Boxed Warning
Abuse potential:
CNS stimulants, including amphetamine-containing products and methylphenidate, have a high potential for abuse and dependence. Assess the risk of abuse prior to prescribing and monitor for signs of abuse and dependence while on therapy.
Cardiovascular events (Adderall):
Misuse of amphetamines may cause sudden death and serious cardiovascular adverse events.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Capsule, extended release, oral:
Adderall XR:
5 mg [dextroamphetamine sulfate 1.25 mg, dextroamphetamine saccharate 1.25 mg, amphetamine aspartate monohydrate 1.25 mg, amphetamine sulfate 1.25 mg (equivalent to amphetamine base 3.1 mg)]
10 mg [dextroamphetamine sulfate 2.5 mg, dextroamphetamine saccharate 2.5 mg, amphetamine aspartate monohydrate 2.5 mg, amphetamine sulfate 2.5 mg (equivalent to amphetamine base 6.3 mg)]
15 mg [dextroamphetamine sulfate 3.75 mg, dextroamphetamine saccharate 3.75 mg, amphetamine aspartate monohydrate 3.75 mg, amphetamine sulfate 3.75 mg (equivalent to amphetamine base 9.4 mg)]
20 mg [dextroamphetamine sulfate 5 mg, dextroamphetamine saccharate 5 mg, amphetamine aspartate monohydrate 5 mg, amphetamine sulfate 5 mg (equivalent to amphetamine base 12.5 mg)]
25 mg [dextroamphetamine sulfate 6.25 mg, dextroamphetamine saccharate 6.25 mg, amphetamine aspartate monohydrate 6.25 mg, amphetamine sulfate 6.25 mg (equivalent to amphetamine base 15.6 mg)]
30 mg [dextroamphetamine sulfate 7.5 mg, dextroamphetamine saccharate 7.5 mg, amphetamine aspartate monohydrate 7.5 mg, amphetamine sulfate 7.5 mg (equivalent to amphetamine base 18.8 mg)]
Mydayis:
12.5 mg [dextroamphetamine sulfate 3.125 mg, dextroamphetamine saccharate 3.125 mg, amphetamine aspartate monohydrate 3.125 mg, amphetamine sulfate 3.125 mg (equivalent to amphetamine base 7.8 mg)]
25 mg [dextroamphetamine sulfate 6.25 mg, dextroamphetamine saccharate 6.25 mg, amphetamine aspartate monohydrate 6.25 mg, amphetamine sulfate 6.25 mg (equivalent to amphetamine base 15.6 mg)]
37.5 mg [dextroamphetamine sulfate 9.375 mg, dextroamphetamine saccharate 9.375 mg, amphetamine aspartate monohydrate 9.375 mg, amphetamine sulfate 9.375 mg (equivalent to amphetamine base 23.5 mg)]
50 mg [dextroamphetamine sulfate 12.5 mg, dextroamphetamine saccharate 12.5 mg, amphetamine aspartate monohydrate 12.5 mg, amphetamine sulfate 12.5 mg (equivalent to amphetamine base 31.3 mg)]
Generic:
5 mg [dextroamphetamine sulfate 1.25 mg, dextroamphetamine saccharate 1.25 mg, amphetamine aspartate monohydrate 1.25 mg, amphetamine sulfate 1.25 mg (equivalent to amphetamine base 3.1 mg)]
10 mg [dextroamphetamine sulfate 2.5 mg, dextroamphetamine saccharate 2.5 mg, amphetamine aspartate monohydrate 2.5 mg, amphetamine sulfate 2.5 mg (equivalent to amphetamine base 6.3 mg)]
15 mg [dextroamphetamine sulfate 3.75 mg, dextroamphetamine saccharate 3.75 mg, amphetamine aspartate monohydrate 3.75 mg, amphetamine sulfate 3.75 mg (equivalent to amphetamine base 9.4 mg)]
20 mg [dextroamphetamine sulfate 5 mg, dextroamphetamine saccharate 5 mg, amphetamine aspartate monohydrate 5 mg, amphetamine sulfate 5 mg (equivalent to amphetamine base 12.5 mg)]
25 mg [dextroamphetamine sulfate 6.25 mg, dextroamphetamine saccharate 6.25 mg, amphetamine aspartate monohydrate 6.25 mg, amphetamine sulfate 6.25 mg (equivalent to amphetamine base 15.6 mg)]
30 mg [dextroamphetamine sulfate 7.5 mg, dextroamphetamine saccharate 7.5 mg, amphetamine aspartate monohydrate 7.5 mg, amphetamine sulfate 7.5 mg (equivalent to amphetamine base 18.8 mg)]
Tablet, oral:
Adderall:
5 mg [dextroamphetamine sulfate 1.25 mg, dextroamphetamine saccharate 1.25 mg, amphetamine aspartate monohydrate 1.25 mg, amphetamine sulfate 1.25 mg (equivalent to amphetamine base 3.13 mg)]
7.5 mg [dextroamphetamine sulfate 1.875 mg, dextroamphetamine saccharate 1.875 mg, amphetamine aspartate monohydrate 1.875 mg, amphetamine sulfate 1.875 mg (equivalent to amphetamine base 4.7 mg)]
10 mg [dextroamphetamine sulfate 2.5 mg, dextroamphetamine saccharate 2.5 mg, amphetamine aspartate monohydrate 2.5 mg, amphetamine sulfate 2.5 mg (equivalent to amphetamine base 6.3 mg)]
12.5 mg [dextroamphetamine sulfate 3.125 mg, dextroamphetamine saccharate 3.125 mg, amphetamine aspartate monohydrate 3.125 mg, amphetamine sulfate 3.125 mg (equivalent to amphetamine base 7.8 mg)]
15 mg [dextroamphetamine sulfate 3.75 mg, dextroamphetamine saccharate 3.75 mg, amphetamine aspartate monohydrate 3.75 mg, amphetamine sulfate 3.75 mg (equivalent to amphetamine base 9.4 mg)]
20 mg [dextroamphetamine sulfate 5 mg, dextroamphetamine saccharate 5 mg, amphetamine aspartate monohydrate 5 mg, amphetamine sulfate 5 mg (equivalent to amphetamine base 12.6 mg)]
30 mg [dextroamphetamine sulfate 7.5 mg, dextroamphetamine saccharate 7.5 mg, amphetamine aspartate monohydrate 7.5 mg, amphetamine sulfate 7.5 mg (equivalent to amphetamine base 18.8 mg)]
Generic:
5 mg [dextroamphetamine sulfate 1.25 mg, dextroamphetamine saccharate 1.25 mg, amphetamine aspartate monohydrate 1.25 mg, amphetamine sulfate 1.25 mg (equivalent to amphetamine base 3.13 mg)]
7.5 mg [dextroamphetamine sulfate 1.875 mg, dextroamphetamine saccharate 1.875 mg, amphetamine aspartate monohydrate 1.875 mg, amphetamine sulfate 1.875 mg (equivalent to amphetamine base 4.7 mg)]
10 mg [dextroamphetamine sulfate 2.5 mg, dextroamphetamine saccharate 2.5 mg, amphetamine aspartate monohydrate 2.5 mg, amphetamine sulfate 2.5 mg (equivalent to amphetamine base 6.3 mg)]
12.5 mg [dextroamphetamine sulfate 3.125 mg, dextroamphetamine saccharate 3.125 mg, amphetamine aspartate monohydrate 3.125 mg, amphetamine sulfate 3.125 mg (equivalent to amphetamine base 7.8 mg)]
15 mg [dextroamphetamine sulfate 3.75 mg, dextroamphetamine saccharate 3.75 mg, amphetamine aspartate monohydrate 3.75 mg, amphetamine sulfate 3.75 mg (equivalent to amphetamine base 9.4 mg)]
20 mg [dextroamphetamine sulfate 5 mg, dextroamphetamine saccharate 5 mg, amphetamine aspartate monohydrate 5 mg, amphetamine sulfate 5 mg (equivalent to amphetamine base 12.6 mg)]
30 mg [dextroamphetamine sulfate 7.5 mg, dextroamphetamine saccharate 7.5 mg, amphetamine aspartate monohydrate 7.5 mg, amphetamine sulfate 7.5 mg (equivalent to amphetamine base 18.8 mg)]
Pharmacology
Mechanism of Action
Amphetamines are noncatecholamine, sympathomimetic amines that promote release of catecholamines (primarily dopamine and norepinephrine) from their storage sites in the presynaptic nerve terminals. A less significant mechanism may include their ability to block the reuptake of catecholamines by competitive inhibition.
Pharmacokinetics/Pharmacodynamics
Absorption
Extended release: Food does not affect absorption but prolongs Tmax of Adderall XR by 2 to 3 hours and Mydayis by 4 to 5 hours.
Metabolism
Hepatic oxidation via cytochrome P450 to 4-hydroxyamphetamine (active) norephedrine (active), and alpha-hydroxy-amphetamine with both active metabolites subsequently oxidized to 4-hydroxy-norephedrine. Cytochrome P450 2D6 is primarily responsible for the formation of 4-hydroxy-amphetamine.
Excretion
Urine (highly dependent on urinary pH); excreted as unchanged amphetamine (30% to 40%, may range from ~1% in alkaline urine to ~75% in acidic urine), and derivatives of alpha-hydroxyamphetamine (50%)
Time to Peak
Immediate release: 3 hours; Adderall XR: 7 hours; Mydayis: 7 to 10 hours (children and adolescents 6 to 17 years), 8 hours (adults)
Duration of Action
Immediate-release tablet: 4 to 6 hours (Dopheide 2009); Adderall XR: 8 to 12 hours (Jain 2017); Mydayis: ≤16 hours
Half-Life Elimination
Children 6 to 12 years: d-amphetamine: 9 hours; l-amphetamine: 11 hours
Adolescents 13 to 17 years: d-amphetamine: 11 hours; l-amphetamine: 13 to 14 hours
Adults: d-amphetamine: 10 hours; l-amphetamine: 13 hours
Use in Specific Populations
Special Populations: Children
Children eliminated amphetamine faster than adults. The elimination half-life is approximately 1 hour shorter for d-amphetamine and 2 hours shorter for l-amphetamine in children than in adults. However, children had higher systemic exposure to amphetamine (Cmax and AUC) than adults for a given dose of ER capsules, which was attributed to the higher dose administered to children on a mg/kg basis compared with adults. Upon dose normalization on a mg/kg basis, children showed 30% less systemic exposure compared with adults. Patients 6 to 12 years of age experienced higher systemic exposure (72% to 79% higher Cmax and 83% higher AUC), compared with adults.
Special Populations Note
Weight: Weight is the primary determinant of apparent differences in the pharmacokinetics of d- and l-amphetamine across the age range. Systemic exposure measured by AUC∞ and Cmax decreased with increases in body weight, while apparent oral volume of distribution, apparent oral clearance, and elimination half-life increased with increases in body weight.
Use: Labeled Indications
Attention-deficit/hyperactivity disorder: Treatment of attention-deficit/hyperactivity disorder (ADHD) as part of a total treatment program that typically includes other remedial measures (psychological, educational, social) for a stabilizing effect.
Narcolepsy, daytime sleepiness (immediate release only): Treatment of narcolepsy.
Contraindications
Hypersensitivity (eg, angioedema, anaphylaxis) or idiosyncrasy to amphetamine, sympathomimetic amines or any component of the formulation; during or within 14 days following MAOI (including linezolid or methylene blue).
Documentation of allergenic cross-reactivity for amphetamines is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Immediate release, Adderall XR: Additional contraindications: Advanced arteriosclerosis; symptomatic cardiovascular disease, moderate to severe hypertension, hyperthyroidism; glaucoma, agitated states; history of drug abuse.
Dosage and Administration
Dosing: Adult
Attention-deficit/hyperactivity disorder:
Immediate release: Oral: Initial: 5 mg once or twice daily; may increase daily dose based on response and tolerability in increments of 5 to 10 mg every week up to a usual maximum of 40 mg/day in 2 to 3 divided doses (Bukstein 2019; Spencer 2001). Some experts recommend waiting up to 1 month before increasing dose (Bukstein 2019). Note: Although doses >40 mg/day will rarely be necessary, doses as high as 60 mg/day may be necessary for optimal response in some patients and have been shown to be safe (Spencer 2001).
Extended release: Oral: Initial: 10 to 20 mg once daily in the morning; may increase daily dose based on response and tolerability in increments of 10 to 20 mg every week (Bukstein 2019; Weisler 2006). Some experts recommend waiting up to 1 month before increasing dose (Bukstein 2019). Although doses >40 mg/day will rarely be necessary, doses up to 60 mg/day may be necessary for optimal response in some patients, but the frequency and severity of adverse effects are increased with higher doses (Biederman 2005; Bukstein 2019).
Triple-bead extended release: Oral: Initial: 12.5 mg once daily in the morning; may increase daily dose based on response and tolerability in increments of 12.5 mg every week (Spencer 2008; Wigal 2018; manufacturer's labeling). Some experts recommend waiting up to 1 month before increasing dose (Bukstein 2019). Maximum dose: 50 mg/day.
Narcolepsy, daytime sleepiness (alternative agent): Oral: Initial: 10 mg once daily in the morning; may increase daily dose based on response and tolerability in increments of 10 mg every week until optimal response is obtained; usual dosage range: 20 to 60 mg/day in 1 to 3 divided doses (Thorpy 2015). Some experts recommend initiating therapy with the IR formulation (FDA approved) and transitioning to extended release (off label) once the patient achieves a stable dose. Although the ER formulation is generally dosed once daily, some patients may require a second dose in the early afternoon (Scammell 2019).
Dosing: Geriatric
Refer to adult dosing; use with caution and start at low end of dosage range.
Dosing: Pediatric
Note: Use lowest effective individualized dose; administer first dose as soon as awake; avoid late evening doses
Attention-deficit/hyperactivity disorder: Note: Extended-release products are not interchangeable on a mg-per-mg basis; use precaution to ensure appropriate product specific dosing.
Immediate-release tablets:
Children 3 to 5 years: Oral: Initial 2.5 mg once daily in the morning; increase daily dose by 2.5 mg at weekly intervals until optimal response is obtained; maximum daily dose: 40 mg/day administered in 1 to 2 divided doses per day; use intervals of 4 to 6 hours between doses. Note: Select patients may require daily dose to be given in 3 divided doses per day. Although FDA approved, current guidelines do not recommend dextroamphetamine/amphetamine use in children ≤5 years due to insufficient evidence (AAP 2011).
Children ≥6 years and Adolescents: Oral: Initial: 5 mg once or twice daily; increase daily dose by 5 mg at weekly intervals until optimal response is obtained; usual maximum daily dose: 40 mg/day administered in 1 to 2 divided doses; use intervals of 4 to 6 hours between doses; some patients weighing >50 kg may require and tolerate doses up to 60 mg/day in divided doses with frequent monitoring (AACAP [Pliszka 2007]; Dopheide 2009). Note: Some patients may require daily dose to be administered as 3 divided doses per day.
Extended-release capsules:
Adderall XR:
Initial therapy:
Children 6 to 12 years: Oral: Initial: 5 to 10 mg once daily in the morning; increase daily dose by 5 mg or 10 mg at weekly intervals until optimal response is obtained; usual maximum daily dose: 30 mg/day; some patients weighing >50 kg may require and tolerate doses up to 60 mg/day (AACAP [Pliszka 2007]; Dopheide 2009)
Adolescents 13 to 17 years: Oral: Initial: 10 mg once daily in the morning; may increase to 20 mg daily after 1 week if symptoms are not controlled; usual maximum daily dose: 20 mg/day; some patients weighing >50 kg may require and tolerate doses up to 60 mg/day with frequent monitoring (AACAP [Pliszka 2007]; Dopheide 2009)
Converting Adderall to Adderall XR:Patients taking divided doses of immediate-release Adderall tablets may be switched to extended-release Adderall XR capsule using the same total daily dose (taken once daily); titrate dose at weekly intervals to achieve optimal response.
Mydayis: Note: Do not substitute Mydayis for other amphetamine products on a mg-per-mg basis because of different amphetamine base compositions and differing pharmacokinetic profiles.
Adolescents 13 to 17 years: Oral: Initial: 12.5 mg once daily in the morning; may increase by 12.5 mg increments at weekly intervals; maximum daily dose: 25 mg/day
Narcolepsy:
Children 6 to 12 years: Immediate-release tablets: Oral: Initial: 5 mg daily; increase daily dose by 5 mg at weekly intervals until optimal response is obtained; maximum daily dose: 60 mg/day given in 1 to 3 divided doses per day; use intervals of 4 to 6 hours between doses
Adolescents: Immediate-release tablets: Oral: Initial: 10 mg daily; increase daily dose by 10 mg at weekly intervals until optimal response is obtained; maximum daily dose: 60 mg/day given in 1 to 3 divided doses per day; use intervals of 4 to 6 hours between doses
Extemporaneously Prepared
A 1 mg/mL oral suspension may be made with tablets. Crush ten 10 mg tablets in a mortar and reduce to a fine powder. Add small portions of Ora-Sweet and mix to a uniform paste; mix while adding the vehicle in equal proportions to almost 100 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add sufficient quantity of vehicle to make 100 mL. Label "shake well". Stable 30 days at room temperature.
Administration
Administer with or without food. Administer Mydayis consistently either with food or without food.
Immediate release: Administer in 1 to 3 divided doses per day with intervals of 4 to 6 hours between doses. To avoid insomnia, late evening doses should be avoided.
Extended release: To avoid insomnia, afternoon doses should be avoided. Capsule may be swallowed whole or it may be opened and the contents sprinkled on applesauce. Applesauce should be consumed immediately without chewing. Do not divide the contents of the capsule. Do not take less than one capsule per day; a single capsule should not be divided.
Storage
Immediate-release tablets: Store at 20°C to 25°C (68°F to 77°F); protect from light.
Extended-release capsules: Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F); protect from light.
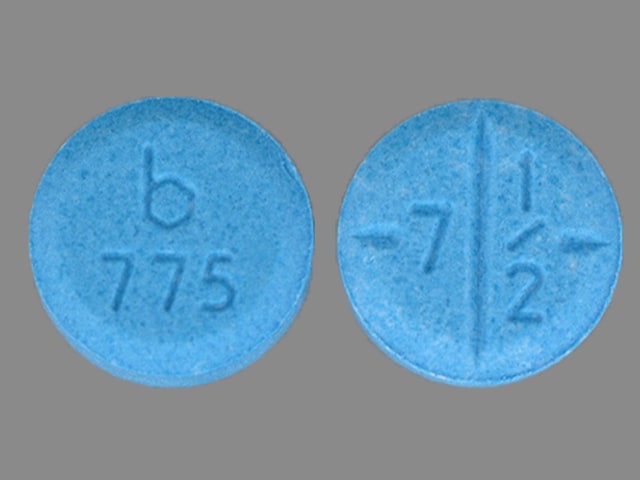
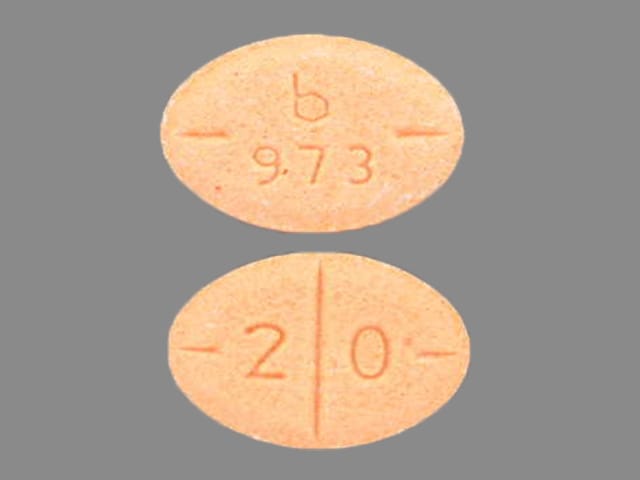
Dextroamphetamine and Amphetamine Images
Drug Interactions
Acebrophylline: May enhance the stimulatory effect of CNS Stimulants. Avoid combination
Alkalinizing Agents: May decrease the excretion of Amphetamines. Management: Consider alternatives to using amphetamines and alkalinizing agents in combination. If these agents must be used together, patients should be monitored closely for excessive amphetamine effects. Consider therapy modification
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Ammonium Chloride: May decrease the serum concentration of Amphetamines. This effect is likely due to an enhanced excretion of amphetamines in the urine. Monitor therapy
Antacids: May decrease the excretion of Amphetamines. Monitor therapy
Antihistamines: Amphetamines may diminish the sedative effect of Antihistamines. Monitor therapy
Antihypertensive Agents: Amphetamines may diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Antipsychotic Agents: May diminish the stimulatory effect of Amphetamines. Monitor therapy
Ascorbic Acid: May decrease the serum concentration of Amphetamines. Monitor therapy
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
BuPROPion: May enhance the neuroexcitatory and/or seizure-potentiating effect of Agents With Seizure Threshold Lowering Potential. Monitor therapy
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
Carbonic Anhydrase Inhibitors: May decrease the excretion of Amphetamines. Exceptions: Brinzolamide; Dorzolamide. Monitor therapy
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
CYP2D6 Inhibitors (Moderate): May increase the serum concentration of Amphetamines. Monitor therapy
CYP2D6 Inhibitors (Strong): May increase the serum concentration of Amphetamines. Exceptions: FLUoxetine; PARoxetine. Monitor therapy
Doxofylline: Sympathomimetics may enhance the adverse/toxic effect of Doxofylline. Monitor therapy
Esketamine: May enhance the hypertensive effect of CNS Stimulants. Monitor therapy
Ethosuximide: Amphetamines may diminish the therapeutic effect of Ethosuximide. Amphetamines may decrease the serum concentration of Ethosuximide. Monitor therapy
Gastrointestinal Acidifying Agents: May decrease the serum concentration of Amphetamines. Monitor therapy
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Iobenguane Radiopharmaceutical Products: Amphetamines may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Iobenguane Radiopharmaceutical Products: CNS Stimulants may diminish the therapeutic effect of Iobenguane Radiopharmaceutical Products. Management: Discontinue all drugs that may inhibit or interfere with catecholamine transport or uptake for at least 5 biological half-lives before iobenguane administration. Do not administer these drugs until at least 7 days after each iobenguane dose. Avoid combination
Ioflupane I 123: Amphetamines may diminish the diagnostic effect of Ioflupane I 123. Monitor therapy
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Methenamine: May decrease the serum concentration of Amphetamines. This effect is likely due to an enhanced excretion of amphetamines in the urine. Monitor therapy
Monoamine Oxidase Inhibitors: May enhance the hypertensive effect of Amphetamines. While linezolid and tedizolid may interact via this mechanism, management recommendations differ from other monoamine oxidase inhibitors. Refer to monographs specific to those agents for details. Avoid combination
Multivitamins/Fluoride (with ADE): May decrease the serum concentration of Amphetamines. More specifically, the ascorbic acid (vitamin C) in many multivitamins may decrease amphetamine concentrations. Monitor therapy
Multivitamins/Minerals (with ADEK, Folate, Iron): May decrease the serum concentration of Amphetamines. Monitor therapy
Multivitamins/Minerals (with AE, No Iron): May decrease the serum concentration of Amphetamines. Specifically, vitamin C may impair absorption of amphetamines. Monitor therapy
Opioid Agonists: Amphetamines may enhance the analgesic effect of Opioid Agonists. Monitor therapy
PHENobarbital: Amphetamines may decrease the serum concentration of PHENobarbital. Monitor therapy
Phenytoin: Amphetamines may decrease the serum concentration of Phenytoin. Monitor therapy
Proton Pump Inhibitors: May increase the absorption of Amphetamine. Monitor therapy
Proton Pump Inhibitors: May increase the absorption of Dextroamphetamine. Specifically, the dextroamphetamine absorption rate from mixed amphetamine salt extended release (XR) capsules may be increased in the first hours after dosing. Monitor therapy
Quinolones: Amphetamines may enhance the cardiotoxic effect of Quinolones. Monitor therapy
Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors): Amphetamines may enhance the serotonergic effect of Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors). This could result in serotonin syndrome. Selective Serotonin Reuptake Inhibitors (Strong CYP2D6 Inhibitors) may increase the serum concentration of Amphetamines. Management: Monitor for increased amphetamine toxicities, including signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability) when these agents are combined. Monitor therapy
Serotonergic Agents (High Risk): Amphetamines may enhance the serotonergic effect of Serotonergic Agents (High Risk). This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) when these agents are combined. Exceptions: Amitriptyline; Amoxapine; ClomiPRAMINE; Desipramine; Dothiepin; Doxepin (Systemic); Doxepin (Topical); FLUoxetine; Imipramine; Isocarboxazid; Linezolid; Lofepramine; Melitracen [INT]; Methylene Blue; Moclobemide; Nortriptyline; PARoxetine; Phenelzine; Protriptyline; Tranylcypromine; Trimipramine. Monitor therapy
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Solriamfetol: CNS Stimulants may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Tricyclic Antidepressants: May enhance the adverse/toxic effect of Amphetamines. Tricyclic Antidepressants may potentiate the cardiovascular effects of Amphetamines. Amphetamines may enhance the serotonergic effect of Tricyclic Antidepressants. This could result in serotonin syndrome. Management: Monitor for signs and symptoms of serotonin syndrome/serotonin toxicity (eg, hyperreflexia, clonus, hyperthermia, diaphoresis, tremor, autonomic instability, mental status changes) and increased cardiovascular effects when these agents are combined. Monitor therapy
Urinary Acidifying Agents: May decrease the serum concentration of Amphetamines. Monitor therapy
Test Interactions
May cause a significant elevation in plasma corticosteroid levels; may interfere with urinary steroid testing
Adverse Reactions
Frequency not always defined.
Cardiovascular: Systolic hypertension (extended release; adolescents: 12% to 35%; dose related; transient), tachycardia (extended release; adults: ≤6%), palpitations (extended release: 2% to 4%), increased blood pressure, myocardial infarction, Raynaud's phenomenon
Central nervous system: Insomnia (extended release: 8% to 31%), headache (extended release; adults: ≤26%), emotional lability (extended release: 2% to 9%), anxiety (extended release; adults: 7% to 8%), agitation (extended release; adults: 2% to ≤8%), dizziness (extended release: 2% to 7%), irritability (6%), fatigue (extended release: 2% to 6%), drowsiness (extended release: 2% to 4%), speech disturbance (extended release: 2% to 4%), twitching (extended release: 2% to 4%), depression (3%), jitteriness (2%), aggressive behavior, dysphoria, euphoria, exacerbation of vocal tics, formication, outbursts of anger, overstimulation, paresthesia, psychosis, restlessness, talkativeness
Dermatologic: Diaphoresis (extended release: 2% to 4%), skin photosensitivity (extended release: 2% to 4%), alopecia, dermatillomania, skin rash, urticaria
Endocrine & metabolic: Weight loss (extended release: 4% to 10%), decreased libido (extended release: 2% to 4%), dysmenorrhea (extended release: 2% to 4%)
Gastrointestinal: Decreased appetite (extended release: 22% to 36%), xerostomia (extended release: 2% to 35%), abdominal pain (extended release: 11% to 14%), nausea (extended release: 2% to 8%), vomiting (extended release: 2% to 7%), diarrhea (extended release: 2% to 6%), constipation (extended release: 2% to 4%), dyspepsia (extended release: 2% to 4%), teeth clenching (extended release: ≤4%), tooth infection (extended release: ≤4%), anorexia (extended release: 2%), bruxism (2%), unpleasant taste
Genitourinary: Urinary tract infection (extended release: 5%), upper abdominal pain (adolescents: 4%), impotence (extended release: 2% to 4%), erectile dysfunction (2%), frequent erections, prolonged erections
Hypersensitivity: Anaphylaxis, angioedema, hypersensitivity reaction
Infection: Infection (extended release: 2% to 4%)
Neuromuscular & skeletal: Dyskinesia, rhabdomyolysis, tremor
Ophthalmic: Blurred vision, mydriasis
Respiratory: Dyspnea (extended release: 2% to 4%)
Miscellaneous: Fever (extended release: 5%), accidental injury (children and adolescents: 4%)
<1%, postmarketing, and/or case reports: Cardiomyopathy, cerebrovascular accident, exacerbation of Gilles de la Tourette's syndrome, exacerbation of vocal tics, peripheral vascular disease, seizure, Stevens-Johnson syndrome, toxic epidermal necrolysis
Warnings/Precautions
Concerns related to adverse effects:
- Cardiovascular events: Use has been associated with serious cardiovascular events including sudden death in patients with preexisting structural cardiac abnormalities or other serious heart problems (sudden death in children and adolescents; sudden death, stroke, and MI in adults). Consistent with other studies, a large retrospective cohort study involving 1,200,438 children, adolescents, and young adults (aged 2 to 24 years) prescribed methylphenidate, dexmethylphenidate, dextroamphetamines, amphetamine salts, pemoline, or atomoxetine found no evidence that current use of an ADHD medication increased risk for sudden cardiac death, acute MI, or stroke (Cooper 2011). Stimulants should be avoided in patients with known structural cardiac abnormalities, cardiomyopathy, serious heart rhythm abnormalities, coronary artery disease, Marfan syndrome, or other serious cardiac problems. Some products are contraindicated in patients with moderate or severe hypertension. Prior to initiating stimulant, assess medical history and family history of sudden death or ventricular arrhythmia; conduct a physical exam to assess for cardiac disease; patients should receive further evaluation if findings suggest cardiac disease, such as ECG and echocardiogram. Promptly conduct cardiac evaluation in patients who develop exertional chest pain, unexplained syncope, or any other symptoms of cardiac disease during stimulant treatment.
- CNS effects: Amphetamines may impair the ability to engage in potentially hazardous activities; patients must be cautioned about performing tasks that require mental alertness (eg, operating machinery, driving).
- Hypersensitivity: Hypersensitivity reactions, including anaphylaxis, Stevens-Johnson syndrome, toxic epidermal necrolysis, angioedema, and urticaria, have been observed.
- Peripheral vasculopathy: Stimulants are associated with peripheral vasculopathy, including Raynaud phenomenon; signs/symptoms are usually mild and intermittent, and generally improve with dose reduction or discontinuation. Peripheral vasculopathy effects have been observed at different times, at therapeutic doses, and in all age groups. Digital ulceration and/or soft tissue breakdown have been observed rarely; monitor for digital changes during therapy and seek further evaluation (eg, rheumatology) if necessary.
- Serotonin syndrome: Potentially life-threatening serotonin syndrome (SS) may occur when dextroamphetamine/amphetamine is used in combination with other serotonergic agents (eg, SSRIs, SNRIs, triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, buspirone, St. John's wort, tryptophan), agents that impair metabolism of serotonin (eg, MAOIs) or CYP2D6 inhibitors that impair metabolism of dextroamphetamine/amphetamine. Concomitant use with MAOIs is contraindicated. If concomitant use of dextroamphetamine/amphetamine with serotonergic drugs or CYP2D6 inhibitors is indicated, initiate dextroamphetamine/amphetamine at a low dose and monitor patient closely for signs and symptoms of SS. Discontinue treatment (and any concomitant serotonergic agent) immediately if signs/symptoms arise.
- Visual disturbance: Difficulty in accommodation and blurred vision has been reported with the use of stimulants.
Disease-related concerns:
- Cardiovascular disorders: CNS stimulants may increase heart rate and blood pressure; in pediatric patients, the observed mean increase in heart rate was 3 to 6 bpm and blood pressure was 2 to 4 mm Hg. Use with caution in patients with hypertension, heart failure, recent MI, ventricular arrhythmia, and other cardiovascular conditions that might be exacerbated by increases in blood pressure or heart rate. Some products are contraindicated in patients with moderate to severe hypertension or hyperthyroidism.
- Hepatic impairment: Use with caution in patients with hepatic impairment; elimination is reduced.
- Psychiatric disorders: Use with caution in patients with preexisting psychosis (may exacerbate symptoms of behavior and thought disorder) or bipolar disorder (may induce mixed/manic episode). New-onset psychosis or mania may occur with stimulant use. Patients should be screened for bipolar disorder and risk factors for developing a manic episode prior to treatment; consider discontinuation if psychotic or manic symptoms (eg, delusional thinking, hallucinations, mania) occur. May be associated with aggressive behavior or hostility (causal relationship not established); monitor for development or worsening of these behaviors.
- Renal impairment: Use with caution in patients with renal impairment; elimination is reduced.
- Seizure disorder: Limited information exists regarding stimulant use in seizure disorder. Whereas patients with attention-deficit/hyperactivity disorder (ADHD) are at an increased risk for seizure activity compared to the general population, a retrospective study using drug claims data showed that the use of stimulant medications was associated with a lower risk (Cortese 2013; Wiggs 2018). Manufacturers of some stimulants recommend discontinuing therapy if seizures occur.
- Tourette syndrome/tics: Use with caution in patients with Tourette syndrome or other tic disorders. Stimulants may exacerbate tics (motor and phonic) and Tourette syndrome; however, evidence demonstrating increased tics is limited. Evaluate for tics and Tourette syndrome prior to therapy initiation (AACAP [Murphy 2013; Pliszka 2007]).
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use caution in this age group due to CNS stimulant adverse effects.
- Pediatric: Appetite suppression may occur; particularly in children. Use of stimulants has been associated with weight loss and slowing growth rate; monitor growth rate and weight during treatment. Treatment interruption may be necessary in patients who are not increasing in height or gaining weight as expected. Pediatric patients 12 years and younger experienced high plasma exposure to Mydayis and more adverse reactions, including insomnia and decreased appetite, compared to patients 13 years and older.
Other warnings/precautions:
- Abuse/misuse/diversion: [US Boxed Warning]: Has high potential for abuse and dependence. Assess the risk of abuse prior to prescribing and monitor for signs of abuse and dependence while on therapy. Use with caution in patients with history of ethanol or drug abuse. Prescriptions should be written for the smallest quantity consistent with good patient care to minimize possibility of overdose.
- ADHD treatment: Appropriate use: Recommended to be used as part of a comprehensive treatment program for attention-deficit disorders.
- Appropriate use: Mydayis: Medication errors, including substitution and dispensing errors, may occur, leading to possible overdosage. Do not substitute Mydayis for other amphetamine products on a mg-per-mg basis because of different amphetamine base compositions and differing pharmacokinetic profiles.
- Discontinuation of therapy: Abrupt discontinuation following high doses for prolonged periods results in extreme fatigue, mental depression, and sleep EEG changes; may also result in other symptoms of withdrawal.
Monitoring Parameters
Cardiac evaluation should be completed at baseline and on any patient who develops exertional chest pain, unexplained syncope, and any symptom of cardiac disease during treatment with stimulants. Monitor blood pressure and heart rate (baseline, following dose increases and periodically during treatment); growth rate (height and weight) and appetite in children; weight in adults; signs of peripheral vasculopathy (eg, digital changes); sleep and behavioral changes. Assess for risk of abuse prior to prescribing and signs of misuse, abuse, or addiction throughout treatment (NICE 2018).
Pregnancy
Pregnancy Considerations
Outcome information related to the use of amphetamine/dextroamphetamine in pregnant women with attention-deficit/hyperactivity disorder is limited (Ornoy 2018).
Data collection to monitor pregnancy outcomes following exposure to amphetamine/dextroamphetamine is ongoing. Health care providers are encouraged to enroll females exposed to amphetamine/dextroamphetamine during pregnancy in the National Pregnancy Registry for Psychostimulants (1-866-961-2388 and/or https://womensmentalhealth.org/clinical-and-research-programs/pregnancyregistry/othermedications).
Refer to individual monographs for additional information.
Patient Education
What is this drug used for?
- It is used to treat attention deficit problems with hyperactivity.
- It is used to treat narcolepsy.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Abdominal pain
- Lack of appetite
- Trouble sleeping
- Constipation
- Diarrhea
- Dry mouth
- Bad taste
- Nausea
- Vomiting
- Loss of strength and energy
- Weight loss
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe cerebrovascular disease like change in strength on one side is greater than the other, difficulty speaking or thinking, change in balance, or vision changes.
- Chest pain
- Shortness of breath
- Severe dizziness
- Passing out
- Fast heartbeat
- Severe anxiety
- Severe headache
- Sexual dysfunction
- Sex drive changes
- Abnormal heartbeat
- Seizures
- Abnormal movements
- Agitation
- Vision changes
- Erection that lasts more than 4 hours
- Change in color of hands or feet from pale to blue or red
- Burning or numbness of hands or feet
- Cold sensation of extremities
- Painful extremities
- Serotonin syndrome like dizziness, severe headache, agitation, sensing things that seem real but are not, fast heartbeat, abnormal heartbeat, flushing, tremors, sweating a lot, change in balance, severe nausea, or severe diarrhea.
- Wounds on fingers or toes
- Dark urine
- Unable to pass urine
- Change in amount of urine passed
- Painful urination
- Muscle pain
- Muscle weakness
- Depression like thoughts of suicide, anxiety, emotional instability, or confusion.
- Mood changes
- Sensing things that seem real but are not
- Behavioral changes
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.