Boxed Warning
Suicidal ideation in children and adolescents:
Atomoxetine increased the risk of suicidal ideation in short-term studies in children or adolescents with attention deficit hyperactivity disorder (ADHD). Anyone considering the use of atomoxetine in a child or adolescent must balance this risk with the clinical need. Comorbidities occurring with ADHD may be associated with an increase in the risk of suicidal ideation and/or behavior. Closely monitor patients who are started on therapy for suicidality (suicidal thinking and behavior), clinical worsening, or unusual changes in behavior. Advise families and caregivers of the need for close observation and communication with the prescribing health care provider. Atomoxetine is approved for ADHD in pediatric and adult patients. Atomoxetine is not approved for major depressive disorder (MDD).
Pooled analyses of short-term (6- to 18-week), placebo-controlled trials of atomoxetine in children and adolescents (12 trials involving more than 2,200 patients, including 11 trials in ADHD and 1 trial in enuresis) have revealed a greater risk of suicidal ideation early during treatment in those receiving atomoxetine compared with placebo. The average risk of suicidal ideation in patients receiving atomoxetine was 0.4% compared with none in placebo-treated patients. No suicides occurred in these trials.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, Oral:
Strattera: 10 mg, 18 mg
Strattera: 25 mg [contains fd&c blue #2 (indigotine)]
Strattera: 40 mg, 60 mg, 80 mg [contains corn starch, fd&c blue #2 (indigotine)]
Strattera: 100 mg [contains fd&c blue #2 (indigotine)]
Generic: 10 mg, 18 mg, 25 mg, 40 mg, 60 mg, 80 mg, 100 mg
Pharmacology
Mechanism of Action
Selectively inhibits the reuptake of norepinephrine (Ki 4.5 nM) with little to no activity at the other neuronal reuptake pumps or receptor sites.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Vd: IV: 0.85 L/kg
Metabolism
Hepatic, via CYP2D6 and CYP2C19; forms metabolites (4-hydroxyatomoxetine, active, equipotent to atomoxetine; N-desmethylatomoxetine, limited activity); Note: CYP2D6 poor metabolizers have atomoxetine AUCs that are ~10-fold higher and peak concentrations that are ~fivefold greater than extensive metabolizers; 4-hyroxyatomoxetine plasma concentrations are very low (extensive metabolizers: 1% of atomoxetine concentrations; poor metabolizers: 0.1% of atomoxetine concentrations
Excretion
Urine (80%, as conjugated 4-hydroxy metabolite; <3% is excreted unchanged); feces (17%)
Time to Peak
Plasma: 1-2 hours; delayed 3 hours by high-fat meal
Duration of Action
Up to 24 hours (Jain 2017)
Half-Life Elimination
Atomoxetine: 5 hours (up to 24 hours in poor metabolizers); Active metabolites: 4-hydroxyatomoxetine: 6-8 hours; N-desmethylatomoxetine: 6-8 hours (34-40 hours in poor metabolizers)
Protein Binding
98%, primarily albumin
Use in Specific Populations
Special Populations: Renal Function Impairment
Extensive metabolizers with ESRD had higher systemic exposure (approximately a 65% increase), but there was no difference when exposure was corrected for mg/kg dose.
Special Populations: Hepatic Function Impairment
AUC is increased in extensive metabolizers with moderate or severe hepatic impairment.
Use: Labeled Indications
Attention-deficit/hyperactivity disorder: Treatment of attention-deficit/hyperactivity disorder (ADHD)
Contraindications
Hypersensitivity to atomoxetine or any component of the formulation; use with or within 14 days of MAO inhibitors; narrow-angle glaucoma; current or history of pheochromocytoma; severe cardiac or vascular disorders in which the condition would be expected to deteriorate with clinically important increases in blood pressure (eg, 15 to 20 mm Hg) or heart rate (eg, 20 beats/minute).
Canadian labeling: Additional contraindications (not in US labeling): Symptomatic cardiovascular diseases, moderate to severe hypertension; advanced arteriosclerosis; uncontrolled hyperthyroidism
Dosage and Administration
Dosing: Adult
Attention-deficit/hyperactivity disorder (ADHD) treatment: Oral: Note: Atomoxetine may be discontinued without tapering.
Initial: 40 mg/day, increase after minimum of 3 days to 80 mg/day; may administer as a single daily dose in the morning or as 2 evenly divided doses in the morning and late afternoon/early evening. May increase (if optimal response has not been achieved) to 100 mg/day after an additional 2 to 4 weeks. Maximum: 100 mg/day.
Dosage adjustment in patients receiving strong CYP2D6 inhibitors (eg, paroxetine, fluoxetine, quinidine) or patients known to be CYP2D6 poor metabolizers: Initial: 40 mg/day; if tolerating therapy but inadequate response, may increase after minimum of 4 weeks to 80 mg/day.
Dosing: Geriatric
Use has not been evaluated in the elderly.
Dosing: Pediatric
Attention-deficit/hyperactivity disorder: Children ≥6 years and Adolescents:
Patient weight ≤70 kg: Oral: Initial: ~0.5 mg/kg/day; increase after a minimum of 3 days to ~1.2 mg/kg/day; may administer either once daily in the morning or in 2 evenly divided doses and administered in the morning and late afternoon/early evening; maximum daily dose: 1.4 mg/kg/day or 100 mg/day, whichever is less. Note: Doses >1.2 mg/kg/day have not been shown to provide additional benefit.
Dosage adjustment with concurrent strong CYP2D6 inhibitors (eg, paroxetine, fluoxetine, quinidine) use or patients known to be CYP2D6 poor metabolizers: Oral: Initial: 0.5 mg/kg/day; if tolerating therapy but inadequate response, may increase after a minimum of 4 weeks to 1.2 mg/kg/day.
Patient weight >70 kg: Oral: Initial: 40 mg once daily; increase after a minimum of 3 days to ~80 mg daily; may administer either once daily in the morning or in 2 evenly divided doses and administered in morning and late afternoon/early evening. If optimal response has not been achieved after an additional 2 to 4 weeks of therapy, may increase dose up to a maximum daily dose: 100 mg/day.
Dosage adjustment with concurrent strong CYP2D6 inhibitors (eg, paroxetine, fluoxetine, quinidine) use or patients known to be CYP2D6 poor metabolizers: Oral: Initial: 40 mg once daily; if tolerating therapy but inadequate response, may increase after a minimum of 4 weeks to 80 mg/day.
Administration
Oral: Administer without regard to food. Do not crush, chew, or open capsule; swallow whole. Note: Atomoxetine is an ocular irritant; if capsule is opened inadvertently and contents come into contact with eye, flush eye immediately with water and obtain medical advice; wash hands and any potentially contaminated surface as soon as possible.
Storage
Store at 25°C (77°F); excursions are permitted between 15°C and 30°C (59°F and 86°F).
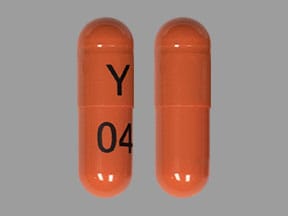
AtoMOXetine Images
Drug Interactions
Abiraterone Acetate: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of abiraterone with CYP2D6 substrates that have a narrow therapeutic index whenever possible. When concurrent use is not avoidable, monitor patients closely for signs/symptoms of toxicity. Consider therapy modification
Ajmaline: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Asunaprevir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Consider therapy modification
Beta2-Agonists: AtoMOXetine may enhance the tachycardic effect of Beta2-Agonists. Monitor therapy
CloBAZam: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Cobicistat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Moderate): May decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
CYP2D6 Inhibitors (Strong): May increase the serum concentration of AtoMOXetine. Management: Initiate atomoxetine at a reduced dose (adult doses -- patients up to 70kg: 0.5mg/kg/day; patients 70kg or more: 40mg/day) in patients receiving a strong CYP2D6 inhibitor. Consider therapy modification
Dacomitinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Management: Avoid concurrent use of dacomitinib with CYP2D6 subtrates that have a narrow therapeutic index. Consider therapy modification
Darunavir: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Haloperidol: QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of Haloperidol. Monitor therapy
Imatinib: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Iobenguane Radiopharmaceutical Products: Selective Norepinephrine Reuptake Inhibitors may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Lumefantrine: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Monoamine Oxidase Inhibitors: May enhance the neurotoxic (central) effect of AtoMOXetine. Avoid combination
Panobinostat: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Peginterferon Alfa-2b: May decrease the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Peginterferon Alfa-2b may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Perhexiline: CYP2D6 Substrates (High risk with Inhibitors) may increase the serum concentration of Perhexiline. Perhexiline may increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
QT-prolonging Agents (Highest Risk): QT-prolonging Agents (Indeterminate Risk - Caution) may enhance the QTc-prolonging effect of QT-prolonging Agents (Highest Risk). Management: Monitor for QTc interval prolongation and ventricular arrhythmias when these agents are combined. Patients with additional risk factors for QTc prolongation may be at even higher risk. Monitor therapy
QuiNINE: May increase the serum concentration of CYP2D6 Substrates (High risk with Inhibitors). Monitor therapy
Sympathomimetics: AtoMOXetine may enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Adverse Reactions
Percentages as reported in children and adults; some adverse reactions may be increased in "poor metabolizers" (CYP2D6). Frequency not always defined.
>10%:
Central nervous system: Headache (19%; children and adolescents), insomnia (1% to 19%), drowsiness (8% to 11%)
Dermatologic: Hyperhidrosis (4% to 15%)
Gastrointestinal: Xerostomia (17% to 35%), nausea (7% to 26%), decreased appetite (15% to 23%), abdominal pain (7% to 18%), vomiting (4% to 11%), constipation (1% to 11%)
Genitourinary: Erectile dysfunction (8% to 21%)
1% to 10%:
Cardiovascular: Increased diastolic blood pressure (5% to 9%; ≥15 mm Hg), systolic hypertension (4% to 5%), palpitations (3%), cold extremities (1% to 3%), syncope (≤3%), flushing (≥2%), orthostatic hypotension (≤2%), tachycardia (≤2%), prolonged Q-T interval on ECG
Central nervous system: Fatigue (6% to 10%), dizziness (5% to 8%), depression (4% to 7%), disturbed sleep (3% to 7%), irritability (5% to 6%), jitteriness (2% to 5%), abnormal dreams (4%), chills (3%), paresthesia (adults 3%; postmarketing observation in children), anxiety (≥2%), hostility (children and adolescents 2%), emotional lability (1% to 2%), agitation, restlessness, sensation of cold
Dermatologic: Excoriation (2% to 4%), skin rash (2%), pruritus, urticaria
Endocrine & metabolic: Weight loss (2% to 7%), decreased libido (3%), hot flash (3%), increased thirst (2%), menstrual disease
Gastrointestinal: Dyspepsia (4%), anorexia (3%), dysgeusia, flatulence
Genitourinary: Ejaculatory disorder (2% to 6%), urinary retention (1% to 6%), dysmenorrhea (3%), dysuria (2%), orgasm abnormal, pollakiuria, prostatitis, testicular pain, urinary frequency
Neuromuscular & skeletal: Tremor (1% to 5%), muscle spasm, weakness
Ophthalmic: Blurred vision (1% to 4%), conjunctivitis (1% to 3%), mydriasis
Respiratory: Pharyngolaryngeal pain
Miscellaneous: Therapeutic response unexpected (2%)
<1%, postmarketing, and/or case reports: Aggressive behavior, akathisia, alopecia, anaphylaxis, angioedema, cerebrovascular accident, change in libido, delusions, growth suppression (children), hallucination, hepatotoxicity, hypersensitivity reaction, hypoesthesia, hypomania, impulsivity, jaundice, lethargy, mania, myocardial infarction, panic attack, pelvic pain, priapism, Raynaud's phenomenon, rhabdomyolysis, seizure (including patients with no prior history or known risk factors for seizure), severe hepatic disease, suicidal ideation, tics
Warnings/Precautions
Concerns related to adverse effects:
- Aggressive behavior: New or worsening symptoms of hostility or aggressive behaviors have been associated with atomoxetine, particularly with the initiation of therapy.
- Allergic reactions: Anaphylactic reactions, angioneurotic edema, urticaria, and rash may occur (rare).
- Altered cardiac conduction: In clinical trials at therapeutic doses, atomoxetine consistently did not prolong the QT/QTc interval; however, one placebo-controlled study in healthy CYP2D6 poor metabolizers demonstrated a statistically significant increase in QTc with increasing atomoxetine concentrations (Loghin 2013; Martinez-Raga 2013). Case reports suggest that atomoxetine overdose may increase the QT interval; however, this occurred when atomoxetine was combined with other agents known to have QT prolongation potential or inhibit CYP2D6 (Barker 2004; Sawant 2004). Atomoxetine, at high concentrations ex vivo, has demonstrated hERG channel block (Scherer 2009).
- Cardiovascular events: Atomoxetine has been associated with serious cardiovascular events including sudden death in children and adolescents and sudden death, stroke, and MI in adult patients with preexisting structural cardiac abnormalities or other serious heart problems. Atomoxetine should be avoided in patients with known serious structural cardiac abnormalities, cardiomyopathy, serious heart rhythm abnormalities, coronary artery disease, or other serious cardiac problems that could increase the risk of sudden death that these conditions alone carry. Prior to initiating atomoxetine, assess medical history and family history of sudden death or ventricular arrhythmia; conduct a physical exam to assess for cardiac disease; patients should receive further evaluation if findings suggest cardiac disease, such as ECG and echocardiogram. Promptly conduct cardiac evaluation in patients who develop exertional chest pain, unexplained syncope, or any other symptoms of cardiac disease during atomoxetine treatment.
- Hepatotoxicity: Use may be associated with rare but severe liver injury, including hepatic failure; monitor liver enzymes upon any sign or symptom of liver dysfunction (eg, pruritus, dark urine, jaundice, right upper quadrant tenderness, unexplained flu-like symptoms); discontinue and do not restart in patients with jaundice or laboratory evidence of liver injury. The majority of reported cases occurred within 120 days of initiation of therapy.
- Priapism: Prolonged (>4 hours), painful, and nonpainful penile erections have been reported (rarely) in pediatric and adult patients. There are 3 published reports in boys ages 11 to 12 years (Armstrong 2015; Goetz 2014; Wadoo 2009), only one of whom was solely taking atomoxetine; another of the 3 was attributed to risperidone. Despite at least 22 cases involving methylphenidate (Baytunca 2016; Bozkurt 2017; Chauhan 2016; Eiland 2014; Esnafoglu 2017; Mann 2017; Unver 2017), a 2013 FDA warning states priapism appears to be more common in patients taking atomoxetine than in patients taking methylphenidate. In reports involving methylphenidate, amphetamines, or atomoxetine, priapism has been reported with different formulations, doses, following dose changes, and during periods of withdrawal. Patients with certain hematological dyscrasias (eg, sickle cell disease), malignancies, perineal trauma, or concomitant use of alcohol, illicit drugs, or other medications associated with priapism may be at increased risk (Eiland 2014). Patients who develop abnormally sustained or frequent and painful erections should discontinue therapy and seek immediate medical attention. In patients with severe cases of priapism that were slow to resolve and/or required detumescence by aspiration, avoidance of stimulants and atomoxetine may be preferred (Eiland 2014).
- Psychiatric effects: Treatment-emergent psychotic or manic symptoms (eg, hallucinations, delusional thinking, mania) may occur in children and adolescents without a prior history of psychotic illness or mania. Consider discontinuation of treatment if symptoms occur.
Disease-related concerns:
- ADHD and comorbidities: Randomized, controlled trials have demonstrated that atomoxetine does not worsen anxiety in patients with existing anxiety disorders or tics related to Tourette disorder.
- Bipolar disorder: Use caution in patients with comorbid bipolar disorder; therapy may induce mixed/manic episodes. Atomoxetine is not approved for major depressive disorder; patients presenting with depressive symptoms should be screened for bipolar disorder.
- Cardiovascular disorders: Atomoxetine may increase BP and heart rate (HR); most pediatric patients may experience a moderate increase in BP and/or HR; a large, pooled analysis reported more pronounced increases in BP (≥15 to 20 mm Hg) and HR (≥20 bpm) in 8% to 12% of pediatric patients (Reed 2016). CYP2D6 poor metabolizers may experience greater increases in BP and HR. Use with caution in patients with underlying conditions (eg, hypertension, tachycardia, cardiovascular or cerebrovascular disease) that could be worsened by BP or HR increases and in patients predisposed to hypotension or with conditions associated with abrupt HR or BP changes. Avoid use in patients with severe cardiac or vascular disorders that would be expected to deteriorate with clinically significant increases in BP.
- Hepatic impairment: Use with caution in patients with hepatic impairment; dosage adjustments necessary in moderate and severe hepatic insufficiency.
- Urinary retention: Use with caution in patients with a history of urinary retention or bladder outlet obstruction; may cause urinary retention/hesitancy.
Special populations:
- CYP2D6 poor metabolizers: Dosage adjustments are recommended in CYP2D6 poor metabolizers; these patients have increased exposure to atomoxetine.
- Pediatric: [US Boxed Warning]: Use with caution in pediatric patients; may be an increased risk of suicidal ideation. Closely monitor for clinical worsening, suicidality, or unusual changes in behavior; especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases. The family or caregiver should be instructed to closely observe the patient and communicate condition with health care provider. Growth should be monitored during treatment. Height and weight gain may be reduced during the first 9 to 12 months of treatment, but should recover by 3 years of therapy.
Other warnings/precautions:
- ADHD treatment: Appropriate use: Recommended to be used as part of a comprehensive treatment program for attention deficit disorders.
Monitoring Parameters
Liver enzymes (upon signs/symptoms of liver dysfunction and for several weeks after discontinuation for liver dysfunction). Cardiac evaluation should be completed at baseline and on any patient who develops exertional chest pain, unexplained syncope, and any symptom of cardiac disease during treatment. Monitor blood pressure and heart rate (baseline, following dose increases and periodically during treatment); growth (weight and height) and appetite in children; weight in adults; sleep and behavioral changes.
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse events have been observed in animal reproduction studies. Information related to atomoxetine use in pregnancy is limited; appropriate contraception is recommended for sexually active women of childbearing potential (Heiligenstein 2003).
Patient Education
What is this drug used for?
- It is used to treat attention deficit problems with hyperactivity.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Abdominal pain
- Trouble sleeping
- Nausea
- Vomiting
- Lack of appetite
- Dry mouth
- Constipation
- Loss of strength and energy
- Fatigue
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Vision changes
- Behavioral changes
- Irritability
- Agitation
- Panic attacks
- Sensing things that seem real but are not
- Fast heartbeat
- Abnormal heartbeat
- Severe headache
- Difficult urination
- Sexual dysfunction
- Erection that lasts more than 4 hours
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes.
- Chest pain
- Shortness of breath
- Severe dizziness
- Passing out
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.