Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Intravenous, as sodium [strength expressed as base, preservative free]:
Zinacef in Sterile Water: 1.5 g (50 mL [DSC])
Solution Reconstituted, Injection, as sodium [strength expressed as base]:
Zinacef: 750 mg (1 ea [DSC]); 1.5 g (1 ea [DSC]); 7.5 g (1 ea [DSC])
Generic: 750 mg (1 ea [DSC])
Solution Reconstituted, Injection, as sodium [strength expressed as base, preservative free]:
Generic: 750 mg (1 ea); 7.5 g (1 ea)
Solution Reconstituted, Intravenous, as sodium [strength expressed as base]:
Zinacef: 750 mg (1 ea [DSC]); 1.5 g (1 ea [DSC])
Solution Reconstituted, Intravenous, as sodium [strength expressed as base, preservative free]:
Generic: 1.5 g (1 ea)
Suspension Reconstituted, Oral, as axetil [strength expressed as base]:
Ceftin: 125 mg/5 mL (100 mL [DSC]); 250 mg/5 mL (50 mL [DSC], 100 mL [DSC]) [contains aspartame; tutti-frutti flavor]
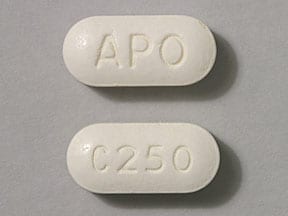
Tablet, Oral, as axetil [strength expressed as base]:
Ceftin: 250 mg [DSC], 500 mg [DSC]
Generic: 250 mg, 500 mg
Pharmacology
Mechanism of Action
Inhibits bacterial cell wall synthesis by binding to one or more of the penicillin-binding proteins (PBPs) which in turn inhibits the final transpeptidation step of peptidoglycan synthesis in bacterial cell walls, thus inhibiting cell wall biosynthesis. Bacteria eventually lyse due to ongoing activity of cell wall autolytic enzymes (autolysins and murein hydrolases) while cell wall assembly is arrested.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral tablet: Increases with food
Distribution
Widely to body tissues and fluids including bronchial secretions, synovial and pericardial fluid, kidneys, heart, liver, bone and bile; crosses blood-brain barrier
Metabolism
Cefuroxime axetil (oral) is hydrolyzed in the intestinal mucosa and blood to cefuroxime.
Excretion
Urine (66% to 100% as unchanged drug)
Time to Peak
Serum: IM: ~15 to 60 minutes; IV: 2 to 3 minutes; Oral: Children: ~3 to 4 hours; Adults: ~2 to 3 hours
Half-Life Elimination
Premature neonates:
PNA ≤3 days: Median: 5.8 hours (de Louvois 1982)
PNA ≥8 days: Median: 1.6 to 3.8 hours (de Louvois 1982)
Children and Adolescents: 1.4 to 1.9 hours
Adults: ~1 to 2 hours; prolonged with renal impairment
Protein Binding
33% to 50%
Use: Labeled Indications
Bone and joint infections (injection only): Treatment of bone and joint infections caused by Staphylococcus aureus (penicillinase- and non-penicillinase-producing strains).
Chronic obstructive pulmonary disease, acute exacerbation (tablets only): Treatment of mild to moderate acute bacterial exacerbations of chronic bronchitis in adults and adolescents ≥13 years of age caused by Streptococcus pneumoniae, Haemophilus influenzae (beta-lactamase negative strains), or Haemophilus parainfluenzae (beta-lactamase negative strains).
Lower respiratory tract infections (injection only): Treatment of lower respiratory tract infections, including pneumonia, caused by S. pneumoniae, H. influenzae (including ampicillin-resistant strains), Klebsiella spp., S. aureus (penicillinase- and non-penicillinase-producing strains), Streptococcus pyogenes, and Escherichia coli.
Lyme disease (early) (tablets only): Treatment of adults and adolescents ≥13 years of age with early Lyme disease caused by Borrelia burgdorferi.
Otitis media, acute (tablets and oral suspension only): Treatment of pediatric patients ≥3 months of age with acute bacterial otitis media caused by S. pneumoniae, H. influenzae (including beta-lactamase-producing strains), Moraxella catarrhalis (including beta-lactamase-producing strains), or S. pyogenes.
Pharyngitis/tonsillitis (tablets and oral suspension only): Treatment of mild to moderate pharyngitis/tonsillitis caused by S. pyogenes in adults and pediatric patients ≥3 months of age.
Limitations of use: Efficacy in the prevention of rheumatic fever has not been established in clinical trials. Efficacy in the treatment of penicillin-resistant strains of S. pyogenes has not been demonstrated.
Septicemia (injection only): Treatment of septicemia caused by S. aureus (penicillinase- and non-penicillinase-producing strains), S. pneumoniae, E. coli, H. influenzae (including ampicillin-resistant strains), and Klebsiella spp.
Sinusitis, acute bacterial (tablets and oral suspension only): Treatment of mild to moderate acute bacterial maxillary sinusitis caused by S. pneumoniae or H. influenzae (non-beta-lactamase-producing strains only).
Limitations of use: Effectiveness for sinus infections caused by beta-lactamase-producing H. influenzae or M. catarrhalis in patients with acute bacterial maxillary sinusitis has not been established. Note: According to the IDSA guidelines for acute bacterial rhinosinusitis, cefuroxime is no longer recommended as monotherapy for initial empiric treatment (IDSA [Chow 2012]).
Skin and skin-structure infections (impetigo) (oral suspension only): Treatment of pediatric patients 3 months to 12 years of age with skin or skin-structure infections (impetigo) caused by S. aureus (including beta-lactamase-producing strains) or S. pyogenes.
Skin and skin-structure infections (injection; tablets [uncomplicated infections only]): Treatment of adults and pediatric patients >3 months of age with skin and skin-structure infections (including impetigo) caused by S. aureus (penicillinase- and non-penicillinase-producing strains), S. pyogenes, E. coli, Klebsiella spp., and Enterobacter spp.
Surgical prophylaxis (injection only): Prophylaxis of infection in patients undergoing surgical procedures that are classified as clean-contaminated or potentially contaminated procedures.
Urinary tract infections (tablets and injection only): Treatment of adults and pediatric patients >3 months of age with urinary tract infections caused by E. coli and Klebsiella spp.
Use: Off Label
Bite wound, prophylaxis or treatment (animal or human bite)cyes
Based on the Infectious Diseases Society of America (IDSA) guidelines for the diagnosis and management of skin and soft tissue infections (SSTIs), cefuroxime, in combination with an agent appropriate for anaerobes, is an effective and recommended alternative option for prophylaxis and treatment of animal bite wounds.
Clinical experience also suggests the utility of cefuroxime as an alternative agent for prophylaxis and treatment of human bite wounds Baddour 2019a.
Intraabdominal infection, community-acquired (mild to moderate infection in low-risk patients)yes
Based on the Surgical Infection Society/IDSA guidelines for the diagnosis and management of complicated intraabdominal infection in adults and children, cefuroxime, in combination with metronidazole, is an effective and recommended empiric treatment option for the management of community-acquired intraabdominal infection, and, as monotherapy, for the management of mild to moderate acute cholecystitis.
Lyme disease (Borrelia spp. infection), early disseminated or late diseaseyes
Based on the IDSA guidelines for the clinical assessment, treatment, and prevention of Lyme disease, human granulocytic anaplasmosis, and babesiosis, cefuroxime is effective and recommended for the treatment of early disseminated Lyme disease (isolated facial nerve palsy [alternative agent] or mild carditis) or late Lyme disease (arthritis without neurologic involvement).
Contraindications
Hypersensitivity to cefuroxime, any component of the formulation, or other beta-lactam antibacterial drugs (eg, penicillins and cephalosporins)
Dosage and Administration
Dosing: Adult
Note: Ceftin oral suspension has been discontinued in the US for more than 1 year.
Bite wound, prophylaxis or treatment (animal or human bite) (alternative agent) (off-label use): Oral: 500 mg twice daily, in combination with an agent appropriate for anaerobes (Baddour 2019a; IDSA [Stevens 2014]). Duration of prophylaxis is 3 to 5 days (IDSA [Stevens 2014]). Duration of treatment for established infection typically ranges from 5 to 14 days and varies based on clinical response and patient-specific factors (Baddour 2019a; Baddour 2019b).
Chronic obstructive pulmonary disease, acute exacerbation: Oral: 250 to 500 mg twice daily for 5 to 7 days (GOLD 2018; Yoon 2013). Note: Some experts reserve cefuroxime for patients with uncomplicated COPD (eg, age <65 years without major comorbidities, FEV1 >50% predicted, infrequent exacerbations) (Anzueto 2007; Sethi 2008).
Intraabdominal infection, community-acquired (mild to moderate infection in low-risk patients) (off-label use):
Cholecystitis, acute: IV: 1.5 g every 8 hours; continue for 1 day after gallbladder removal or until clinical resolution in patients managed nonoperatively (SIS/IAI [Mazuski 2017]; SIS/IDSA [Solomkin 2010]; Vollmer 2019). Note: The addition of anaerobic therapy is recommended if biliary-enteric anastomosis is present (SIS/IDSA [Solomkin 2010]).
Other intraabdominal infections (eg, perforated appendix, diverticulitis, intraabdominal abscess): IV: 1.5 g every 8 hours in combination with metronidazole. May switch to an oral regimen when clinically improved and able to tolerate an oral diet. Total duration of therapy is for 4 to 7 days following adequate source control (SIS/IAI [Mazuski 2017]; SIS/IDSA [Solomkin 2010]); for infections managed without surgical or percutaneous intervention, a longer duration may be necessary (Barshak 2019; Pemberton 2019).
Lyme disease (Borrelia spp. infection):
Early localized (eg, erythema migrans): Oral: 500 mg twice daily for 14 to 21 days (IDSA [Wormser 2006])
Early disseminated, carditis (initial therapy for mild disease [first-degree atrioventricular block with PR interval <300 msec] or step-down therapy after initial parenteral treatment for more severe disease once PR interval <300 msec) (off-label use): Oral: 500 mg twice daily for 14 to 21 days (Hu 2019; IDSA [Wormser 2006]); for step-down therapy, some experts prefer a total duration of 21 to 28 days (Hu 2019).
Early disseminated, mild neurologic involvement (isolated facial nerve palsy [no evidence of meningitis]) (alternative agent) (off-label use): Oral: 500 mg twice daily for 14 to 21 days (IDSA [Wormser 2006])
Late disease, arthritis without neurologic involvement (off-label use): Oral: 500 mg twice daily for 28 days (IDSA [Wormser 2006]). Some experts reserve cefuroxime for patients who cannot take doxycycline or amoxicillin (Hu 2019).
Otitis media, acute (alternative agent for mild [non-anaphylactic] penicillin allergy) (off-label): Oral: 500 mg twice daily; duration of therapy is 5 to 7 days (mild to moderate infection) or 10 days (severe infection) (Limb 2019).
Pneumonia, community-acquired, outpatient empiric therapy or pathogen-directed therapy (alternative agent):
Note: For directed therapy of community-acquired pneumonia due to S. pneumoniae, use only if the penicillin MIC is <2 mcg/mL (IDSA/ATS [Mandell 2007]).
Oral: 500 mg twice daily; when used for empiric therapy, use as part of an appropriate combination regimen. Duration is for a minimum of 5 days and varies based on disease severity and response to therapy; patients should be afebrile for ≥48 hours and clinically stable before discontinuing therapy (IDSA/ATS [Mandell 2007]).
Streptococcal pharyngitis (group A) (alternative agent for mild [non-anaphylactic] penicillin allergy): Oral: 250 mg twice daily for 10 days (Pichichero 2019; manufacturer's labeling)
Surgical prophylaxis (eg, cardiac surgery, head and neck surgery) (alternative agent): IV: 1.5 g within 60 minutes prior to surgical incision; use in combination with metronidazole for select head and neck procedures. Cefuroxime dose may be repeated intraoperatively in 4 hours if procedure is lengthy or if there is excessive blood loss (ASHP/IDSA/SIS/SHEA [Bratzler 2013]). In cases where an extension of prophylaxis is warranted postoperatively, total duration should be ≤24 hours (Anderson 2014; ASHP/IDSA/SIS/SHEA [Bratzler 2013]). Postoperative prophylaxis is not recommended in clean and clean-contaminated surgeries (CDC [Berríos-Torres 2017]).
Urinary tract infection (alternative agent): Acute uncomplicated cystitis or acute simple cystitis (infection limited to bladder and no signs/symptoms of upper tract or systemic infection): Oral: 250 mg twice daily for 5 to 7 days (Hooton 2019a; Hooton 2019b; manufacturer's labeling). Note: Although evidence is limited, some experts recommend the use of beta-lactams, such as cefuroxime, when first-line agents cannot be used (efficacy of oral beta-lactams in this setting is decreased compared to other agents) (Hooton 2019a; Hooton 2019b; IDSA/ESCMID [Gupta 2011]).
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Ceftin oral suspension has been discontinued in the US for >1 year.
Note: Cefuroxime axetil film-coated tablets and oral suspension are not bioequivalent and are not substitutable on a mg/mg basis.
General dosing, susceptible infection (Red Book [AAP 2015]): Infants, Children, and Adolescents:
Mild to moderate infection:
Oral: 20 to 30 mg/kg/day divided twice daily; maximum dose: 500 mg/dose
IM, IV: 75 to 100 mg/kg/day divided in 3 doses; maximum dose: 1,500 mg/dose
Severe infection: IM, IV: 100 to 200 mg/kg/day divided in 3 to 4 doses; maximum dose: 1,500 mg/dose
Bone and joint infection: Infants ≥3 months, Children, and Adolescents: IM, IV: 50 mg/kg/dose every 8 hours; maximum dose: 1,500 mg/dose. Note: Upon completion of parenteral therapy follow with oral antibiotic therapy if indicated.
Bronchitis, chronic; acute exacerbations: Adolescents: Oral tablets: 250 to 500 mg every 12 hours for 10 days
Impetigo: Infants ≥3 months and Children: Oral suspension: 15 mg/kg/dose twice daily for 10 days; maximum dose: 500 mg/dose
Intra-abdominal infection complicated, community-acquired: Infants, Children, and Adolescents: IV: 150 mg/kg/day in divided doses every 6 to 8 hours; maximum dose: 1,500 mg/dose (IDSA [Solomkin 2010])
Lyme disease: Infants, Children, and Adolescents:
Acrodermatitis chronica atrophicans: Oral: 15 mg/kg/dose every 12 hours for 21 days; maximum dose: 500 mg/dose (Wormser 2006)
Early localized disease: Oral: 15 mg/kg/dose every 12 hours for 14 days; maximum dose: 500 mg/dose (Red Book [AAP 2015]; Wormser 2006)
Late disease (arthritis): Oral: 15 mg/kg/dose every 12 hours for 28 days; maximum dose: 500 mg/dose (Wormser 2006)
Otitis media, acute: Infants ≥3 months and Children:
Oral suspension: 15 mg/kg/dose twice daily for 10 days; maximum dose: 500 mg/dose
Oral tablet (patients able to swallow tablet whole): 250 mg twice daily for 10 days
Note: AAP recommends variable duration of therapy depending on age: If 6 months to 2 years of age or severe symptoms (any age): 10-day course; if 2 to 5 years of age with mild to moderate symptoms: 7-day course; if ≥6 years of age with mild to moderate symptoms: 5- to 7-day course (AAP [Lieberthal 2013])
Pharyngitis/tonsillitis:
Infants ≥3 months and Children: Oral suspension: 10 mg/kg/dose twice daily for 10 days; maximum dose: 250 mg/dose
Adolescents: Oral tablets: 250 mg twice daily for 10 days
Pneumonia, bacterial (HIV-exposed/-positive): Infants and Children: IV: 35 to 50 mg/kg/dose 3 times daily; maximum dose: 2,000 mg/dose (HHS [OI pediatric 2016])
Sinusitis:
Infants ≥3 months and Children:
Oral suspension: 15 mg/kg/dose twice daily for 10 days; maximum dose: 500 mg/dose
Oral tablet (for patients able to swallow tablet whole): 250 mg twice daily for 10 days
Adolescents: Oral tablet: 250 mg twice daily for 10 days
Skin and skin structure infections, uncomplicated: Adolescents: Oral tablet: 250 to 500 mg twice daily for 10 days
Surgical prophylaxis: Children and Adolescents: IV: 50 mg/kg within 60 minutes prior to procedure; may repeat dose in 4 hours if procedure is lengthy or if there is excessive blood loss; maximum dose: 1,500 mg/dose (Bratzler 2013)
Urinary tract infection, uncomplicated:
Infants and Children 2 to 24 months: Oral suspension: 10 to 15 mg/kg/dose twice daily (AAP 2011)
Children >24 months: Moderate to severe disease (possible pyelonephritis): Oral suspension: 20 to 30 mg/kg/day divided twice daily; maximum dose: 500 mg/dose (Bradley 2017)
Adolescents: Oral tablet: 250 mg twice daily for 7 to 10 days
Reconstitution
Oral suspension: Refer to manufacturer's product labeling for reconstitution instructions.
Duplex container: Unlatch side tab, unfold, and remove foil strip from drug chamber. Point set port in downward direction, fold container just below the diluent meniscus, and squeeze the diluent chamber until the seal between the diluent and drug powder opens. Shake until dissolved.
Administration
Oral suspension: Administer with food. Shake well before use.
Oral tablet: May administer with or without food. Swallow tablet whole (crushed tablet has strong, persistent, bitter taste).
IM: Inject deep IM into large muscle mass.
IV: Inject direct IV over 3 to 5 minutes. Infuse intermittent infusion over 15 to 30 minutes.
Dietary Considerations
Some products may contain phenylalanine and/or sodium.
Oral suspension: Should be taken with food.
Storage
Injection: Store intact vials at 15°C to 30°C (59°F to 86°F); protect from light. Reconstituted solution is stable for 24 hours at room temperature and 48 hours when refrigerated. IV infusion in NS or D5W solution is stable for 24 hours at room temperature, 7 days when refrigerated, or 26 weeks when frozen. After freezing, thawed solution is stable for 24 hours at room temperature or 21 days when refrigerated.
Duplex container: Store unactivated units at 20°C to 25°C (68°F to 77°F). Unactivated units with foil strip removed from the drug chamber must be protected from light and used within 7 days. Once activated, may be stored for up to 24 hours at room temperature or for 7 days under refrigeration. Do not freeze.
TwistVial vials: Joined, but not activated, vials are stable for 14 days. Once activated, stable for 24 hours at room temperature and 7 days refrigerated. Do not freeze.
Premix Galaxy plastic containers: Store frozen at -20°C. Thaw container at room temperature or under refrigeration; do not force thaw. Thawed solution is stable for 24 hours at room temperature and 28 days refrigerated; do not refreeze.
Oral suspension: Prior to reconstitution, store at 2°C to 30°C (36°F to 86°F). Reconstituted suspension is stable for 10 days at 2°C to 8°C (36°F to 46°F).
Tablet: Store at 15°C to 30°C (59°F to 86°F).
Cefuroxime Images
Drug Interactions
Aminoglycosides: Cephalosporins (2nd Generation) may enhance the nephrotoxic effect of Aminoglycosides. Monitor therapy
Antacids: May decrease the serum concentration of Cefuroxime. Management: Administer cefuroxime axetil at least 1 hour before or 2 hours after the administration of short-acting antacids. Consider therapy modification
BCG (Intravesical): Antibiotics may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
BCG Vaccine (Immunization): Antibiotics may diminish the therapeutic effect of BCG Vaccine (Immunization). Monitor therapy
Cholera Vaccine: Antibiotics may diminish the therapeutic effect of Cholera Vaccine. Management: Avoid cholera vaccine in patients receiving systemic antibiotics, and within 14 days following the use of oral or parenteral antibiotics. Avoid combination
Histamine H2 Receptor Antagonists: May decrease the absorption of Cefuroxime. Separate oral doses by at least 2 hours. Avoid combination
Lactobacillus and Estriol: Antibiotics may diminish the therapeutic effect of Lactobacillus and Estriol. Monitor therapy
Probenecid: May increase the serum concentration of Cephalosporins. Monitor therapy
Proton Pump Inhibitors: May decrease the absorption of Cefuroxime. Avoid combination
Sodium Picosulfate: Antibiotics may diminish the therapeutic effect of Sodium Picosulfate. Management: Consider using an alternative product for bowel cleansing prior to a colonoscopy in patients who have recently used or are concurrently using an antibiotic. Consider therapy modification
Typhoid Vaccine: Antibiotics may diminish the therapeutic effect of Typhoid Vaccine. Only the live attenuated Ty21a strain is affected. Management: Vaccination with live attenuated typhoid vaccine (Ty21a) should be avoided in patients being treated with systemic antibacterial agents. Use of this vaccine should be postponed until at least 3 days after cessation of antibacterial agents. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Cephalosporins may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Test Interactions
Positive direct Coombs', false-positive urinary glucose test using cupric sulfate (Benedict's solution, Clinitest®, Fehling's solution); false-negative may occur with ferricyanide test. Glucose oxidase or hexokinase-based methods should be used.
Adverse Reactions
>10%: Gastrointestinal: Diarrhea (4% to 11%, duration dependent)
1% to 10%:
Cardiovascular: Local thrombophlebitis (2%)
Dermatologic: Diaper rash (children 3%)
Endocrine & metabolic: Increased lactate dehydrogenase (1%)
Gastrointestinal: Nausea and vomiting (3% to 7%), unpleasant taste (children 5%)
Genitourinary: Vaginitis (≤5%)
Hematologic & oncologic: Decreased hematocrit (≤10%), decreased hemoglobin (≤10%), eosinophilia (1% to 7%)
Hepatic: Increased serum transaminases (2% to 4%), increased serum alkaline phosphatase (2%)
Immunologic: Jarisch-Herxheimer reaction (6%)
<1%, postmarketing, and/or case reports (Limited to important or life-threatening): Abdominal pain, anaphylaxis, angioedema, anorexia, arthralgia, brain disease, candidiasis, chest pain, chest tightness, chills, cholestasis, Clostridioides (formerly Clostridium) difficile-associated diarrhea, colitis, cough, decreased creatinine clearance, dizziness, drowsiness, drug fever, dyspepsia, dyspnea, dysuria, erythema, erythema multiforme, fever, flatulence, gastrointestinal hemorrhage, gastrointestinal infection, glossitis, headache, hearing loss, hemolytic anemia, hepatitis, hyperactivity, hyperbilirubinemia, hypersensitivity, hypersensitivity angiitis, increased blood urea nitrogen, increased liver enzymes, increased serum creatinine, increased thirst, interstitial nephritis, irritability, jaundice, joint swelling, leukopenia, muscle cramps, muscle rigidity, muscle spasm (neck), neutropenia, oral mucosa ulcer, pancytopenia, positive direct Coombs test, prolonged prothrombin time, pruritus, pseudomembranous colitis, renal insufficiency, renal pain, seizure, serum sickness-like reaction, sialorrhea, sinusitis, skin rash, Stevens-Johnson syndrome, stomach cramps, tachycardia, thrombocytopenia (rare), toxic epidermal necrolysis, trismus, upper respiratory tract infection, urethral bleeding, urethral pain, urinary tract infection, urticaria, vaginal discharge, vaginal irritation, viral infection, vulvovaginal candidiasis, vulvovaginal pruritus
Warnings/Precautions
Concerns related to adverse effects:
- Elevated INR: May be associated with increased INR, especially in nutritionally-deficient patients, prolonged treatment, hepatic or renal disease.
- Hypersensitivity reactions: Serious and occasionally severe or fatal hypersensitivity (anaphylactic) reactions have been reported in patients receiving beta-lactam drugs. Before initiating therapy, carefully investigate previous penicillin, cephalosporin, or other allergen hypersensitivity. Use caution if given to a patient with a penicillin or other beta-lactam allergy because cross sensitivity among beta-lactam antibacterial drugs has been established. If an allergic reaction occurs, discontinue and institute appropriate therapy.
- Superinfection: Prolonged use may result in fungal or bacterial superinfection, including C. difficile-associated diarrhea (CDAD) and pseudomembranous colitis; CDAD has been observed >2 months postantibiotic treatment.
Disease-related concerns:
- Gastrointestinal disease: Use with caution in patients with a history of colitis.
- Renal impairment: Use with caution in patients with renal impairment; modify dosage in severe impairment.
- Seizure disorders: Use with caution in patients with a history of seizure disorder; cephalosporins have been associated with seizure activity, particularly in patients with renal impairment not receiving dose adjustments. Discontinue if seizures occur.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Dosage form specific issues:
- Benzyl alcohol and derivatives: Some dosage forms may contain sodium benzoate/benzoic acid; benzoic acid (benzoate) is a metabolite of benzyl alcohol; large amounts of benzyl alcohol (≥99 mg/kg/day) have been associated with a potentially fatal toxicity (“gasping syndrome”) in neonates; the “gasping syndrome” consists of metabolic acidosis, respiratory distress, gasping respirations, CNS dysfunction (including convulsions, intracranial hemorrhage), hypotension, and cardiovascular collapse (AAP ["Inactive" 1997]; CDC 1982); some data suggests that benzoate displaces bilirubin from protein binding sites (Ahlfors 2001); avoid or use dosage forms containing benzyl alcohol derivative with caution in neonates. See manufacturer's labeling.
- Phenylalanine: Some products may contain phenylalanine.
- Suspension/tablet bioequivalence: Tablets and oral suspension are not bioequivalent; do not substitute on a mg-per-mg basis.
- Tablets: Should not be crushed or chewed due to a strong, persistent bitter taste. Patients unable to swallow whole tablets should be prescribed the oral suspension.
Monitoring Parameters
Monitor renal, hepatic, and hematologic function periodically with prolonged therapy. Monitor prothrombin time in patients at risk of prolongation during cephalosporin therapy (nutritionally-deficient, prolonged treatment, renal or hepatic disease). Observe for signs and symptoms of anaphylaxis during first dose.
Pregnancy
Pregnancy Considerations
Cefuroxime crosses the placenta (Dallmann 2017; Lalic-Popovic 2016).
An increased risk of major birth defects or other adverse fetal or maternal outcomes has generally not been observed following maternal use of cephalosporin antibiotics, including cefuroxime.
Due to pregnancy-induced physiologic changes, some pharmacokinetic properties of cefuroxime may be altered (Dallmann 2017; Lalic-Popovic 2016).
Cefuroxime is one of the antibiotics effective for prophylactic use prior to cesarean delivery (ACOG 199 2018).
Patient Education
What is this drug used for?
- It is used to treat or prevent bacterial infections.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Bad taste
- Injection site irritation
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Bruising
- Bleeding
- Unable to pass urine
- Change in amount of urine passed
- Severe loss of strength and energy
- Seizure
- Vaginal pain, itching, and discharge
- Hearing loss
- Clostridium difficile (C. diff)-associated diarrhea like abdominal pain or cramps, severe diarrhea or watery stools, or bloody stools.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.