and treated according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. Signs and symptoms include irritability, hyperactivity and abnormal sleep pattern, high pitched cry, tremor, vomiting, diarrhea and failure to gain weight. Onset, duration and severity depend on the drug used, duration of use, maternal dose, and rate of drug elimination by the newborn.
- Pediatric: [US Boxed Warning]: Life-threatening respiratory depression and death have occurred in children who received tramadol. Some of the reported cases occurred following tonsillectomy and/or adenoidectomy; in at least 1 case, the child had evidence of being an ultra-rapid metabolizer of tramadol due to a CYP-450 2D6 polymorphism. Tramadol/acetaminophen is contraindicated in pediatric patients <12 years and in pediatric patients <18 years following tonsillectomy and/or adenoidectomy. Avoid the use of tramadol/acetaminophen in pediatric patients 12 to 18 years of age who have other risk factors that may increase their sensitivity to the respiratory depressant effects of tramadol. Risk factors include conditions associated with hypoventilation, such as postoperative status, obstructive sleep apnea, obesity, severe pulmonary disease, neuromuscular disease, and concomitant use of other medications that cause respiratory depression. Deaths have also occurred in breastfeeding infants after being exposed to high concentrations of morphine because the mothers were ultra-rapid metabolizers of codeine.
Other warnings/precautions:
- Abrupt discontinuation/withdrawal: Abrupt discontinuation in patients who are physically dependent on opioids has been associated with serious withdrawal symptoms, uncontrolled pain, attempts to find other opioids (including illicit), and suicide. Use a collaborative, patient-specific taper schedule that minimizes the risk of withdrawal, considering factors such as current opioid dose, duration of use, type of pain, and physical and psychological factors. Monitor pain control, withdrawal symptoms, mood changes, suicidal ideation, and for use of other substances; provide care as needed. Concurrent use of mixed agonist/antagonist (eg, pentazocine, nalbuphine, butorphanol) or partial agonist (eg, buprenorphine) analgesics may also precipitate withdrawal symptoms and/or reduced analgesic efficacy in patients following prolonged therapy with mu opioid agonists.
- Abuse/misuse/diversion: [US Boxed Warning]: Use exposes patients and other users to the risks of addiction, abuse, and misuse, potentially leading to overdose and death. Assess each patient's risk prior to prescribing; monitor all patients regularly for development of these behaviors or conditions. Use with caution in patients with a history of drug abuse or acute alcoholism; potential for drug dependency exists. Other factors associated with increased risk for misuse include younger age, concomitant depression (major), and psychotropic medication use.
- Accidental ingestion: [US Boxed Warning]: Accidental ingestion of even one dose, especially in children, can result in a fatal overdose of tramadol.
- Dosage limit: Limit acetaminophen dose from all sources (prescription and OTC) to <4 g/day.
- Optimal regimen: An opioid-containing analgesic regimen should be tailored to each patient's needs and based upon the type of pain being treated, the route of administration, degree of tolerance for opioids (naive versus chronic user), age, weight, and medical condition. The optimal analgesic dose varies widely among patients; doses should be titrated to pain relief/prevention.
- Risk evaluation and mitigation strategy (REMS): [US Boxed Warning]: To ensure that the benefits of opioid analgesics outweigh the risks of addiction, abuse, and misuse, the FDA has required a REMS for these products. Under the requirements of the REMS, drug companies with approved opioid analgesic products must make REMS-compliant education programs available to health care providers. Health care providers are strongly encouraged to complete a REMS-compliant education program; counsel patients and/or their caregivers, with every prescription, on safe use, serious risks, storage, and disposal of these products; emphasize to patients and their caregivers the importance of reading the Medication Guide every time it is provided by their pharmacist; and consider other tools to improve patient, household, and community safety.
- Surgery: Opioids decrease bowel motility; monitor for decrease bowel motility in postop patients receiving opioids. Use with caution in the perioperative setting; individualize treatment when transitioning from parenteral to oral analgesics.
Monitoring Parameters
Pain relief, respiratory and mental status, blood pressure, heart rate; bowel function; signs/symptoms of tolerance, addiction, abuse, misuse, or suicidal ideation.
Pregnancy
Pregnancy Considerations
Acetaminophen and tramadol cross the placenta.
[US Boxed Warning]: Prolonged use of opioids duringpregnancy can cause neonatal withdrawal syndrome, which may be life-threatening if notrecognized and treated according to protocols developed by neonatology experts. If opioid use is required for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available.
Refer to individual monographs for additional information.
Patient Education
What is this drug used for?
- It is used to ease pain.
Frequently reported side effects of this drug
- Dry mouth
- Headache
- Nausea
- Vomiting
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Adrenal gland problems like severe nausea, vomiting, severe dizziness, passing out, muscle weakness, severe fatigue, mood changes, lack of appetite, or weight loss.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Passing out
- Severe dizziness
- Trouble breathing
- Slow breathing
- Shallow breathing
- Noisy breathing
- Severe fatigue
- Severe constipation
- Severe abdominal pain
- Severe loss of strength and energy
- Chest pain
- Fast heartbeat
- Confusion
- Unable to pass urine
- Change in amount of urine passed
- Pale skin
- Vision changes
- Seizures
- Sexual dysfunction (males)
- No menstrual periods
- Decreased sex drive
- Trouble getting pregnant
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.