Boxed Warning
Suicidality and antidepressant drugs:
Antidepressants increased the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term trials. These trials did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in subjects aged 65 and older.
In patients of all ages who are started on antidepressant therapy, monitor closely for worsening and for emergence of suicidal thoughts and behaviors. Advise families and caregivers of the need for close observation and communication with the prescriber. Bupropion is not approved for use in pediatric patients.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Tablet, Oral, as hydrochloride:
Wellbutrin: 75 mg [DSC], 100 mg [DSC]
Generic: 75 mg, 100 mg
Tablet Extended Release 12 Hour, Oral, as hydrochloride:
Buproban: 150 mg [DSC]
Wellbutrin SR: 100 mg, 150 mg, 200 mg
Zyban: 150 mg [DSC]
Generic: 100 mg, 150 mg, 200 mg
Tablet Extended Release 24 Hour, Oral, as hydrobromide:
Aplenzin: 174 mg, 348 mg, 522 mg
Tablet Extended Release 24 Hour, Oral, as hydrochloride:
Forfivo XL: 450 mg
Wellbutrin XL: 150 mg, 300 mg
Generic: 150 mg, 300 mg, 450 mg
Pharmacology
Mechanism of Action
Aminoketone antidepressant structurally different from all other marketed antidepressants; like other antidepressants the mechanism of bupropion's activity is not fully understood. Bupropion is a relatively weak inhibitor of the neuronal uptake of norepinephrine and dopamine, and does not inhibit monoamine oxidase or the reuptake of serotonin. Metabolite inhibits the reuptake of norepinephrine. The primary mechanism of action is thought to be dopaminergic and/or noradrenergic.
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid
Distribution
Vd: ~20 to 47 L/kg (Laizure 1985)
Metabolism
Extensively hepatic via CYP2B6 to hydroxybupropion; non-CYP-mediated metabolism to erythrohydrobupropion and threohydrobupropion. Metabolite activity ranges from 20% to 50% potency of bupropion.
Excretion
Urine (87%, primarily as metabolites); feces (10%, primarily as metabolites)
Onset of Action
1 to 2 weeks
Time to Peak
Bupropion: Immediate release: Within 2 hours; 12-hour extended release (sustained release): Within 3 hours; 24-hour extended release: ~5 hours; 12 hours (fed)
Metabolite: Hydroxybupropion: Immediate release: ~3 hours; Extended release: ~6 to 7 hours
Duration of Action
1 to 2 days
Half-Life Elimination
Distribution: 3 to 4 hours
Elimination:
Hydrochloride salt: ~21 hours after chronic dosing (± 9 hours); Metabolites (after a single dose): Hydroxybupropion: 20 ± 5 hours; Erythrohydrobupropion: 33 ± 10 hours; Threohydrobupropion: 37 ± 13 hours
Hydrobromide salt: 21 ± 7 hours; Metabolites: Hydroxybupropion: 24 ± 5 hours; Erythrohydrobupropion: 31 ± 8 hours; Threohydrobupropion: 51 ± 9 hours
Protein Binding
84%
Use in Specific Populations
Special Populations: Renal Function Impairment
Elimination of bupropion and/or major metabolites may be reduced.
Special Populations: Hepatic Function Impairment
Elimination of hydroxybupropion is reduced in patients with alcoholic liver disease. Bupropion Cmax increased 70%, AUC increased 3-fold, and mean half-life increased to 29 hours in patients with severe hepatic impairment. Mean half-life for active metabolites increased 2- to 5-fold in patients with severe hepatic impairment.
Special Populations: Elderly
May be at risk of accumulation of bupropion and its metabolites.
Special Populations: Gender
AUC was approximately 13% higher in men.
Use: Labeled Indications
Major depressive disorder (unipolar [excluding Zyban]): Treatment of major depressive disorder (MDD)
Seasonal affective disorder (24-hour extended release [Aplenzin, Wellbutrin XL]): Prevention of seasonal major depressive episodes in patients with a diagnosis of seasonal affective disorder (SAD)
Smoking cessation (12-hour extended release [sustained release; Zyban]): As an aid to smoking cessation treatment
Use: Off Label
Attention-deficit/hyperactivity disorderbyes
Data from a meta-analysis support the use of bupropion in the treatment of attention-deficit/hyperactivity disorder (ADHD) in adults Maneeton 2011.
Based on the
Bipolar depressionbyes
Data from a meta-analysis support the use of bupropion in the treatment of bipolar depression. Despite demonstrating the efficacy of bupropion, the authors of this meta-analysis caution that there is a risk of switching from depression to mania when bupropion is used for this indication Li 2016.
Based on the 2002 American Psychiatric Association (APA) guideline for the treatment of patients with bipolar disorder and the 2018 CANMAT and International Society for Bipolar Disorders guidelines for the management of patients with bipolar disorder, augmentation with bupropion is second-line for the management of bipolar depression that does not respond to preferred treatments. Due to inconsistencies in bupropion augmentation clinical trial results, the World Federation of Societies of Biological Psychiatry guidelines recommend bupropion augmentation of lithium or valproic acid as an option only in patients who are unresponsive to treatments with greater evidence.
Selective serotonin reuptake inhibitor-induced sexual dysfunction, augmentationbyes
Data from two randomized, double-blind, placebo-controlled trials support the use of bupropion as an augmentation strategy for increasing sexual desire, arousal, lubrication, orgasm, and satisfaction in patients with selective serotonin reuptake inhibitor (SSRI)-induced sexual dysfunction who have achieved remission on a serotonergic antidepressant Clayton 2004, Safarinejad 2011.
Based on the APA practice guideline for the treatment of patients with major depressive disorder, bupropion given for SSRI-induced sexual dysfunction is recommended for the management of side effects of arousal, erectile dysfunction, or orgasm dysfunction.
Contraindications
Hypersensitivity to bupropion or any component of the formulation; seizure disorder; history of anorexia/bulimia; patients undergoing abrupt discontinuation of ethanol or sedatives, including benzodiazepines, barbiturates, or antiepileptic drugs; use of MAO inhibitors (concurrently or within 14 days of discontinuing either bupropion or the MAO inhibitor); initiation of bupropion in a patient receiving linezolid or intravenous methylene blue
24-hour extended release: Additional contraindications: Other conditions that increase seizure risk, including arteriovenous malformation, severe head injury, severe stroke, CNS tumor, CNS infection
Canadian labeling: Additional contraindications (not in US labeling): Concurrent use or use within 14 days of thioridazine; concurrent use with other dosage forms of bupropion
Dosage and Administration
Dosing: Adult
Note: Bupropion is available as hydrochloride and hydrobromide salts. Doses are expressed in this monograph as hydrochloride salt except where noted as bupropion hydrobromide salt. Bupropion hydrochloride 150 mg is equivalent to about 174 mg of bupropion hydrobromide. Bupropion is available as immediate release, 12-hour extended release (sustained release), and 24-hour extended release tablets.
Attention-deficit/hyperactivity disorder (off-label use): Note: For patients with comorbid mood disorders or as an alternative agent for patients with substance use disorders (Brent 2019; CANMAT [Bond 2012]).
12-hour extended release (sustained release): Oral: Initial: 100 mg once daily in the morning; increase in 100 mg/day increments at intervals of 3 to 4 weeks based on response and tolerability up to 200 mg twice daily (Bukstein 2019; Reimherr 2005; Wilens 2001).
24-hour extended release: Oral: Initial: 150 mg once daily in the morning for 1 week; increase to 300 mg once daily for 3 weeks; may further increase dose based on response and tolerability up to 450 mg once daily (Wilens 2005).
Bipolar depression (off-label use): 12-hour extended release (sustained release): Oral: Initial: 100 mg once daily as an adjunct to mood stabilizer; increase based on response and tolerability at 2-week intervals up to 450 mg/day in 2 divided doses (average dose in clinical trials was 250 mg/day) (APA 2002; Grossman 1999; McIntyre 2002).
Major depressive disorder (unipolar): Note: Treatment should be periodically evaluated at appropriate intervals to ensure lowest effective dose is used. Slower dose titrations may be indicated based on patient care setting, symptom severity, and concern for side effects. May also be used as an alternative agent for patients with SSRI-induced sexual dysfunction (APA 2010).
Immediate release: Oral: Initial: 100 mg twice daily; after 3 days may increase to the usual dose of 100 mg 3 times a day; if no clinical improvement after several weeks, may increase to a maximum dose of 450 mg/day in 3 or 4 divided doses; do not exceed 150 mg in a single dose.
12-hour extended release (sustained release): Oral: Initial: 150 mg daily in the morning; if tolerated, after 3 days, may increase to a target dose of 150 mg twice daily; if no clinical improvement after several weeks, may increase to a maximum dose of 200 mg twice daily; do not exceed 200 mg in a single dose.
24-hour extended release: Oral:
Hydrochloride salt: Initial: 150 mg once daily in the morning; if tolerated, may increase as early as day 4 of dosing to 300 mg once daily; if no clinical improvement after 2 weeks, may increase to 450 mg once daily.
Hydrobromide salt: Initial: 174 mg once daily in the morning; may increase as early as day 4 of dosing to 348 mg once daily (target dose).
Seasonal affective disorder (SAD): 24-hour extended release: Oral:
Hydrochloride salt: Initial: 150 mg once daily in the morning; if tolerated, may increase after 7 days to 300 mg once daily in the morning.
Hydrobromide salt: Initial: 174 mg once daily in the morning; if tolerated, may increase after 7 days to 348 mg once daily in the morning.
Note: Prophylactic treatment should be reserved for patients with frequent depressive episodes and/or significant impairment. Initiate treatment in the autumn prior to symptom onset, and discontinue in early spring with dose tapering. Doses >300 mg daily (hydrochloride salt) or >348 mg daily (hydrobromide salt) have not been studied in SAD.
Selective serotonin reuptake inhibitor (SSRI)-induced sexual dysfunction, augmentation (off-label use): 12-hour extended release (sustained release): Oral: Initial: 150 mg once daily for the first 3 days; increase to 150 mg twice daily, based on response and tolerability (Clayton 2004; Safarinejad 2011).
Smoking cessation: Note: May be used as monotherapy or in combination with nicotine replacement therapy (Siu 2015): 12-hour extended release (sustained release): Oral: Initial: 150 mg once daily for 3 days; increase to 150 mg twice daily (maximum dose: 300 mg/day). For patients who do not tolerate titration to the full dose, consider continuing 150 mg once daily; the lower dose has shown efficacy (Hughes 2014).
Note: Therapy should begin at least 1 week before target quit date. Target quit dates are generally in the second week of treatment. If patient successfully quits smoking after 7 to 12 weeks but is not ready to discontinue treatment, may consider ongoing maintenance therapy based on individual patient risk:benefit. Efficacy of maintenance therapy (300 mg daily) has been demonstrated for up to 1 year. Conversely, if significant progress has not been made by the seventh week of therapy, success is unlikely; consider combination therapy, or discontinuation and use of an alternative agent.
Dosing conversion:
Immediate-, 12-hour (sustained release), and 24-hour extended-release formulations (hydrochloride salt): Convert using same total daily dose (up to the maximum recommended dose for a given dosage form), but adjust frequency as indicated for immediate (3 to 4 times daily), 12-hour extended (sustained release) (twice daily), or 24-hour extended (once daily) release products.
Hydrochloride salt formulation (immediate release, 12-hour (sustained release), or 24-hour extended release) to hydrobromide salt formulation (extended release):
Bupropion hydrochloride 150 mg daily is equivalent to bupropion hydrobromide 174 mg once daily.
Bupropion hydrochloride 300 mg daily is equivalent to bupropion hydrobromide 348 mg once daily.
Bupropion hydrochloride 450 mg daily is equivalent to bupropion hydrobromide 522 mg once daily.
MAOI recommendations: Switching to or from an MAOI antidepressant:
Allow 14 days to elapse between discontinuing an MAOI intended to treat depression and initiation of bupropion.
Allow 14 days to elapse between discontinuing bupropion and initiation of an MAOI intended to treat depression.
Discontinuation of therapy: Upon discontinuation of antidepressant therapy, gradually taper the dose (eg, over 2 to 4 weeks) to allow for the detection of reemerging symptoms. Withdrawal symptoms resulting from abrupt discontinuation are unlikely because bupropion has minimal serotonergic activity (APA 2010).
Dosing: Geriatric
Refer to adult dosing; use with caution.
Discontinuation of therapy: Refer to adult dosing.
MAOI recommendations: Refer to adult dosing.
Dosing: Pediatric
Note: Bupropion is available as either hydrochloride or hydrobromide (Aplenzin; not used in pediatric patients) salt formulations which are not interchangeable on a mg per mg basis; dosage expressed in terms of the salt formulation. Bupropion is available as immediate-release, 12-hour sustained-release, and 24-hour extended-release tablets. Patients must be able to swallow sustained or extended-release products whole.
Attention-deficit/hyperactivity disorder: Limited data available: Children ≥6 years (Dopheide 2009; Pliszka 2007) and Adolescents: Oral:
Immediate release, hydrochloride salts: Initial: 3 mg/kg/day in 2 to 3 divided doses; maximum initial dose: 150 mg/day; titrate dose as needed to a maximum daily dose of 6 mg/kg/day or 300 mg/day with no single dose >150 mg (Dopheide 2009; Pliszka 2007).
12-hour sustained release (Wellbutrin SR) and 24-hour extended release (Wellbutrin XL), hydrochloride salts: May be used in place of regular tablets, once the daily dose is titrated using the immediate release product and the titrated 12-hour dosage corresponds to a sustained release tablet (Wellbutrin SR) or the 24-hour dosage range corresponds to an extended release tablet size (Wellbutrin XL)
Depression, refractory to SSRIs: Limited data available; Note: May be most beneficial in patients with comorbid ADHD, conduct disorder, substance abuse problems or who want to quit smoking (Dopheide 2006). Treatment should be periodically evaluated at appropriate intervals to ensure lowest effective dose is used.
Immediate release, hydrochloride salt: Children 8 to ≤11 years: Oral: Initial: 37.5 mg twice daily; titrate to response; usual dosage range: 100 to 400 mg/day (Dopheide 2006)
12-hour sustained release, hydrochloride salt (Wellbutrin SR): Children ≥11 years and Adolescents: Oral: Initial: 2 mg/kg up to 100 mg administered as a morning dose; may titrate as needed every 2 to 3 weeks using the following titration schedule: Step 2: Increase up to 3 mg/kg every morning; Step 3: Increase up to 3 mg/kg every morning and 2 mg/kg at 5 pm (17:00); Step 4: Increase up to 3 mg/kg/dose twice daily; maximum dose: 150 mg; reported mean effective dose: Morning: 2.2 mg/kg and afternoon: 1.7 mg/kg (Daviss 2001)
24-hour extended release, hydrochloride salt (Wellbutrin XL): Children ≥12 years and Adolescents: Oral: Initial: 150 mg once daily; may titrate after 2 weeks to 300 mg once daily if adequate response not achieved; dosing based on a pharmacokinetic study in eight patients with depression (Daviss 2006); doses as high as 400 mg/day have been reported (Dopheide 2006); may also be used once the daily dose is titrated using the immediate release product and the 24-hour dosage range corresponds to an extended release tablet size (Wellbutrin XL).
Smoking cessation: Limited data available: Adolescents ≥14 years and ≥40.5 kg: 12-hour sustained release, hydrochloride salt (Buproban, Zyban): Oral: Initial: 150 mg once daily for 3 days; increase to 150 mg twice daily; treatment should start while the patient is still smoking in order to allow drug to reach steady-state levels prior to smoking cessation; generally, patients should stop smoking during the second week of treatment; maximum daily dose: 300 mg/day; short-term efficacy was demonstrated in 104 adolescents who received therapy for 7 weeks with cessation counseling (Muramoto 2007).
Dosing conversion between hydrochloride salt immediate (Wellbutrin), 12-hour sustained (Wellbutrin SR), and 24-hour extended-release (Wellbutrin XL) products: Convert using same total daily dose (up to the maximum recommended dose for a given dosage form), but adjust frequency as indicated for 12-hour sustained (twice daily) or for 24-hour extended (once daily) release products.
Discontinuation of therapy: Upon discontinuation of antidepressant therapy, gradually taper the dose to allow for the detection of reemerging symptoms. Withdrawal symptoms resulting from abrupt discontinuation are unlikely because bupropion has minimal serotonergic activity (APA 2010).
MAO inhibitor recommendations: Switching to or from an MAO inhibitor antidepressant:
Allow 14 days to elapse between discontinuing an MAO inhibitor intended to treat depression and initiation of bupropion.
Allow 14 days to elapse between discontinuing bupropion and initiation of an MAO inhibitor intended to treat depression.
Administration
Oral: May be taken without regard to meals. The manufacturer states that tablets should be swallowed whole; do not crush, chew, or divide.
Immediate release: Administer 3 to 4 times daily with at least 6 hours between successive doses; do not exceed 150 mg in a single dose.
12-hour extended release (sustained release): Administer 2 times daily with at least 8 hours between successive doses; do not exceed 200 mg in a single dose.
24-hour extended release: Administer once daily with at least 24 hours between successive doses.
Storage
Store at 15°C to 30°C (59°F to 86°F). Protect from light and moisture.
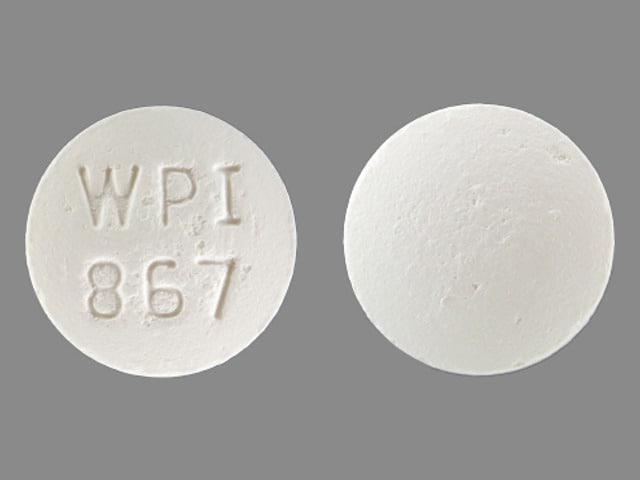
BuPROPion Images
Drug Interactions
Agents With Seizure Threshold Lowering Potential: BuPROPion may enhance the neuroexcitatory and/or seizure-potentiating effect of Agents With Seizure Threshold Lowering Potential. Monitor therapy
Ajmaline: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Ajmaline. Monitor therapy
Alcohol (Ethyl): May enhance the adverse/toxic effect of BuPROPion. Specifically, seizure threshold may be lowered. BuPROPion may enhance the adverse/toxic effect of Alcohol (Ethyl). Specifically, alcohol tolerance may decrease during treatment. Management: Patients receiving bupropion should be advised to minimize or avoid alcohol consumption due to possible lower alcohol tolerance, and lower seizure threshold associated with heavy alcohol consumption/abrupt discontinuation of heavy consumption. Consider therapy modification
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Antihepaciviral Combination Products: May decrease the serum concentration of BuPROPion. Monitor therapy
Anti-Parkinson Agents (Dopamine Agonist): May enhance the adverse/toxic effect of BuPROPion. Monitor therapy
ARIPiprazole: CYP2D6 Inhibitors (Strong) may increase the serum concentration of ARIPiprazole. Management: See full interaction monograph for details. Consider therapy modification
ARIPiprazole Lauroxil: CYP2D6 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of ARIPiprazole Lauroxil. Management: Please refer to the full interaction monograph for details concerning the recommended dose adjustments. Consider therapy modification
AtoMOXetine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of AtoMOXetine. Management: Initiate atomoxetine at a reduced dose (adult doses -- patients up to 70kg: 0.5mg/kg/day; patients 70kg or more: 40mg/day) in patients receiving a strong CYP2D6 inhibitor. Consider therapy modification
Benzhydrocodone: CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Benzhydrocodone. Monitor therapy
Brexanolone: BuPROPion may enhance the CNS depressant effect of Brexanolone. Monitor therapy
Brexpiprazole: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Brexpiprazole. Management: Reduce brexpiprazole dose to 50% of usual with a strong CYP2D6 inhibitor, reduce to 25% of usual if used with both a strong CYP2D6 inhibitor and a CYP3A4 inhibitor; these recommendations do not apply if treating major depressive disorder. Consider therapy modification
Citalopram: BuPROPion may enhance the adverse/toxic effect of Citalopram. Specifically, the risk for seizures and serotonin syndrome may be increased with this combination. BuPROPion may increase the serum concentration of Citalopram. Management: Initiate citalopram at the lower end of the normal dose range in patients receiving bupropion and consider limiting the maximum citalopram adult dose to 20 mg/day during concomitant bupropion treatment. Consider therapy modification
CloZAPine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of CloZAPine. Monitor therapy
Codeine: CYP2D6 Inhibitors (Strong) may diminish the therapeutic effect of Codeine. These CYP2D6 inhibitors may prevent the metabolic conversion of codeine to its active metabolite morphine. Consider therapy modification
CYP2B6 Inducers (Moderate): May decrease the serum concentration of CYP2B6 Substrates (High risk with Inducers). Monitor therapy
CYP2B6 Inhibitors (Weak): May increase the serum concentration of BuPROPion. Monitor therapy
CYP2D6 Substrates (High risk with Inhibitors): CYP2D6 Inhibitors (Strong) may decrease the metabolism of CYP2D6 Substrates (High risk with Inhibitors). Exceptions: Ajmaline; Dapoxetine; Indoramin; Metoprolol; Tamoxifen; Timolol (Ophthalmic); Tropisetron. Consider therapy modification
Dabrafenib: May decrease the serum concentration of CYP2B6 Substrates (High risk with Inducers). Monitor therapy
Dapoxetine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Dapoxetine. Monitor therapy
Deutetrabenazine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Deutetrabenazine. Management: The total daily dose of deutetrabenazine should not exceed 36 mg, and the maximum single dose of deutetrabenazine should not exceed 18 mg with concurrent use of a strong CYP2D6 inhibitor. Consider therapy modification
Digoxin: BuPROPion may decrease the serum concentration of Digoxin. Monitor therapy
Dipyrone: May decrease the serum concentration of BuPROPion. Monitor therapy
DOXOrubicin (Conventional): CYP2D6 Inhibitors (Strong) may increase the serum concentration of DOXOrubicin (Conventional). Management: Seek alternatives to strong CYP2D6 inhibitors in patients treated with doxorubicin whenever possible. One U.S. manufacturer (Pfizer Inc.) recommends that these combinations be avoided. Consider therapy modification
DULoxetine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of DULoxetine. Monitor therapy
Efavirenz: May decrease the serum concentration of BuPROPion. Management: Monitor for decreased response to bupropion in patients treated with efavirenz. Increased bupropion doses may be required. Avoid the use of naltrexone/bupropion for weight management in patients receiving efavirenz. Monitor therapy
Eliglustat: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Eliglustat. Management: Reduce the eliglustat dose to 84 mg daily. Avoid use of eliglustat in combination with a strong CYP2D6 inhibitor and a strong or moderate CYP3A4 inhibitor. Consider therapy modification
Escitalopram: BuPROPion may enhance the adverse/toxic effect of Escitalopram. Specifically, the risk for seizures and serotonin syndrome may be increased. Monitor therapy
Fesoterodine: CYP2D6 Inhibitors may increase serum concentrations of the active metabolite(s) of Fesoterodine. Monitor therapy
FLUoxetine: May enhance the neuroexcitatory and/or seizure-potentiating effect of BuPROPion. BuPROPion may increase the serum concentration of FLUoxetine. Monitor therapy
FluvoxaMINE: BuPROPion may enhance the adverse/toxic effect of FluvoxaMINE. Specifically, the risk for seizures and serotonin syndrome may be increased. Monitor therapy
Galantamine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Galantamine. Monitor therapy
HYDROcodone: CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of HYDROcodone. Specifically, concentrations of hydromorphone may be decreased. Monitor therapy
Iloperidone: CYP2D6 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Iloperidone. Specifically, concentrations of the metabolite P88 may be increased. CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Iloperidone. Specifically, concentrations of the metabolite P95 may be decreased. CYP2D6 Inhibitors (Strong) may increase the serum concentration of Iloperidone. Management: Reduce iloperidone dose by half when administered with a strong CYP2D6 inhibitor. Consider therapy modification
Indoramin: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Indoramin. Monitor therapy
Iobenguane Radiopharmaceutical Products: BuPROPion may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer bupropion until at least 7 days after each iobenguane dose. Avoid combination
Ioflupane I 123: BuPROPion may diminish the diagnostic effect of Ioflupane I 123. Monitor therapy
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Isavuconazonium Sulfate: May decrease the serum concentration of BuPROPion. Monitor therapy
Lofexidine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Lofexidine. Monitor therapy
Lopinavir: May decrease the serum concentration of BuPROPion. Concentrations of the active metabolite, hydroxybupropion, may also be decreased. Management: Monitor bupropion response closely. Significant bupropion dose adjustments may be necessary to maintain adequate response. Avoid the use of naltrexone/bupropion for weight management in patients receiving lopinavir. Monitor therapy
Lorcaserin: BuPROPion may enhance the serotonergic effect of Lorcaserin. This could result in serotonin syndrome. Management: Seek alternatives to this combination when possible. Consider therapy modification
Lumacaftor and Ivacaftor: May decrease the serum concentration of CYP2B6 Substrates (High risk with Inducers). Monitor therapy
Mequitazine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Mequitazine. Avoid combination
Metoclopramide: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Metoclopramide. Management: Reduce metoclopramide dose to 5 mg 4 times daily (30 minutes before each meal and at bedtime) and limit the maximum daily dose to 20 mg if combined with strong CYP2D6 inhibitors. Consider therapy modification
Metoprolol: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Metoprolol. Monitor therapy
MiFEPRIStone: May increase the serum concentration of CYP2B6 Substrates (High risk with Inhibitors). Monitor therapy
Monoamine Oxidase Inhibitors: May enhance the hypertensive effect of BuPROPion. Avoid combination
Nebivolol: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Nebivolol. Monitor therapy
Nicergoline: CYP2D6 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Nicergoline. Specifically, concentrations of the MMDL metabolite may be increased. CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Nicergoline. Specifically, concentrations of the MDL metabolite may be decreased. Monitor therapy
PARoxetine: BuPROPion may enhance the adverse/toxic effect of PARoxetine. Specifically, the risk for seizures and serotonin syndrome may be increased. Monitor therapy
Perhexiline: CYP2D6 Inhibitors may increase the serum concentration of Perhexiline. Management: Consider alternatives to this combination if possible. If combined, monitor for increased perhexiline serum concentrations and toxicities (eg, hypoglycemia, neuropathy, liver dysfunction). Perhexiline dose reductions will likely be required. Consider therapy modification
Pimozide: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Pimozide. Avoid combination
Pitolisant: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Pitolisant. Management: Reduce the pitolisant dose by 50% if a strong CYP2D6 inhibitor is initiated. For patients receiving strong CYP2D6 inhibitors, initiate pitolisant at 8.9 mg once daily and increase after 7 days to a maximum of 17.8 mg once daily. Consider therapy modification
Primaquine: CYP2D6 Inhibitors (Strong) may diminish the therapeutic effect of Primaquine. Management: Monitor for signs and symptoms of possible treatment failure with primaquine in patients who are taking strong CYP2D6 inhibitors. If efficacy of primaquine is compromised, may consider adjusting therapies. Consider therapy modification
Ritonavir: May decrease the serum concentration of BuPROPion. Mixed effects on concentrations of the active hydroxybupropion metabolite have been reported. Management: Monitor for decreased bupropion effects. Significant bupropion dose adjustments may be necessary to maintain adequate response. Avoid the use of naltrexone/bupropion for weight management in patients receiving ritonavir. Monitor therapy
Sertraline: BuPROPion may enhance the adverse/toxic effect of Sertraline. Specifically, the risk for seizures and serotonin syndrome may be increased. Monitor therapy
Solriamfetol: BuPROPion may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Tamoxifen: CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of Tamoxifen. Specifically, strong CYP2D6 inhibitors may decrease the metabolic formation of highly potent active metabolites. Avoid combination
Tamsulosin: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Tamsulosin. Monitor therapy
Tetrabenazine: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Tetrabenazine. Specifically, concentrations of the active alpha- and beta-dihydrotetrabenazine metabolites may be increased. Management: Tetrabenazine adult dose should be reduced by 50% when starting a strong CYP2D6 inhibitor. Maximum tetrabenazine adult dose is 50 mg/day when used with a strong CYP2D6 inhibitor. Consider therapy modification
Thioridazine: CYP2D6 Inhibitors may increase the serum concentration of Thioridazine. Avoid combination
Thiotepa: May increase the serum concentration of CYP2B6 Substrates (High risk with Inhibitors). Monitor therapy
Timolol (Ophthalmic): CYP2D6 Inhibitors (Strong) may increase the serum concentration of Timolol (Ophthalmic). Monitor therapy
TraMADol: CYP2D6 Inhibitors (Strong) may diminish the therapeutic effect of TraMADol. CYP2D6 Inhibitors (Strong) may decrease serum concentrations of the active metabolite(s) of TraMADol. CYP2D6 Inhibitors (Strong) may increase the serum concentration of TraMADol. Monitor therapy
Tricyclic Antidepressants: May enhance the neuroexcitatory and/or seizure-potentiating effect of BuPROPion. BuPROPion may increase the serum concentration of Tricyclic Antidepressants. Exceptions: Amoxapine; Protriptyline. Monitor therapy
Tropisetron: CYP2D6 Inhibitors (Strong) may increase the serum concentration of Tropisetron. Monitor therapy
Valbenazine: CYP2D6 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Valbenazine. Monitor therapy
Vilazodone: BuPROPion may enhance the adverse/toxic effect of Vilazodone. Specifically, the risk for seizures and serotonin syndrome may be increased. Monitor therapy
Vortioxetine: BuPROPion may enhance the adverse/toxic effect of Vortioxetine. Specifically, the risk for seizures and serotonin syndrome may be increased. BuPROPion may increase the serum concentration of Vortioxetine. Management: The vortioxetine dose should be reduced by 50% when used together with bupropion. Following cessation of bupropion, the vortioxetine dose should be returned to the normal level. Consider therapy modification
Test Interactions
May interfere with urine detection of amphetamine/methamphetamine (false-positive). Decreased prolactin levels.
Adverse Reactions
>10%:
Cardiovascular: Tachycardia (≤11%)
Central nervous system: Insomnia (11% to 40%), headache (25% to 34%), agitation (2% to 32%), dizziness (6% to 22%)
Dermatologic: Diaphoresis (5% to 22%)
Endocrine & metabolic: Weight loss (14% to 23%)
Gastrointestinal: Xerostomia (10% to 28%), constipation (8% to 26%), nausea and vomiting (23%), nausea (1% to 18%)
Neuromuscular & skeletal: Tremor (1% to 21%)
Ophthalmic: Blurred vision (3% to 15%)
Respiratory: Nasopharyngitis (13%), pharyngitis (3% to 13%), rhinitis (12%)
1% to 10%:
Cardiovascular: Palpitations (2% to 6%), cardiac arrhythmia (5%), chest pain (≤4%), flushing (≤4%), hypertension (1% to 4%; may be severe), hypotension (3%)
Central nervous system: Lack of concentration (9%), confusion (≤8%), anxiety (3% to 8%), hostility (≤6%), nervousness (4% to 5%), abnormal dreams (3% to 5%), abnormal sensory symptoms (4%), sleep disorder (4%), migraine (≤4%), irritability (3%), memory impairment (≤3%), drowsiness (2% to 3%), pain (3%), akathisia (≤2%), central nervous system stimulation (≤2%), paresthesia (≤2%), twitching (≤2%), dystonia (≥1%), abnormality in thinking (1%), depression
Dermatologic: Skin rash (1% to 8%), pruritus (2% to 4%), xeroderma (2%), urticaria (1% to 2%)
Endocrine & metabolic: Weight gain (9%), menstrual disease (2% to 5%), decreased libido (≤3%), hot flash (1% to 3%)
Gastrointestinal: Abdominal pain (2% to 9%), diarrhea (4% to 7%), flatulence (6%), anorexia (1% to 5%), dysgeusia (2% to 4%), increased appetite (2% to 4%), vomiting (≥1% to 4%), dyspepsia (3%), oral mucosa ulcer (2%), dysphagia (≤2%)
Genitourinary: Urinary frequency (≥1% to 5%), urinary urgency (≤2%), vaginal hemorrhage (≤2%), urinary tract infection (≤1%)
Hypersensitivity: Hypersensitivity reaction (1%)
Infection: Infection (8% to 9%)
Neuromuscular & skeletal: Myalgia (2% to 6%), arthralgia (4% to 5%), asthenia (4%), neck pain (2%), arthritis (≤2%), dyskinesia (≥1%)
Ophthalmic: Diplopia (≤3%)
Otic: Tinnitus (1% to 6%), auditory disturbance (5%)
Renal: Polyuria (≤1%)
Respiratory: Upper respiratory infection (9%), sinusitis (2% to 5%), cough (2% to 4%), increased cough (2% to 3%), epistaxis (2%), bronchitis (≤2%)
Miscellaneous: Accidental injury (2%), fever (1% to 2%)
<1%, postmarketing, and/or case reports: Abnormal stools, accommodation disturbance, acute myocardial infarction, aggressive behavior, akinesia, alopecia, amnesia, anaphylactic shock, anaphylaxis, anemia, angioedema, angle-closure glaucoma, aphasia, ataxia, atrioventricular block, bronchospasm, bruxism, cerebrovascular accident, change in prothrombin time, chills, colitis, coma, complete atrioventricular block, cutaneous lupus erythematosus (Hannah 2018), cystitis, deafness, delirium, delusion, depersonalization, derealization, drug-induced Parkinson disease, dry eye syndrome, dysarthria, dyspareunia, dysphoria, dysuria, ecchymoses, edema, EEG pattern changes, ejaculatory disorder, emotional lability, erythema multiforme, esophagitis, euphoria, exfoliative dermatitis, extrapyramidal reaction, extrasystoles, facial edema, gastric ulcer, gastroesophageal reflux disease, gastrointestinal hemorrhage, gingival hemorrhage, gingivitis, glossitis, glycosuria, gynecomastia, hallucination, hepatic injury, hepatic insufficiency, hepatitis, hirsutism, homicidal ideation, hyperglycemia, hyperkinetic muscle activity, hypertonia, hypoesthesia, hypoglycemia, hypokinesia, hypomania, hyponatremia, impotence, increased intraocular pressure, increased libido, increased thirst, inguinal hernia, intestinal perforation, jaundice, leukocytosis, leukopenia, lower limb cramp, lymphadenopathy, maculopapular rash, malaise, manic behavior, menopause, muscle rigidity, musculoskeletal chest pain, myasthenia, mydriasis, myoclonus, neuralgia, neuropathy, nonimmune anaphylaxis, orthostatic hypotension, painful erection, pancreatitis, pancytopenia, panic, paranoid ideation, peripheral edema, phlebitis, pneumonia, prostatic disease, psychiatric signs and symptoms, psychosis, pulmonary embolism, restlessness, rhabdomyolysis, salpingitis, sciatica, seizure (dose-related), serum sickness-like reaction, SIADH, sialorrhea, skin photosensitivity, Stevens-Johnson syndrome, stomatitis, subacute cutaneous lupus erythematosus (Hannah 2018), suicidal ideation, syncope, tardive dyskinesia, thrombocytopenia, tongue edema, type IV hypersensitivity reaction, urinary incontinence, urinary retention, vaginitis, vasodilation, vertigo
Warnings/Precautions
Major psychiatric warnings (use in treating psychiatric disorders):
- Suicidal thinking/behavior (use in treating psychiatric disorders): [US Boxed Warning]: Antidepressants increased the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term trials. These trials did not show an increase in the risk of suicidal thoughts and behavior with antidepressant use in subjects aged 65 and older. In patients of all ages who are started on antidepressant therapy, monitor closely for worsening and for emergence of suicidal thoughts and behaviors, particularly during the initial 1 to 2 months of therapy or during periods of dosage adjustments (increases or decreases); advise families and caregivers of the need for close observation and communication with the prescriber. A medication guide concerning the use of antidepressants should be dispensed with each prescription.
- The possibility of a suicide attempt is inherent in major depression and may persist until remission occurs. Worsening depression and severe abrupt suicidality that are not part of the presenting symptoms may require discontinuation or modification of drug therapy. Use caution in high-risk patients during initiation of therapy.
- Prescriptions should be written for the smallest quantity consistent with good patient care. The patient's family or caregiver should be alerted to monitor patients for the emergence of suicidality and associated behaviors such as anxiety, agitation, panic attacks, insomnia, irritability, hostility, impulsivity, akathisia, hypomania, and mania; patients should be instructed to notify their health care provider if any of these symptoms or worsening depression or psychosis occur.
Concerns related to adverse effects:
- CNS stimulation: May cause CNS stimulation (restlessness, anxiety, insomnia) or anorexia.
- Cognitive impairment: May cause motor or cognitive impairment in some patients, which may impair physical or mental abilities; patients must be cautioned about performing tasks which require mental alertness (eg, operating machinery or driving).
- Hypersensitivity reactions: Anaphylactoid/anaphylactic reactions have occurred, with symptoms of pruritus, urticaria, angioedema, and dyspnea. Serious reactions have been (rarely) reported, including erythema multiforme, Stevens-Johnson syndrome and anaphylactic shock. Arthralgia, myalgia, and fever with rash and other symptoms suggestive of delayed hypersensitivity resembling serum sickness have been reported.
- Hypertension: May elevate blood pressure and cause hypertension. Events have been observed in patients with or without evidence of preexisting hypertension. The risk is increased when used concomitantly with monoamine oxidase inhibitors, nicotine replacement, or other drugs that increase dopaminergic or noradrenergic activity. Assess blood pressure before treatment and monitor periodically.
- Mania/hypomania: May precipitate a shift to mania or hypomania in patients with bipolar disorder. Monotherapy in patients with bipolar disorder should be avoided. Combination therapy with an antidepressant and a mood stabilizer may be effective for acute treatment of bipolar major depressive episodes but should be avoided in acute mania or mixed episodes as well as maintenance treatment in bipolar disorder due to the mood-destabilizing effects of antidepressants (CANMAT [Yatham 2018]; WFSBP [Grunze 2018]). Patients presenting with depressive symptoms should be screened for bipolar disorder. Bupropion is not FDA-approved for the treatment of bipolar depression.
- Neuropsychiatric effect (use in smoking cessation): Serious neuropsychiatric events have occurred in patients taking bupropion for smoking cessation, including changes in mood (eg, depression, mania), psychosis, hallucinations, paranoia, delusions, homicidal ideation, hostility, agitation, aggression, anxiety, panic, suicidal ideation, suicide attempt, and completed suicide. The majority occurred during bupropion treatment; some occurred during treatment discontinuation. A causal relationship is uncertain as depressed mood may be a symptom of nicotine withdrawal. Some cases also occurred in patients taking bupropion who continued to smoke. Neuropsychiatric effects occurred in patients with and without preexisting psychiatric disease; some patients experienced a worsening of their psychiatric illnesses. However, subsequent controlled trials in patients with or without psychiatric disorders have not identified significant differences in neuropsychiatric effects for patients taking bupropion, varenicline, nicotine patches, or placebo (Anthenelli 2016; Cinciripini 2013). Observe all patients taking bupropion for neuropsychiatric reactions. Instruct patients to stop taking bupropion and contact a health care provider if neuropsychiatric reactions occur.
- Ocular effects: May cause mild pupillary dilation, which in susceptible individuals can lead to an episode of narrow-angle glaucoma. Consider evaluating patients who have not had an iridectomy for narrow-angle glaucoma risk factors.
- Psychosis: May cause delusions, hallucinations, psychosis, concentration disturbance, paranoia, and confusion; most common in patients with an underlying psychiatric illness. Symptoms may abate with dose reduction and/or withdrawal of treatment.
- Seizures: May cause a dose-related risk of seizures. Use is contraindicated in patients with a history of seizures or certain conditions with high seizure risk (eg, history of anorexia/bulimia or patients undergoing abrupt discontinuation of ethanol, benzodiazepines, barbiturates, or antiepileptic drugs); 24-hour ER formulations are also contraindicated in patients with certain conditions with high seizure risk (eg, arteriovenous malformation, severe head injury, severe stroke, CNS tumor, and CNS infection). Use caution with concurrent use of antipsychotics, antidepressants, theophylline, systemic corticosteroids, stimulants (including cocaine), anorexiants, or hypoglycemic agents, or with excessive use of ethanol, benzodiazepines, sedative/hypnotics, or opioids. Use with caution in seizure-potentiating metabolic disorders (hypoglycemia, hyponatremia, severe hepatic impairment, and hypoxia). The dose-dependent risk of seizures may be reduced by gradual dose increases and by not exceeding the maximum daily dose. Do not coadminister with other bupropion-containing formulations. Permanently discontinue if seizure occurs during therapy. Chewing, crushing, injecting, or dividing long-acting products may increase seizure risk.
- Sexual dysfunction: The incidence of sexual dysfunction with bupropion is generally lower than with selective serotonin reuptake inhibitors (Clayton 2004).
- Weight loss: May cause weight loss; use caution in patients where weight loss is not desirable.
Disease-related concerns:
- Attention-deficit/hyperactivity disorder (off-label use): All children diagnosed with attention-deficit/hyperactivity disorder who may be candidates for stimulant medications should have a thorough cardiovascular assessment to identify risk factors for sudden cardiac death prior to initiation of drug therapy.
- Cardiovascular disease: Use with caution in patients with cardiovascular disease, history of hypertension, or coronary artery disease; treatment-emergent hypertension (including some severe cases) has been reported, both with bupropion alone and in combination with nicotine transdermal systems.
- Hepatic impairment: Use with caution in patients with hepatic impairment; consider a reduction in dose and/or frequency.
- Renal impairment: Use with caution in patients with renal impairment; consider a reduction in dose and/or frequency.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use with caution in elderly patients; may be at greater risk of drug accumulation during chronic dosing. Consider a reduction in dose.
Dosage form specific issues:
- 24-hour ER tablet: Insoluble tablet shell may remain intact and be visible in the stool.
Other warnings/precautions:
- Abuse/misuse: Using doses higher than prescribed may result in increased motor activity, agitation/excitement and euphoria. Inhalation of crushed tablets or injection of dissolved bupropion has been reported, some resulting in seizures and death.
- Electroconvulsive therapy: May increase the risks associated with electroconvulsive therapy (ECT); consider discontinuing, when possible, prior to ECT treatment (APA 2010).
Monitoring Parameters
Body weight; mental status for depression, suicidal ideation (especially at the beginning of therapy or when doses are increased or decreased), anxiety, social functioning, mania, panic attacks; blood pressure (baseline and periodically especially when used in conjunction with nicotine transdermal replacement); renal and hepatic function
When used for the treatment of ADHD, thoroughly evaluate for cardiovascular risk. Monitor heart rate, blood pressure, and consider obtaining ECG prior to initiation (Vetter 2008).
Pregnancy
Pregnancy Considerations
Bupropion and its metabolites cross the placenta (Fokina 2016).
An increased risk of congenital malformations has not been observed following maternal use of bupropion during pregnancy; however, data specific to cardiovascular malformations is inconsistent. The long-term effects on development and behavior have not been studied.
Therapy with antidepressants during pregnancy should be individualized (ACOG 2008). Psychotherapy or other nonmedication therapies may be considered for some women; however, antidepressant medication should be considered for pregnant women with moderate to severe major depressive disorder (APA 2010). If treatment for MDD is initiated for the first time during pregnancy, agents other than bupropion are preferred (MacQueen 2016). Treatment algorithms have been developed by the ACOG and the APA for the management of depression in women prior to conception and during pregnancy (ACOG 2008; APA 2010; Yonkers 2009).
There is insufficient information related to the use of bupropion to recommend use for smoking cessation during pregnancy (ACOG 721 2017).
Pregnant women exposed to antidepressants during pregnancy are encouraged to enroll in the National Pregnancy Registry for Antidepressants (NPRAD). Women 18 to 45 years of age or their health care providers may contact the registry by calling 844-405-6185. Enrollment should be done as early in pregnancy as possible.
Patient Education
What is this drug used for?
- It is used to treat low mood (depression).
- It is used to treat seasonal affective disorder (SAD).
- It is used to help you stop smoking.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Abdominal pain
- Tremors
- Nightmares
- Nausea
- Vomiting
- Constipation
- Passing gas
- Dry mouth
- Trouble sleeping
- Stuffy nose
- Sore throat
- Sweating a lot
- Lack of appetite
- Tablet shell in stool
- Weight gain or loss
- Joint pain
- Muscle pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Depression like thoughts of suicide, anxiety, emotional instability, agitation, irritability, panic attacks, mood changes, behavioral changes, or confusion
- Confusion
- Seizures
- Thoughts of homicide
- Forceful actions
- Anger
- Sensing things that seem real but are not
- Severe headache
- Severe dizziness
- Passing out
- Chest pain
- Fast heartbeat
- Abnormal heartbeat
- Swelling
- Shortness of breath
- Hearing changes
- Noise or ringing in the ears
- Passing a lot of urine
- Swollen glands
- Trouble moving
- Trouble focusing
- Vision changes
- Eye pain
- Eye irritation
- Eye redness
- Eye swelling
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.