Boxed Warning
Pregnancy:
Acitretin must not be used by females who are pregnant, or who intend to become pregnant during therapy or at any time for at least 3 years following discontinuation of therapy. Acitretin also must not be used by females who may not use reliable contraception while undergoing treatment and for at least 3 years following discontinuation of treatment. Acitretin is a metabolite of etretinate, and major human fetal abnormalities have been reported with the administration of etretinate and acitretin. Potentially, any fetus exposed can be affected.
Clinical evidence has shown that concurrent ingestion of acitretin and ethanol has been associated with the formation of etretinate, which has a significantly longer elimination half-life than acitretin. Because the longer elimination half-life of etretinate would increase the duration of teratogenic potential for female patients, ethanol must not be ingested by female patients of childbearing potential either during treatment with acitretin or for 2 months after cessation of therapy. This allows for elimination of acitretin, thus removing the substrate for transesterification to etretinate. The mechanism of the metabolic process for conversion of acitretin to etretinate has not been fully defined. It is not known whether substances other than ethanol are associated with transesterification.
Acitretin has been shown to be embryotoxic and/or teratogenic in rabbits, mice, and rats at doses of 0.6, 3, and 15 mg/kg, respectively. These doses are approximately 0.2, 0.3, and 3 times the maximum recommended therapeutic dose, respectively, based on a mg/m2 comparison.
Major human fetal abnormalities associated with acitretin and/or etretinate administration have been reported, including meningomyelocele, meningoencephalocele, multiple synostoses, facial dysmorphia, syndactyly, absence of terminal phalanges, malformations of hip, ankle and forearm, low-set ears, high palate, decreased cranial volume, cardiovascular malformation, and alterations of the skull and cervical vertebrae.
Acitretin should be prescribed only by those who have special competence in the diagnosis and treatment of severe psoriasis, are experienced in the use of systemic retinoids, and understand the risk of teratogenicity.
Because of the teratogenicity of acitretin, a program called the Do Your P.A.R.T program (Pregnancy Prevention Actively Required During and After Treatment), has been developed to educate women of childbearing potential and their health care providers about the serious risks associated with acitretin and to help prevent pregnancies from occurring with the use of this drug and for 3 years after its discontinuation. The Do Your P.A.R.T. program requirements and program materials are available at http://www.soriatane.com/doyour-part-Program.html or may be requested by calling 1-888-784- 3335 (1-888-STIEFEL).
Important information for women of childbearing potential:
Acitretin should be considered only for women with severe psoriasis unresponsive to other therapies or whose clinical condition contraindicates the use of other treatments.
Females of reproductive potential must not be given a prescription for acitretin until pregnancy is excluded. Acitretin is contraindicated in females of reproductive potential unless the patient meets all of the following conditions:
Must have had 2 negative urine or serum pregnancy tests with a sensitivity of at least 25 milliunits/mL before receiving the initial acitretin prescription. The first test (a screening test) is obtained by the prescriber when the decision is made to pursue acitretin therapy. The second pregnancy test (a confirmation test) should be done during the first 5 days of the menstrual period immediately preceding the beginning of acitretin therapy. For patients with amenorrhea, the second test should be done at least 11 days after the last act of unprotected sexual intercourse (without using 2 effective forms of contraception [birth control] simultaneously). If the second pregnancy test is negative, initiation of treatment should begin within 7 days of the specimen collection. Acitretin should be limited to a monthly supply.
Must have a pregnancy test with a sensitivity of at least 25 milliunits/mL repeated every month during treatment with acitretin. The patient must have a negative result from a urine or serum pregnancy test before receiving a prescription for acitretin. To encourage compliance with this recommendation, a monthly supply of the drug should be prescribed. For at least 3 years after discontinuing therapy, a pregnancy test must be repeated every 3 months.
Must have selected and have committed to use 2 effective forms of contraception (birth control) simultaneously, at least 1 of which must be a primary form, unless absolute abstinence is the chosen method, or the patient has undergone a hysterectomy or is clearly postmenopausal.
Patients must use 2 effective forms of contraception (birth control) simultaneously for at least 1 month prior to initiation of acitretin therapy, during acitretin therapy, and for at least 3 years after discontinuing acitretin therapy. A contraception counseling referral form is available so that patients can receive an initial free contraception counseling session and pregnancy testing. Counseling about contraception and behaviors associated with an increased risk of pregnancy must be repeated on a monthly basis by the prescriber during acitretin therapy and every 3 months for at least 3 years following discontinuation of acitretin. Effective forms of contraception include both primary and secondary forms of contraception. Primary forms of contraception include the following: tubal ligation, partner's vasectomy, intrauterine devices, birth control pills, and injectable/implantable/insertable/topical hormonal birth control products. Secondary forms of contraception include latex condoms (with or without spermicide), diaphragms, and cervical caps (which must be used with a spermicide) and vaginal sponges (contains spermicide). Any birth control method can fail. Therefore, it is critically important that women of childbearing potential use 2 effective forms of contraception (birth control) simultaneously. It has not been established if there is a pharmacokinetic interaction between acitretin and combined oral contraceptives. However, it has been established that acitretin interferes with the contraceptive effect of microdosed progestin preparations. Microdosed “minipill” progestin preparations are not recommended for use with acitretin. It is not known whether other progestin-only contraceptives, such as implants and injectables, are adequate methods of contraception during acitretin therapy. Prescribers are advised to consult the package insert of any medication administered concomitantly with hormonal contraceptives because some medications may decrease the effectiveness of these birth control products. Patients should be prospectively cautioned not to self-medicate with the herbal supplement St. John's wort because a possible interaction has been suggested with hormonal contraceptives based on reports of breakthrough bleeding on oral contraceptives shortly after starting St. John's wort. Pregnancies have been reported by users of combined hormonal contraceptives who also used some form of St. John's wort.
Must have signed a Patient Agreement/Informed Consent for Female Patients that contains warnings about the risk of potential birth defects if the fetus is exposed to acitretin, about contraceptive failure, and about the fact that they must not ingest beverages or products containing ethanol while taking acitretin and for 2 months after acitretin treatment has been discontinued, and about preventing pregnancy while taking acitretin and for at least 3 years after discontinuing treatment.
If pregnancy does occur during acitretin therapy or at any time for at least 3 years following discontinuation of acitretin therapy, the prescriber and patient should discuss the possible effects on the pregnancy. The available information is as follows:
Acitretin, the active metabolite of etretinate, is teratogenic and is contraindicated during pregnancy. The risk of severe fetal malformations is well established when systemic retinoids are taken during pregnancy. Pregnancy must also be prevented after stopping acitretin therapy, while the drug is being eliminated to below a threshold blood concentration that would be associated with an increased incidence of birth defects. Because this threshold has not been established for acitretin in humans and because elimination rates vary among patients, the duration of posttherapy contraception to achieve adequate elimination cannot be calculated precisely. It is strongly recommended that contraception be continued for at least 3 years after stopping treatment with acitretin, based on the following considerations:
In the absence of transesterification to form etretinate, greater than 98% of the acitretin would be eliminated within 2 months, assuming a mean elimination half-life of 49 hours.
In cases where etretinate is formed, as has been demonstrated with concomitant administration of acitretin and ethanol, greater than 98% of the etretinate formed would be eliminated in 2 years, assuming a mean elimination half-life of 120 days, and greater than 98% of the etretinate formed would be eliminated in 3 years, based on the longest demonstrated elimination half-life of 168 days. However, etretinate was found in plasma and subcutaneous fat in 1 patient reported to have had sporadic alcohol intake, 52 months after she stopped acitretin therapy.
Severe birth defects have been reported where conception occurred during the time interval when the patient was being treated with acitretin and/or etretinate. In addition, severe birth defects have also been reported when conception occurred after the mother completed therapy. These cases have been reported both prospectively (before the outcome was known) and retrospectively (after the outcome was known). The events below are listed without distinction as to whether the reported birth defects are consistent with retinoid-induced embryopathy or not.
There have been 318 prospectively reported cases involving pregnancies and the use of etretinate, acitretin, or both. In 238 of these cases, the conception occurred after the last dose of etretinate (103 cases), acitretin (126), or both (9). Fetal outcome remained unknown in approximately one-half of these cases, of which 62 were terminated and 14 were spontaneous abortions. Fetal outcome is known for the other 118 cases and 15 of the outcomes were abnormal (including cases of absent hand/wrist, clubfoot, GI malformation, hypocalcemia, hypotonia, limb malformation, neonatal apnea/anemia, neonatal ichthyosis, placental disorder/death, undescended testicle, and 5 cases of premature birth). In the 126 prospectively reported cases where conception occurred after the last dose of acitretin only, 43 cases involved conception at least 1 year but less than 2 years after the last dose. There were 3 reports of abnormal outcomes out of these 43 cases (involving limb malformation, GI tract malformations, and premature birth). There were only 4 cases where conception occurred at least 2 years after the last dose but there were no reports of birth defects in these cases.
There is also a total of 35 retrospectively reported cases where conception occurred at least 1 year after the last dose of etretinate, acitretin, or both. From these cases, there are 3 reports of birth defects when the conception occurred at least 1 year but less than 2 years after the last dose of acitretin (including heart malformations, Turner syndrome, and unspecified congenital malformations) and 4 reports of birth defects when conception occurred 2 or more years after the last dose of acitretin (including foot malformation, cardiac malformations [2 cases], and unspecified neonatal and infancy disorder). There were 3 additional abnormal outcomes in cases where conception occurred 2 or more years after the last dose of etretinate (including chromosome disorder, forearm aplasia, and stillbirth).
Females who have taken etretinate must continue to follow the contraceptive recommendations for etretinate. Etretinate is no longer marketed in the United States; for information, call the manufacturer at 1-888-784-3335 (1-888-STIEFEL).
Patients should not donate blood during and for at least 3 years following the completion of acitretin therapy because women of childbearing potential must not receive blood from patients being treated with acitretin.
Important information for males taking acitretin:
Patients should not donate blood during and for at least 3 years following acitretin therapy because women of childbearing potential must not receive blood from patients being treated with acitretin.
Samples of seminal fluid from 3 male patients treated with acitretin and 6 male patients treated with etretinate have been assayed for the presence of acitretin. The maximum concentration of acitretin observed in the seminal fluid of these men was 12.5 ng/mL. Assuming an ejaculate volume of 10 mL, the amount of drug transferred in semen would be 125 ng, which is 1/200,000 of a single 25 mg capsule. Thus, although it appears that residual acitretin in seminal fluid poses little, if any, risk to a fetus while a male patient is taking the drug or after it is discontinued, the no-effect limit for teratogenicity is unknown and there is no registry for birth defects associated with acitretin. The available data are as follows:
There have been 25 cases of reported conception when the male partner was taking acitretin. The pregnancy outcome is known in 13 of these 25 cases. Of these, 9 reports were retrospective and 4 were prospective (meaning the pregnancy was reported prior to knowledge of the outcome).
When acitretin treatment was given at time of conception, there were 5 deliveries of healthy neonates (4 of 5 cases were prospective), 5 spontaneous abortions, and 1 induced abortion.
When acitretin was discontinued approximately 4 weeks prior to conception, there was 1 induced abortion (with malformation pattern not typical of retinoid embryopathy [bilateral cystic hygromas of neck, hypoplasia of lungs bilateral, pulmonary atresia, ventricular septal defect with overriding truncus arteriosus]).
When acitretin was discontinued approximately 6 to 8 months prior to conception, there was 1 spontaneous abortion.
Medication guide (for all patients):
An acitretin Medication Guide must be given to the patient each time acitretin is dispensed, as required by law.
Hepatotoxicity:
Of the 525 patients treated in US clinical trials, 2 had clinical jaundice with elevated serum bilirubin and transaminases considered related to acitretin treatment. Liver function test results in these patients returned to normal after acitretin was discontinued. Two of the 1,289 patients treated in European clinical trials developed biopsy-confirmed toxic hepatitis. A second biopsy in 1 of these patients revealed nodule formation suggestive of cirrhosis. One patient in a Canadian clinical trial of 63 patients developed a 3-fold increase of transaminases. A liver biopsy of this patient showed mild lobular disarray, multifocal hepatocyte loss, and mild triaditis of the portal tracts compatible with acute reversible hepatic injury. The patient's transaminase levels returned to normal 2 months after acitretin was discontinued.
The potential of acitretin therapy to induce hepatotoxicity was prospectively evaluated using liver biopsies in an open-label study of 128 patients. Pretreatment and posttreatment biopsies were available for 87 patients. A comparison of liver biopsy findings before and after therapy revealed 58% of patients showed no change, 25% improved, and 17% of patients had a worsening of their liver biopsy status. For 6 patients, the classification changed from class 0 (no pathology) to class I (normal fatty infiltration; nuclear variability and portal inflammation; both mild); for 7 patients, the change was from class I to class II (fatty infiltration, nuclear variability, portal inflammation and focal necrosis; all moderate to severe); and for 1 patient, the change was from class II to class IIIb (fibrosis, moderate to severe). No correlation could be found between liver function test result abnormalities and the change in liver biopsy status, and no cumulative dose relationship was found.
Elevations of AST, ALT, gamma-glutamyl transpeptidase (GGT; GGTP), or lactate dehydrogenase (LDH) have occurred in approximately 1 in 3 patients treated with acitretin. Of the 525 patients treated in clinical trials in the United States, treatment was discontinued in 3.8% of patients due to elevated liver function test results. If hepatotoxicity is suspected during treatment with acitretin, the drug should be discontinued and the etiology further investigated.
Ten of 652 patients treated in US clinical trials of etretinate, of which acitretin is the active metabolite, had clinical or histologic hepatitis considered to be possibly or probably related to etretinate treatment. There have been reports of hepatitis-related deaths worldwide; a few of these patients had received etretinate for 1 month or less before presenting with hepatic symptoms or signs.
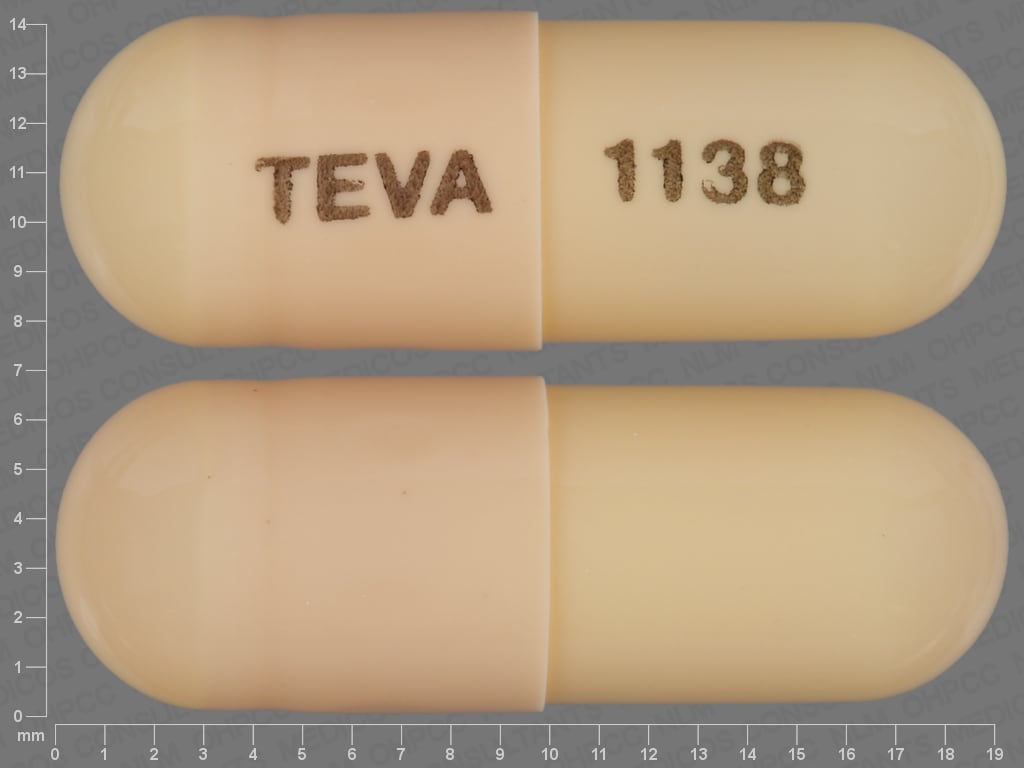
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Soriatane: 10 mg, 17.5 mg [DSC], 25 mg [contains edetate calcium disodium]
Generic: 10 mg, 17.5 mg, 25 mg
Pharmacology
Mechanism of Action
Binds to and activates all nuclear subtypes (alpha, beta, and gamma) of retinoid X receptors (RXR) and retinoic acid receptors (RAR) to inhibit the expression of the proinflammatory cytokines interleukin-6 (IL-6), migration inhibitory factor-related protein-8 (MRP-8), and interferon-gamma (markers of hyperproliferation and abnormal keratinocyte differentiation). Resulting actions are anti-inflammatory and antiproliferative, and keratinocyte differentiation is normalized in the epithelium.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: ~72% absorbed when given with food
Metabolism
Metabolized to cis-acitretin; both compounds are further metabolized. Concomitant ethanol use leads to the formation of etretinate (active).
Excretion
Feces (34% to 54%); urine (16% to 53%)
Onset of Action
May take 2 to 3 months for full effect; improvement may be seen within 8 weeks
Time to Peak
2-5 hours
Half-Life Elimination
Acitretin: 49 hours (range: 33 to 96); cis-acitretin: 63 hours (range: 28 to 157); etretinate: 120 days (range: Up to 168 days)
Protein Binding
>99% bound, primarily to albumin
Use in Specific Populations
Special Populations: Renal Function Impairment
Plasma concentrations are lower in end-stage renal failure.
Special Populations: Elderly
Higher plasma concentrations are seen; however, no changes occur in the half-life.
Use: Labeled Indications
Psoriasis: Treatment of severe psoriasis in adults.
Limitations of use: Not for the treatment of acne.
Use: Off Label
Disorders of keratinizationc
Data from a limited number of patients studied suggest that acitretin may be beneficial for the treatment of various nonpsoriatic disorders of keratinization (eg, lamellar ichthyosis, palmoplantar keratoderma, nonbullous congenital ichthyosiform erythroderma, Darier disease, pityriasis rubra pilaris, arsenical keratosis) Blanchet-Bardon 1991, Kullavanijaya 1993. Additional data may be necessary to further define the role of acitretin in these conditions.
Contraindications
Hypersensitivity (eg, angioedema, urticaria) to acitretin, other retinoids, or any component of the formulation; patients who are pregnant or intend on becoming pregnant during therapy or within 3 years after treatment discontinuation; severe hepatic or renal dysfunction; chronic abnormally elevated blood lipid levels; concomitant use with methotrexate or tetracyclines
Acitretin is contraindicated in females of childbearing potential unless all of the following conditions apply.
1) Patient has severe psoriasis unresponsive to other therapy or if clinical condition contraindicates other treatments.
2) Patient must have two negative urine or serum pregnancy tests prior to therapy.
3) Patient must have pregnancy test repeated monthly during therapy. After discontinuation of therapy, a pregnancy test must be repeated every 3 months for at least 3 years.
4) Patient must commit to using two effective forms of birth control starting 1 month prior to acitretin treatment and for 3 years after discontinuation. Prescriber must counsel patient about contraception every month during therapy and every 3 months following discontinuation for at least 3 years.
5) Patient is reliable in understanding and carrying out instructions.
6) Patient has received, and acknowledged, understanding of a careful oral and printed explanation of the hazards of fetal exposure to acitretin and the risk of possible contraception failure. Patient must sign an agreement/informed consent document stating that she understands these risks and that she should not consume ethanol during therapy or for 2 months after discontinuation.
Canadian labeling: Additional contraindications (not in U.S. labeling): Breastfeeding; concomitant use with Vitamin A or other retinoids
Dosage and Administration
Dosing: Adult
Psoriasis: Oral: Individualization of dosage is required to achieve maximum therapeutic response while minimizing side effects
Initial: 25 to 50 mg daily, given as a single dose with the main meal
Maintenance: 25 to 50 mg daily may be given after initial response to treatment; the maintenance dose should be based on clinical efficacy and tolerability
American Academy of Dermatology recommendations: 10 to 50 mg daily as a single dose; doses ≤25 mg daily are used to decrease side effects (Menter 2009)
Disorders of keratinization (nonpsoriatic) (off-label use): Oral: Initial: 25 to 35 mg once daily for 4 weeks than adjust dose as needed; maintenance: 10 to 50 mg daily; maximum: 50 mg daily (Blanchet-Bardon 1991; Kullavanijava 1993; Soriatane Canadian product labeling)
Dosing: Geriatric
Refer to adult dosing.
Administration
Administer with food, preferably with the main meal of the day.
Dietary Considerations
Avoid ingestion of additional sources of exogenous vitamin A (in excess of RDA); females of childbearing potential should not ingest ethanol and ethanol-containing products during therapy and for 2 months after the last dose of acitretin.
Storage
Store between 15°C to 25°C (59°F to 77°F). Avoid high temperatures and humidity. Protect from light.
Acitretin Images
Drug Interactions
Alcohol (Ethyl): May enhance the teratogenic effect of Acitretin. Avoid combination
Aminolevulinic Acid (Systemic): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Systemic). Avoid combination
Aminolevulinic Acid (Topical): Photosensitizing Agents may enhance the photosensitizing effect of Aminolevulinic Acid (Topical). Monitor therapy
Methotrexate: Acitretin may enhance the hepatotoxic effect of Methotrexate. Avoid combination
Multivitamins/Fluoride (with ADE): May enhance the adverse/toxic effect of Retinoic Acid Derivatives. Avoid combination
Multivitamins/Minerals (with ADEK, Folate, Iron): May enhance the adverse/toxic effect of Retinoic Acid Derivatives. Avoid combination
Multivitamins/Minerals (with AE, No Iron): May enhance the adverse/toxic effect of Retinoic Acid Derivatives. Avoid combination
Porfimer: Photosensitizing Agents may enhance the photosensitizing effect of Porfimer. Monitor therapy
Progestins (Contraceptive): Acitretin may diminish the therapeutic effect of Progestins (Contraceptive). Contraceptive failure is possible. Management: Given the potential for progestin-only preparations to fail to prevent pregnancy during acitretin therapy, such products should not be relied upon. Alternative, nonhormonal forms of contraception must be employed during acitretin therapy. Consider therapy modification
Tetracyclines: May enhance the adverse/toxic effect of Retinoic Acid Derivatives. The development of pseudotumor cerebri is of particular concern. Avoid combination
Verteporfin: Photosensitizing Agents may enhance the photosensitizing effect of Verteporfin. Monitor therapy
Vitamin A: May enhance the adverse/toxic effect of Retinoic Acid Derivatives. Avoid combination
Adverse Reactions
>10%:
Central nervous system: Hyperesthesia (10% to 25%), paresthesia (10% to 25%), rigors (10% to 25%)
Dermatologic: Cheilitis (>75%), alopecia (50% to 75%), exfoliation of skin (50% to 75%), xeroderma (25% to 50%), nail disease (25% to 50%), pruritus (25% to 50%), erythematous rash (10% to 25%), paronychia (10% to 25%), skin atrophy (10% to 25%), acquired cutaneous adherence (10% to 25%)
Endocrine & metabolic: Hypertriglyceridemia (50% to 75%), increased serum glucose (fasting; 25% to 50%), decreased HDL cholesterol (25% to 50%), hypercholesterolemia (25% to 50%), acetonuria (10% to 25%), decreased serum glucose (fasting; 10% to 25%), decreased serum magnesium (10% to 25%), hypermagnesemia (10% to 25%), hyperphospheremia (10% to 25%), increased gamma-glutamyl transferase (10% to 25%), increased serum potassium (10% to 25%), increased serum sodium (10% to 25%), increased uric acid (10% to 25%)
Gastrointestinal: Xerostomia (10% to 25%)
Genitourinary: Erythrocyturia (10% to 25%), hematuria (10% to 25%)
Hematologic & oncologic: Leukocyturia (25% to 50%), reticulocytosis (25% to 50%), increased haptoglobin (10% to 25%), decreased hematocrit (10% to 25%), decreased hemoglobin (10% to 25%), increased neutrophils (10% to 25%), change in WBC count (10% to 25%)
Hepatic: Increased liver enzymes (25% to 50%), increased serum alkaline phosphatase (10% to 25%), increased direct serum bilirubin (10% to 25%)
Neuromuscular & skeletal: Increased creatine phosphokinase (25% to 50%), arthralgia (10% to 25%), spinal hyperostosis (progression; 10% to 25%)
Ophthalmic: Xerophthalmia (10% to 25%)
Respiratory: Rhinitis (25% to 50%), epistaxis (10% to 25%)
1% to 10%:
Cardiovascular: Edema, flushing
Central nervous system: Bell's palsy, depression, drowsiness, fatigue, headache, hypertonia, insomnia, pain
Dermatologic: Abnormal hair texture, abnormal skin odor, Bullous skin disease, cold and clammy skin, dermatitis, diaphoresis (increased), madarosis, psoriasiform eruption, pyogenic granuloma, seborrhea, skin fissure, skin rash, sunburn
Endocrine & metabolic: Decreased haptoglobins, decreased serum albumin, decreased serum calcium, decreased serum iron, decreased serum potassium, decreased serum sodium, diaphoresis (increased), glycosuria, hot flash, hyperchloremia, hypochloremia, hypophosphatemia, increased serum albumin, increased serum calcium, increased serum iron, increased thirst
Gastrointestinal: Abdominal pain, anorexia, aphthous stomatitis, diarrhea, dysgeusia, gingival hemorrhage, gingivitis, increased appetite, nausea, sialorrhea, stomatitis, tongue disease
Genitourinary: Proteinuria
Hematologic & oncologic: Change in RBC count, decreased neutrophils, increased hematocrit, increased hemoglobin, reticulocytopenia, purpura
Hepatic: Increased serum bilirubin
Neuromuscular & skeletal: Arthritis, back pain, myalgia, ostealgia, osteoarthritis, peripheral joint hyperostosis
Ophthalmic: Blepharitis, blurred vision, cataract, conjunctivitis, diplopia, epithelial keratopathy, eye pain, nocturnal amblyopia, photophobia
Otic: Otalgia, tinnitus
Renal: Increased blood urea nitrogen, increased serum creatinine
Respiratory: Sinusitis
Miscellaneous: Ulcer
<1%: Abnormal gait, abnormal lacrimation, acne vulgaris, ageusia, aggressive behavior, alcohol intolerance, anal disease, angioedema, anxiety, bone disease, bursitis (olecranon), candidiasis, capillary leak syndrome, cerebrovascular accident, chalazion, chest pain, conjunctival hemorrhage, constipation, corneal lesion, corneal ulcer, cough, cutaneous nodule, cyanosis, cyst, deafness, decreased libido, diplopia, dizziness, dyspepsia, dysuria, ectropion, eczema, epidermal thinning, erythroderma, esophagitis, exfoliation of skin, exfoliative dermatitis, eye pruritus, fever, flu-like symptoms, fragile skin, fungal infection, furunculosis, gastritis, gastroenteritis, gingival hyperplasia, glossitis, hair discoloration, hemorrhage, hemorrhoids, hepatic cirrhosis, hepatic dysfunction, hepatitis, herpes simplex infection, hordeolum (recurrent), hyperkeratosis, hypersensitivity reaction, hypertrichosis, hypoesthesia, increased bronchial secretions, increased cerumen production, intermittent claudication, jaundice, laryngitis, leukorrhea, malaise, mastalgia, melena, migraine, myasthenia, myocardial infarction, myopathy (with peripheral neuropathy), nail disease (fragility), nervousness, neuritis, otitis media, pancreatitis, papilledema, peripheral ischemia, pharyngitis, prolonged bleeding time, pseudotumor cerebri, scleroderma, skin hypertrophy, skin photosensitivity, spinal hyperostosis (new lesion), suicidal ideation, tendonitis, tenesmus, thromboembolism, tongue ulcer, urticaria, vaginitis, voice disorder, vulvovaginitis, warts, weight gain, wound healing impairment
Warnings/Precautions
Concerns related to adverse effects:
- Capillary leak syndrome: Capillary leak syndrome, a potential manifestation of retinoic acid syndrome (differentiation syndrome) has been reported with acitretin use. Capillary leak syndrome features may include localized or generalized edema with secondary weight gain, fever, and hypotension; rhabdomyolysis and myalgias have also been reported. Laboratory tests may show neutrophilia, hypoalbuminemia, and an elevated hematocrit. Discontinue use if capillary leak syndrome develops during therapy.
- Depression: Depression, including aggressive behavior and thoughts of self-harm have been reported; use with caution in patients with a history of mental illness.
- Exfoliative dermatitis: Exfoliative dermatitis has been reported with acitretin use; discontinue use if exfoliative dermatitis occurs during therapy.
- Hepatotoxicity: [US Boxed Warnings]: Hepatitis has been reported (including fatalities); some patients received etretinate for ≤1 month before presenting with hepatic signs or symptoms. Changes in transaminases have occurred in up to 1/3of patients, which generally returned to normal after discontinuation of treatment. Monitor for hepatotoxicity; discontinue if hepatotoxicity is suspected.
- Lipid effects: Lipid changes, including increased triglycerides, increased cholesterol, and decreased HDL, are common (up to 66%), which were reversible upon discontinuation of treatment; increased triglycerides may lead to pancreatitis. Fatal fulminant pancreatitis has been reported. Use with caution in patients at risk of hypertriglyceridemia (eg, patients with lipid metabolism disturbances, diabetes mellitus, obesity, increased alcohol intake, or a familial history of these conditions). Consider discontinuation if hypertriglyceridemia and decreased HDL persist. Use is contraindicated in patients with chronic abnormally elevated blood lipid values.
- Otic effects: Tinnitus and impaired hearing have been reported with use; consider therapy discontinuation and further evaluation if clinically indicated.
- Photosensitivity: May be photosensitizing; minimize sun or other UV exposure to treated areas. The risk of burning is increased with phototherapy; decreased doses are required.
- Pseudotumor cerebri: Retinoids, including acitretin, have been associated with pseudotumor cerebri (benign intracranial hypertension). Concurrent use of other drugs associated with this effect (eg, tetracyclines) may increase risk. Early signs and symptoms include papilledema, headache, nausea, vomiting, and visual disturbances. Discontinue use in patients experiencing papilledema.
- Skeletal abnormalities: Patients receiving long-term treatment should be periodically examined for bony abnormalities; risk vs benefit of therapy should be considered if abnormalities occur.
- Visual disturbances: May cause adverse effects to the eyes and vision, including a decrease in night vision or decreased tolerance to contact lenses. Use caution when operating vehicles at night; discontinue if visual changes occur.
Disease-related concerns:
- Diabetes: Impaired glucose control has been reported with retinoid use. Use with caution in patients with diabetes mellitus; new cases of diabetes have been diagnosed.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Ethanol use: [US Boxed Warning]: Female patients of childbearing potential should abstain from ethanol or ethanol-containing products during therapy and for 2 months after discontinuation.
Special populations:
- Females: [US Boxed Warning]: Females of childbearing potential must be able to fulfill all conditions for use prior to initiating therapy, including a Patient Agreement/Informed Consent (consult manufacturer's labeling for further detail). Prescriptions should be written for a monthly supply. The Do Your P.A.R.T. (Pregnancy Prevention Actively Required During and After Treatment) program explains teratogenic risks and requirements expected of females of childbearing potential to prevent pregnancies from occurring during use and 3 years following discontinuation; this should be used to educate patients and healthcare providers. Information for the Do Your P.A.R.T. program is available at www.soriatane.com/doyour-part-Program.html or by calling 1-888-784-3335.
- Pediatric: Growth potential may be affected. Long-term use of high-dose oral retinoids within this population has been associated with decreased bone mineral density, skeletal hyperostosis, and ossification of interosseous tendons and ligaments of the extremities (Menter, 2009).
- Pregnancy: [US Boxed Warning]: Acitretin is a known teratogen and contraindicated in females who are or may become pregnant. Birth defects (including facial, ear, central nervous system, cardiovascular, limb, bone, and joint) have been noted following acitretin exposure during pregnancy. Use only in women with severe psoriasis that is unresponsive to other therapies or with contraindications to the use of alternative treatments. Pregnancy must be avoided for at least 3 years after treatment discontinuation. Two reliable forms of contraception must be used simultaneously for 1 month prior to initiating therapy, during therapy, and for 3 years after discontinuation. Two negative pregnancy tests (sensitivity at least 25 milliunits/mL) are required prior to initiating therapy; pregnancy tests must be repeated every month during treatment. In addition, because ethanol forms a teratogenic metabolite and would increase the duration of teratogenic potential, ethanol should not be consumed during treatment or for 2 months after discontinuation. Any pregnancy which occurs during treatment, or within 3 years after treatment is discontinued, should be reported to the manufacturer at 1-888-784-3335 or to the FDA at 1-800-FDA-1088.
Other warnings/precautions:
- Blood donation: [US Boxed Warning]: All patients should be advised not to donate blood during therapy or for 3 years following completion of therapy.
- Experienced physician: [US Boxed Warning]: Only physicians experienced with the diagnosis and treatment of severe psoriasis, including the use of retinoid treatment, and physicians who understand the risk of teratogenicity should prescribe acitretin.
- Medication guide: [US Boxed Warning]: All patients must be provided with a medication guide each time acitretin is dispensed. Female patients must also sign an informed consent prior to therapy.
- Subsequent use: Most patients experience relapse of psoriasis after discontinuing therapy. Subsequent courses, when clinically indicated, have produced results similar to the initial course of therapy.
- Worsening of disease: Transient worsening of psoriasis may initially occur; patients should be advised that it may take 2-3 months to achieve the full benefits of treatment.
Monitoring Parameters
Lipid profile (baseline and at 1- to 2-week intervals for 4 to 8 weeks, then as clinically indicated); liver function tests (baseline, and at 1- to 2-week intervals until stable, then as clinically indicated); blood glucose in patients with diabetes; evaluate for bone abnormalities (with long-term use)
Pregnancy testing in females of reproductive potential:
- Two negative urine or serum pregnancy tests with a sensitivity of ≥25 mIU per mL before receiving the initial prescription. The first test should be done at the time the decision is made to prescribe acitretin; the second test should be conducted within the first 5 days of the menstrual period immediately prior to the initiation of treatment.
- A pregnancy test with a sensitivity of ≥25 mIU per mL must be repeated monthly during treatment and every 3 months for ≥3 years after discontinuation of acitretin.
The American Academy of Dermatology recommends: CBC and renal function tests (baseline and then every 12 weeks); liver function tests (every 2 weeks for the first 8 weeks, then every 6 to 12 weeks thereafter) (Menter, 2009)
Pregnancy
Pregnancy Considerations
[US Boxed Warning]: Acitretin must not be used by females who are pregnant, or who intend to become pregnant during therapy or at any time for at least 3 years following discontinuation of therapy.
Acitretin is a metabolite of etretinate; major birth defects have been reported with both etretinate and acitretin. Birth defects in humans include meningomyelocele; meningoencephalocele; multiple synostoses; facial dysmorphia; syndactyly; absence of terminal phalanges; malformations of hip, ankle, and forearm; low-set ears; high palate; decreased cranial volume; cardiovascular malformation; and alterations of the skull and cervical vertebrae. All exposed fetuses have the potential to be affected.
Pregnancy outcome information is available from prospectively (n=318) and retrospectively (n=35) collected data following exposure to etretinate and/or acitretin. Of the 318 prospectively reported pregnancies, conception occurred in 238 cases after the last maternal dose and fetal outcome is known in 118 cases: 15 were abnormal (absent hand/wrist, clubfoot, GI malformation, hypocalcemia, hypotonia, limb malformation, neonatal apnea/anemia, neonatal ichthyosis, placental disorder/death, undescended testicle, and five cases of premature birth), 62 pregnancies were terminated, and 14 ended in spontaneous abortion. Conception occurred ≥1 year after the last dose of etretinate and/or acitretin in the retrospective reports. When conception occurred ≥1 year but <2 years after the last dose of acitretin, birth defects occurred in three cases (including heart malformations, Turner syndrome, and unspecified congenital malformations). When conception occurred ≥2 years after the last dose of acitretin, birth defects occurred in four cases (including foot malformation, cardiac malformations [two cases], and unspecified neonatal and infancy disorder). When conception occurred ≥2 years after the last dose of etretinate, abnormal outcomes were noted in three cases (including chromosome disorder, forearm aplasia, and stillbirth).
If pregnancy occurs during acitretin therapy or at any time for at least 3 years following discontinuation of acitretin, the prescriber and patient should discuss the possible effects on the pregnancy.
[US Boxed Warning]: Pregnancy must be excluded prior to therapy. Acitretin should be considered only for females of childbearing potential with severe psoriasis unresponsive to other therapies or whose clinical condition contraindicates the use of other treatments. Use is contraindicated in females of reproductive potential unless all conditions associated with use can be met, including two negative urine or serum pregnancy tests with a sensitivity of ≥25 mIU per mL before receiving the initial acitretin prescription; a pregnancy test every month during treatment; use of two effective forms of contraception simultaneously (at least one of which must be a primary form, unless absolute abstinence is the chosen method, or the patient has undergone a hysterectomy or is clearly postmenopausal). Female patients must sign the Patient Agreement/Informed Consent for Female Patients prior to beginning therapy. To encourage compliance with these recommendations, only a 1-month supply of the acitretin should be prescribed. Pregnancy testing must be repeated every 3 months for at least 3 years after acitretin is discontinued.
Effective contraception include both a primary (tubal ligation, partner’s vasectomy, intrauterine devices, birth control pills, and injectable/implantable/insertable/topical hormonal birth control products) and secondary (condoms with or without spermicide, diaphragms and cervical caps which must be used with a spermicide, and vaginal sponges containing a spermicide) form. Microdosed “minipill” progestin preparations are not recommended. Concomitant therapy should be evaluated for potential drug interactions that may decrease the effectiveness of the birth control methods used. A 24-hour number (1-800-739-6700) is available for patients to receive automated birth control and emergency contraception information.
Prescribing of acitretin should be done only by providers experienced with the diagnosis and treatment of severe psoriasis, including the use of retinoid treatment, and those who understand the risk of teratogenicity.
Limited amounts of acitretin are found in seminal fluid; although it appears this poses little risk to a fetus, the actual risk of teratogenicity is not known.
The Do Your P.A.R.T. (Pregnancy Prevention Actively Required During and After Treatment) program explains teratogenic risks and requirements expected of females of childbearing potential to prevent pregnancies from occurring during use and 3 years following discontinuation; this should be used to educate patients and health care providers. Information for the Do Your P.A.R.T. program is available at www.soriatane.com/doyour-part-Program.html or by calling 1-888-784-3335.
Any pregnancy which occurs during treatment, or at any time for at least 3 years after treatment is discontinued, should be reported to the manufacturer at 1-888-784-3335 or to the FDA at 1-800-FDA-1088.
Patient Education
What is this drug used for?
- It is used to treat psoriasis.
Frequently reported side effects of this drug
- Runny nose
- Nail changes
- Dry mouth
- Dry lips
- Dry eyes
- Itching
- Hair loss
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Capillary leak syndrome like abnormal heartbeat; chest pain; shortness of breath; weight gain; vomiting blood or vomit that looks like coffee grounds; black, tarry, or bloody stools; unable to pass urine or change in amount of urine passed; or blood in the urine
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion
- High blood sugar like confusion, fatigue, increased thirst, hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit
- Severe cerebrovascular disease like change in strength on one side is greater than the other, trouble speaking or thinking, change in balance, or change in eyesight
- Pancreatitis like severe abdominal pain, severe back pain, severe nausea, or vomiting
- Aggressive behavior
- Chest pain
- Severe dizziness
- Passing out
- Shortness of breath
- Severe headache
- Nausea
- Vomiting
- Seizures
- Burning or numbness feeling
- Swelling of the extremities
- Painful extremities
- Warm sensation in extremities
- Extremity skin discoloration
- Severe muscle pain
- Severe muscle weakness
- Bone pain
- Joint pain
- Vision changes
- Eye pain
- Severe eye irritation
- Contact lens discomfort
- Trouble hearing
- Noise or ringing in the ears
- Swelling
- Weight gain
- Abdominal pain
- Severe diarrhea
- Rectal bleeding
- Rectal pain
- Poor night vision
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.