Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral:
Lopid: 600 mg [scored]
Generic: 600 mg
Pharmacology
Mechanism of Action
The exact mechanism of action of gemfibrozil is unknown, however, several theories exist regarding the VLDL effect; it can inhibit lipolysis and decrease subsequent hepatic fatty acid uptake as well as inhibit hepatic secretion of VLDL; together these actions decrease serum VLDL levels; increases HDL-cholesterol; the mechanism behind HDL elevation is currently unknown
Pharmacokinetics/Pharmacodynamics
Absorption
Well absorbed
Metabolism
Hepatic via oxidation to two inactive metabolites; undergoes enterohepatic recycling
Excretion
Urine (~70% primarily as conjugated drug); feces (6%)
Onset of Action
May require several days
Time to Peak
Serum: 1 to 2 hours
Half-Life Elimination
1.5 hours
Protein Binding
99%
Use: Labeled Indications
Treatment of hypertriglyceridemia in Fredrickson types IV and V hyperlipidemia for patients who are at greater risk for pancreatitis and who have not responded to dietary intervention; to reduce the risk of CHD development in Fredrickson type IIb patients without a history or symptoms of existing CHD who have not responded to dietary and other interventions (including pharmacologic treatment) and who have decreased HDL, increased LDL, and increased triglycerides
Contraindications
Hypersensitivity to gemfibrozil or any component of the formulation; hepatic or severe renal dysfunction; primary biliary cirrhosis; preexisting gallbladder disease; concurrent use with dasabuvir, repaglinide, selexipag, or simvastatin.
Canadian labeling: Additional contraindications (not in the US labeling): Renal dysfunction; concurrent use with cerivastatin; pregnancy; breastfeeding.
Documentation of allergenic cross-reactivity for fibrates is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Dosage and Administration
Dosing: Adult
Hyperlipidemia/hypertriglyceridemia: Oral: 600 mg twice daily 30 minutes before breakfast and dinner. Note: Discontinue if lipid response is inadequate after 3 months of therapy.
Dosing: Geriatric
Refer to adult dosing.
Administration
Administer 30 minutes prior to breakfast and dinner.
Dietary Considerations
Before initiation of therapy, patients should be placed on a standard cholesterol-lowering diet for 3 to 6 months and the diet should be continued during drug therapy. Administer 30 minutes prior to breakfast and dinner
Storage
Store at 20°C to 25°C (68°F to 77°F). Protect from light and moisture.
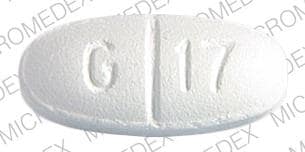
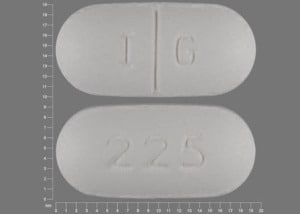
Gemfibrozil Images
Drug Interactions
Acipimox: May enhance the myopathic (rhabdomyolysis) effect of Fibric Acid Derivatives. Monitor therapy
Alitretinoin (Systemic): CYP2C8 Inhibitors (Strong) may increase the serum concentration of Alitretinoin (Systemic). Management: Consider reducing the alitretinoin dose to 10 mg when used together with strong CYP2C8 inhibitors. Monitor for increased alitretinoin effects/toxicities if combined with a strong CYP2C8 inhibitor. Consider therapy modification
Amiodarone: CYP2C8 Inhibitors (Strong) may increase the serum concentration of Amiodarone. Monitor therapy
Amodiaquine: CYP2C8 Inhibitors (Strong) may increase the serum concentration of Amodiaquine. Avoid combination
Apalutamide: CYP2C8 Inhibitors (Strong) may increase the serum concentration of Apalutamide. Monitor therapy
Asunaprevir: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Asunaprevir. Avoid combination
AtorvaSTATin: Gemfibrozil may enhance the myopathic (rhabdomyolysis) effect of AtorvaSTATin. Gemfibrozil may increase the serum concentration of AtorvaSTATin. Avoid combination
Bexarotene (Systemic): Gemfibrozil may increase the serum concentration of Bexarotene (Systemic). Avoid combination
Bile Acid Sequestrants: May decrease the absorption of Fibric Acid Derivatives. Management: Separate doses by at least 2 hours to minimize this interaction; fenofibric acid labeling recommends administration one hour prior to or 4-6 hours after a bile acid sequestrant. Exceptions: Colesevelam. Consider therapy modification
Chenodiol: Fibric Acid Derivatives may diminish the therapeutic effect of Chenodiol. Management: Monitor clinical response to chenodiol closely when used together with any fibric acid derivative. Monitor therapy
Ciprofibrate: May enhance the adverse/toxic effect of Fibric Acid Derivatives. Avoid combination
Colchicine: Fibric Acid Derivatives may enhance the myopathic (rhabdomyolysis) effect of Colchicine. Monitor therapy
CycloSPORINE (Systemic): May enhance the nephrotoxic effect of Fibric Acid Derivatives. Fibric Acid Derivatives may decrease the serum concentration of CycloSPORINE (Systemic). Management: Careful consideration of the risks and benefits should be undertaken prior to use of this combination; extra monitoring of renal function and cyclosporine concentrations will likely be required. Adjustment of cyclosporine dose may be necessary. Consider therapy modification
Dabrafenib: CYP2C8 Inhibitors (Strong) may increase the serum concentration of Dabrafenib. Management: Consider alternatives to strong CYP2C8 inhibitors in patients being treated with dabrafenib. If such a combination cannot be avoided, monitor closely for evidence of dabrafenib-related adverse effects. Consider therapy modification
Dasabuvir: CYP2C8 Inhibitors (Strong) may increase the serum concentration of Dasabuvir. Avoid combination
Desloratadine: CYP2C8 Inhibitors (Strong) may increase the serum concentration of Desloratadine. Monitor therapy
Dichlorphenamide: OAT1/3 Inhibitors may increase the serum concentration of Dichlorphenamide. Monitor therapy
Elagolix: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Elagolix. Avoid combination
Eluxadoline: Gemfibrozil may increase the serum concentration of Eluxadoline. Management: Decrease the eluxadoline dose to 75 mg twice daily if combined with gemfibrozil and monitor patients for increased eluxadoline effects/toxicities. Consider therapy modification
Enzalutamide: CYP2C8 Inhibitors (Strong) may increase the serum concentration of Enzalutamide. Management: Avoid concurrent use of strong CYP2C8 inhibitors and enzalutamide if possible. If the combination must be used, reduce enzalutamide to 80 mg once daily. Consider therapy modification
Ezetimibe: Gemfibrozil may enhance the adverse/toxic effect of Ezetimibe. Specifically, the risk of myopathy and cholelithiasis may be increased. Gemfibrozil may increase the serum concentration of Ezetimibe. Avoid combination
Fluvastatin: Gemfibrozil may enhance the myopathic (rhabdomyolysis) effect of Fluvastatin. Avoid combination
Grazoprevir: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Grazoprevir. Avoid combination
Imatinib: Gemfibrozil may decrease serum concentrations of the active metabolite(s) of Imatinib. Specifically N-desmethylimatinib concentrations may be decreased. Gemfibrozil may decrease the serum concentration of Imatinib. Monitor therapy
Lovastatin: Gemfibrozil may enhance the myopathic (rhabdomyolysis) effect of Lovastatin. Gemfibrozil may increase the serum concentration of Lovastatin. More specifically, gemfibrozil may increase the serum concentrations of lovastatin acid (active form of parent drug). Avoid combination
Montelukast: Gemfibrozil may increase the serum concentration of Montelukast. Monitor therapy
OATP1B1/1B3 (SLCO1B1/1B3) Substrates: Gemfibrozil may increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. See separate drug interaction monographs for agents listed as exceptions. Exceptions: AtorvaSTATin; Eluxadoline; Ezetimibe; Fluvastatin; Pitavastatin; Pravastatin; Repaglinide; Rosuvastatin; Simvastatin. Monitor therapy
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: CYP2C8 Inhibitors (Strong) may increase the serum concentration of Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir. Specifically, the concentrations of the dasabuvir component may be increased. Avoid combination
PACLitaxel (Conventional): CYP2C8 Inhibitors (Strong) may increase the serum concentration of PACLitaxel (Conventional). Monitor therapy
PACLitaxel (Protein Bound): CYP2C8 Inhibitors (Strong) may increase the serum concentration of PACLitaxel (Protein Bound). Monitor therapy
Pioglitazone: CYP2C8 Inhibitors (Strong) may increase the serum concentration of Pioglitazone. Management: Limit the pioglitazone dose to 15 mg daily and monitor for increased pioglitazone toxicities (eg, hypoglycemia) when used in combination with strong CYP2C8 inhibitors. Consider therapy modification
Pitavastatin: Gemfibrozil may enhance the myopathic (rhabdomyolysis) effect of Pitavastatin. Gemfibrozil may increase the serum concentration of Pitavastatin. Avoid combination
Pravastatin: Gemfibrozil may enhance the myopathic (rhabdomyolysis) effect of Pravastatin. Gemfibrozil may increase the serum concentration of Pravastatin. Avoid combination
Raltegravir: May enhance the myopathic (rhabdomyolysis) effect of Fibric Acid Derivatives. Monitor therapy
Repaglinide: CYP2C8 Inhibitors (Strong) may increase the serum concentration of Repaglinide. Avoid combination
Revefenacin: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase serum concentrations of the active metabolite(s) of Revefenacin. Avoid combination
Rosiglitazone: CYP2C8 Inhibitors (Strong) may increase the serum concentration of Rosiglitazone. Monitor therapy
Rosuvastatin: Gemfibrozil may enhance the myopathic (rhabdomyolysis) effect of Rosuvastatin. Gemfibrozil may increase the serum concentration of Rosuvastatin. Management: If possible, avoid concomitant use of rosuvastatin with gemfibrozil. If concomitant can not be avoided, limit rosuvastatin to 10 mg/day (US recommendation) or 20 mg/day (Canadian recommendation). Monitor for signs/symptoms of rhabdomyolysis. Avoid combination
Selexipag: CYP2C8 Inhibitors (Strong) may increase serum concentrations of the active metabolite(s) of Selexipag. CYP2C8 Inhibitors (Strong) may increase the serum concentration of Selexipag. Avoid combination
Simvastatin: Gemfibrozil may enhance the myopathic (rhabdomyolysis) effect of Simvastatin. Gemfibrozil may increase the serum concentration of Simvastatin. Concentrations of the active simvastatin acid metabolite may also be increased by gemfibrozil. Avoid combination
Sulfonylureas: Fibric Acid Derivatives may enhance the hypoglycemic effect of Sulfonylureas. Monitor therapy
Treprostinil: CYP2C8 Inhibitors (Strong) may increase the serum concentration of Treprostinil. Management: Reduce the initial treprostinil extended release tablet dose to 0.125 mg twice daily, titrating by 0.125 mg twice daily every 3 to 4 days. No preemptive dose adjustment is recommended for other treprostinil products. Consider therapy modification
Ursodiol: Fibric Acid Derivatives may diminish the therapeutic effect of Ursodiol. Monitor therapy
Vitamin K Antagonists (eg, warfarin): Fibric Acid Derivatives may enhance the anticoagulant effect of Vitamin K Antagonists. Consider therapy modification
Voxilaprevir: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Voxilaprevir. Avoid combination
Adverse Reactions
>10%: Gastrointestinal: Dyspepsia (20%)
1% to 10%:
Cardiovascular: Atrial fibrillation (1%)
Central nervous system: Fatigue (4%), vertigo (2%)
Dermatologic: Eczema (2%), skin rash (2%)
Gastrointestinal: Abdominal pain (10%), nausea and vomiting (3%)
<1%, postmarketing and/or case reports (probable causation): Anemia, angioedema, arthralgia, blurred vision, bone marrow depression, cholecystitis, cholelithiasis, cholestatic jaundice, decreased libido, depression, dermatitis, dermatomyositis, dizziness, drowsiness, dysgeusia, eosinophilia, exfoliative dermatitis, headache, hypoesthesia, hypokalemia, impotence, increased creatine phosphokinase, increased serum alkaline phosphatase, increased serum bilirubin, increased serum transaminases, laryngeal edema, leukopenia, limb pain, myalgia, myasthenia, myopathy, nephrotoxicity, paresthesia, peripheral neuritis, polymyositis, pruritus, Raynaud phenomenon, rhabdomyolysis, synovitis, urticaria
Reports where causal relationship has not been established: Alopecia, anaphylaxis, cataract, colitis, confusion, extrasystoles, hepatic neoplasm, intracranial hemorrhage, lupus-like syndrome, pancreatitis, peripheral vascular disease, positive ANA titer, reduced fertility (male), renal insufficiency, retinal edema, seizure, skin photosensitivity, syncope, thrombocytopenia, vasculitis, weight loss
Warnings/Precautions
Concerns related to adverse effects:
- Cholelithiasis: May increase risk of cholelithiasis; discontinue if gallstones are found upon gallbladder studies.
- Elevated transaminases: Elevations in serum transaminases may be seen with use; periodic monitoring recommended.
- Hematologic effects: May cause mild decreases in hemoglobin, hematocrit, and WBC upon initiation which usually stabilizes with long-term therapy. Anemia, leukopenia, thrombocytopenia, and bone marrow hypoplasia have rarely been reported. Periodic monitoring recommended during the first year of therapy.
- Malignancy: Possible increased risk of malignancy.
- Myopathy/rhabdomyolysis: Has been associated with rare myositis or rhabdomyolysis; patients should be monitored closely. Patients should be instructed to report unexplained muscle pain, tenderness, weakness, or brown urine.
Disease-related concerns:
- Renal impairment: Use with caution in patients with mild-to-moderate renal impairment; contraindicated in patients with severe impairment. Deterioration has been seen when used in patients with a serum creatinine >2 mg/dL.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Other warnings/precautions:
- Appropriate use: Secondary causes of hyperlipidemia should be ruled out prior to therapy. Be careful in patient selection, this is not a first- or second-line choice; other agents may be more suitable. Discontinue if lipid response not seen.
Monitoring Parameters
Serum cholesterol, LFTs periodically, CBC periodically (first year)
Pregnancy
Pregnancy Considerations
Gemfibrozil crosses the placenta (Tsai 2004).
Triglyceride concentrations increase during pregnancy as required for normal fetal development. When increases are greater than expected, supervised dietary intervention should be initiated. In women who develop very severe hypertriglyceridemia and are at risk for pancreatitis, use of gemfibrozil beginning in the second trimester is one intervention that may be considered (Avis 2009; Berglund 2012; Jacobson 2015; Wong 2015).
Patient Education
What is this drug used for?
- It is used to lower bad cholesterol and raise good cholesterol (HDL).
- It is used to lower triglycerides.
Frequently reported side effects of this drug
- Heartburn
- Abdominal pain
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Gallstones like pain in the upper right abdominal area, right shoulder area, or between the shoulder blades; yellow skin; or fever with chills.
- Infection
- Muscle pain
- Muscle weakness
- Unable to pass urine
- Change in amount of urine passed
- Severe loss of strength and energy
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.