Boxed Warning
Embryofetal toxicity:
Leflunomide is contraindicated in pregnant women because of the potential for fetal harm. Teratogenicity and embryolethality occurred in animals administered leflunomide at doses lower than the human exposure level. Exclude pregnancy before the start of treatment with leflunomide in females of reproductive potential. Advise females of reproductive potential to use effective contraception during leflunomide treatment and during an accelerated elimination procedure after leflunomide treatment. Stop leflunomide and use an accelerated drug elimination procedure if the patient becomes pregnant.
Hepatotoxicity:
Severe liver injury, including fatal liver failure, has been reported in patients treated with leflunomide. Leflunomide is contraindicated in patients with severe hepatic impairment. Concomitant use of leflunomide with other potentially hepatotoxic drugs may increase the risk of liver injury. Patients with preexisting acute or chronic liver disease, or those with serum ALT >2 times ULN before initiating treatment, are at increased risk and should not be treated with leflunomide. Monitor ALT levels at least monthly for 6 months after starting leflunomide, and thereafter every 6 to 8 weeks. If leflunomide-induced liver injury is suspected, stop leflunomide treatment, start an accelerated drug elimination procedure, and monitor liver tests weekly until normalized.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
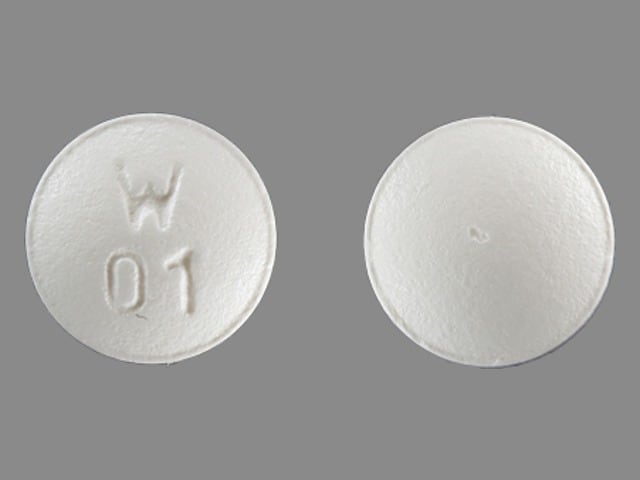
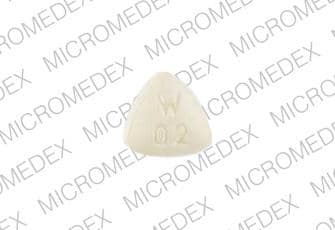
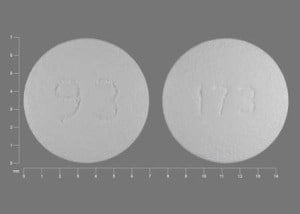
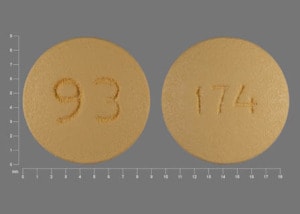
Tablet, Oral:
Arava: 10 mg, 20 mg
Generic: 10 mg, 20 mg
Pharmacology
Mechanism of Action
Leflunomide is an immunomodulatory agent that inhibits pyrimidine synthesis, resulting in antiproliferative and anti-inflammatory effects. Leflunomide is a prodrug; the active metabolite is responsible for activity. For CMV, may interfere with virion assembly.
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: Teriflunomide: 11 L
Metabolism
Hepatic to an active metabolite teriflunomide, which accounts for nearly all pharmacologic activity; further metabolism to multiple inactive metabolites; undergoes enterohepatic recirculation
Excretion
Feces (37.5%); urine (22.6%)
Time to Peak
Teriflunomide: 6 to 12 hours
Half-Life Elimination
Teriflunomide: Mean: 18 to 19 days; enterohepatic recycling appears to contribute to the long half-life of this agent, since activated charcoal and cholestyramine substantially reduce plasma half-life
Protein Binding
Teriflunomide: >99% to albumin
Use: Labeled Indications
Rheumatoid arthritis: Treatment of adults with active rheumatoid arthritis (RA).
Use: Off Label
BK virus (viremia or nephropathy; in kidney transplant recipients)cyes
Data from a small retrospective study suggest leflunomide may be of benefit as a replacement for mycophenolate in kidney transplant recipients with BK virus (viremia or nephropathy) Nesselhauf 2016. Clinical experience also suggests the utility of leflunomide in the management of BK virus in kidney transplant patients Gabardi 2018.
Based on guidelines for BK polyomavirus in solid organ transplantation from the American Society of Transplantation Infectious Diseases Community of Practice, switching immunosuppressive therapy from mycophenolate to leflunomide may be a potential strategy in kidney transplant patients with BK virus infection AST-IDCOP [Hirsch 2019].
Cytomegalovirus disease (in transplant recipients resistant to standard antivirals)c
Data from retrospective studies and case reports suggest leflunomide may be of benefit in the management of cytomegalovirus (CMV) viremia that is resistant to standard antiviral therapy in allogeneic bone marrow or stem cell transplant recipients Avery 2010, Gokarn 2019, Wang 2018. Data from a retrospective study suggest leflunomide may be of benefit in the management of CMV infection and as secondary prophylaxis in lung transplant patients Silva 2018. Data from case reports and a retrospective study suggest leflunomide may be of benefit in the management of CMV disease in solid organ transplant patients who were unable to receive standard antiviral therapy or in CMV which was refractory/resistant to standard antiviral therapy Avery 2010, Chon 2015, John 2004.
Contraindications
Known hypersensitivity (including anaphylaxis) to leflunomide or any component of the formulation; severe hepatic impairment; concomitant treatment with teriflunomide; pregnant females.
Canadian labeling: Additional contraindications (not in the US labeling): Hypersensitivity to teriflunomide; moderate to severe renal impairment; immunodeficiency states; impaired bone marrow function or significant anemia, leukopenia, neutropenia, or thrombocytopenia due to causes other than rheumatoid arthritis; serious infections; impaired liver function; severe hypoproteinemia; females of reproductive potential who are not using reliable contraception before, during, and for a period of 2 years after treatment with leflunomide (or as long as plasma levels of the active metabolite are above 0.02 mg/L); breastfeeding; patients <18 years of age.
Dosage and Administration
Dosing: Adult
BK virus (viremia or nephropathy), in kidney transplant recipients (off-label use; based on limited data): Oral: Loading dose: 100 mg/day for 5 days; Maintenance: 40 mg/day (AST-IDCOP [Hirsch 2019]; Nesselhauf 2016) or Loading dose: 60 mg/day for 2 days; Maintenance: 20 mg/day (Kable 2017); consider adjusting dose based on active metabolite serum concentrations (AST-IDCOP [Hirsch 2019]; Kable 2017; Nesselhauf 2016).
Cytomegalovirus disease, in transplant recipients resistant to standard antivirals, adjunctive therapy (off-label use; based on limited data): Oral: 100 mg once daily for 3 to 5 days, followed by 20 to 40 mg/day (Avery 2010; Chon 2015; Gokarn 2019; Silva 2018; Wang 2018); consider adjusting dose based on active metabolite serum concentrations and/or adverse events (Avery 2010; Wang 2018).
Rheumatoid arthritis: Oral: Loading dose (optional; see Note): 100 mg once daily for 3 days; maintenance dose: 20 mg once daily, may reduce dose to 10 mg once daily if higher dose is not tolerated (maximum dose: 20 mg once daily). Note: Loading dose may be omitted given the higher likelihood of side effects (eg, diarrhea), and especially may be omitted in patients at increased risk of hepatic or hematologic toxicity (eg, recent concomitant methotrexate or other immunosuppressive agents); onset of action may be delayed (Maddison 2005; Osiri 2003). Due to the long half-life of the active metabolite, serum concentrations may require a prolonged period to decline after dosage reduction.
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Juvenile idiopathic arthritis (off-label use) (Silverman 2005): Children ≥3 years and Adolescents: Oral:
<20 kg: 100 mg as a single dose followed by 10 mg every other day
20 kg to 40 kg: 100 mg once daily for 2 days followed by 10 mg once daily
>40 kg: 100 mg once daily for 3 days followed by 20 mg once daily
Administration
Administer without regard to meals.
Storage
Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Protect from light.
Leflunomide Images
Drug Interactions
Alpelisib: BCRP/ABCG2 Inhibitors may increase the serum concentration of Alpelisib. Management: Avoid coadministration of BCRP/ABCG2 inhibitors and alpelisib due to the potential for increased alpelisib concentrations and toxicities. If coadministration cannot be avoided, closely monitor for increased alpelisib adverse reactions. Consider therapy modification
Amodiaquine: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Amodiaquine. Avoid combination
Asunaprevir: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Asunaprevir. Avoid combination
Baricitinib: Immunosuppressants may enhance the immunosuppressive effect of Baricitinib. Management: Use of baricitinib in combination with potent immunosuppressants such as azathioprine or cyclosporine is not recommended. Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted. Consider therapy modification
BCG (Intravesical): Immunosuppressants may diminish the therapeutic effect of BCG (Intravesical). Avoid combination
Bendamustine: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Bendamustine. Concentrations of active metabolites may be increased. Management: Consider alternatives to moderate CYP1A2 inducers during therapy with bendamustine due to the potential for decreased bendamustine plasma concentrations and reduced efficacy. Consider therapy modification
Bile Acid Sequestrants: May decrease serum concentrations of the active metabolite(s) of Leflunomide. Management: Unless using this combination to intentionally enhance leflunomide elimination, consider an alternative to the bile acid sequestrants when possible. Separating drug administration is not likely to be effective at avoiding this interaction. Consider therapy modification
Caffeine and Caffeine Containing Products: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Caffeine and Caffeine Containing Products. Monitor therapy
Charcoal, Activated: May decrease serum concentrations of the active metabolite(s) of Leflunomide. Management: Unless using this combination to intentionally enhance leflunomide elimination, consider an alternative to charcoal when possible. Separating drug administration is not likely to be effective at avoiding this interaction. Consider therapy modification
Cladribine: May enhance the immunosuppressive effect of Immunosuppressants. Avoid combination
ClomiPRAMINE: CYP1A2 Inducers (Moderate) may decrease the serum concentration of ClomiPRAMINE. Monitor therapy
CloZAPine: CYP1A2 Inducers (Moderate) may decrease the serum concentration of CloZAPine. Monitor therapy
Coccidioides immitis Skin Test: Immunosuppressants may diminish the diagnostic effect of Coccidioides immitis Skin Test. Monitor therapy
Dabrafenib: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Dabrafenib. Monitor therapy
Dasabuvir: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Dasabuvir. Monitor therapy
Denosumab: May enhance the adverse/toxic effect of Immunosuppressants. Specifically, the risk for serious infections may be increased. Monitor therapy
Desloratadine: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Desloratadine. Monitor therapy
Dichlorphenamide: OAT1/3 Inhibitors may increase the serum concentration of Dichlorphenamide. Monitor therapy
DULoxetine: CYP1A2 Inducers (Moderate) may decrease the serum concentration of DULoxetine. Monitor therapy
Echinacea: May diminish the therapeutic effect of Immunosuppressants. Consider therapy modification
Elagolix: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Elagolix. Avoid combination
Enzalutamide: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Enzalutamide. Monitor therapy
Erlotinib: Leflunomide may decrease the serum concentration of Erlotinib. Management: Avoid the concomitant use of erlotinib and leflunomide if possible. If concomitant use is unavoidable, increase the erlotinib dose by 50 mg increments at 2-week intervals to a maximum of 300 mg. Consider therapy modification
Fingolimod: Immunosuppressants may enhance the immunosuppressive effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and other immunosuppressants when possible. If combined, monitor patients closely for additive immunosuppressant effects (eg, infections). Consider therapy modification
Grazoprevir: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Grazoprevir. Avoid combination
Immunosuppressants: May enhance the adverse/toxic effect of Leflunomide. Specifically, the risk for hematologic toxicity such as pancytopenia, agranulocytosis, and/or thrombocytopenia may be increased. Management: Consider not using a leflunomide loading dose in patients receiving other immunosuppressants. Patients receiving both leflunomide and another immunosuppressant should be monitored for bone marrow suppression at least monthly. Exceptions: Cytarabine (Liposomal). Consider therapy modification
Lidocaine (Systemic): CYP1A2 Inducers (Moderate) may decrease the serum concentration of Lidocaine (Systemic). Monitor therapy
Melatonin: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Melatonin. Monitor therapy
Methotrexate: May enhance the adverse/toxic effect of Leflunomide. Particular concerns are an increased risk of pancytopenia and/or hepatotoxicity. Monitor therapy
Mexiletine: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Mexiletine. Monitor therapy
Natalizumab: Immunosuppressants may enhance the adverse/toxic effect of Natalizumab. Specifically, the risk of concurrent infection may be increased. Avoid combination
Nivolumab: Immunosuppressants may diminish the therapeutic effect of Nivolumab. Consider therapy modification
OLANZapine: CYP1A2 Inducers (Moderate) may decrease the serum concentration of OLANZapine. Monitor therapy
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir. Specifically, the concentrations of the dasabuvir component may be increased. Monitor therapy
PAZOPanib: BCRP/ABCG2 Inhibitors may increase the serum concentration of PAZOPanib. Avoid combination
Pidotimod: Immunosuppressants may diminish the therapeutic effect of Pidotimod. Monitor therapy
Pimecrolimus: May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Pioglitazone: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Pioglitazone. Monitor therapy
Pirfenidone: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Pirfenidone. Monitor therapy
Propranolol: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Propranolol. Monitor therapy
Repaglinide: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Repaglinide. Monitor therapy
Revefenacin: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase serum concentrations of the active metabolite(s) of Revefenacin. Avoid combination
RifAMPin: May increase serum concentrations of the active metabolite(s) of Leflunomide. Monitor therapy
Riluzole: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Riluzole. Monitor therapy
Roflumilast: May enhance the immunosuppressive effect of Immunosuppressants. Consider therapy modification
ROPINIRole: CYP1A2 Inducers (Moderate) may decrease the serum concentration of ROPINIRole. Monitor therapy
Selexipag: CYP2C8 Inhibitors (Moderate) may increase serum concentrations of the active metabolite(s) of Selexipag. Management: Reduce the selexipag dose to once daily when combined with moderate CYP2C8 inhibitors. Revert back to twice daily selexipag dosing upon stopping the moderate CYP2C8 inhibitor. Consider therapy modification
Sipuleucel-T: Immunosuppressants may diminish the therapeutic effect of Sipuleucel-T. Management: Evaluate patients to see if it is medically appropriate to reduce or discontinue therapy with immunosuppressants prior to initiating sipuleucel-T therapy. Consider therapy modification
Tacrolimus (Topical): May enhance the adverse/toxic effect of Immunosuppressants. Avoid combination
Talazoparib: BCRP/ABCG2 Inhibitors may increase the serum concentration of Talazoparib. Monitor therapy
Tasimelteon: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Tasimelteon. Monitor therapy
Teriflunomide: Leflunomide may enhance the adverse/toxic effect of Teriflunomide. Leflunomide may increase the serum concentration of Teriflunomide. Avoid combination
Tertomotide: Immunosuppressants may diminish the therapeutic effect of Tertomotide. Monitor therapy
Theophylline Derivatives: CYP1A2 Inducers (Moderate) may decrease the serum concentration of Theophylline Derivatives. Exceptions: Dyphylline. Monitor therapy
TiZANidine: CYP1A2 Inducers (Moderate) may decrease the serum concentration of TiZANidine. Monitor therapy
Tobacco (Smoked): May decrease the serum concentration of Leflunomide. Monitor therapy
Tofacitinib: Immunosuppressants may enhance the immunosuppressive effect of Tofacitinib. Management: Concurrent use with antirheumatic doses of methotrexate or nonbiologic disease modifying antirheumatic drugs (DMARDs) is permitted, and this warning seems particularly focused on more potent immunosuppressants. Consider therapy modification
TOLBUTamide: Leflunomide may increase the serum concentration of TOLBUTamide. Specifically, the active metabolite of leflunomide (teriflunomide) may both increase total tolbutamide concentrations and increase the free fraction (i.e., non-protein bound) of tolbutamide. TOLBUTamide may increase the serum concentration of Leflunomide. Specifically, tolbutamide may increase the proportion of non-protein-bound (i.e., free fraction) teriflunomide. Monitor therapy
Topotecan: BCRP/ABCG2 Inhibitors may increase the serum concentration of Topotecan. Avoid combination
Trastuzumab: May enhance the neutropenic effect of Immunosuppressants. Monitor therapy
Treprostinil: CYP2C8 Inhibitors (Moderate) may increase the serum concentration of Treprostinil. Monitor therapy
Ubrogepant: BCRP/ABCG2 Inhibitors may increase the serum concentration of Ubrogepant. Management: Use an initial ubrogepant dose of 50 mg and second dose (if needed) of 50 mg when used with a BCRP inhibitor. Consider therapy modification
Vaccines (Inactivated): Immunosuppressants may diminish the therapeutic effect of Vaccines (Inactivated). Management: Vaccine efficacy may be reduced. Complete all age-appropriate vaccinations at least 2 weeks prior to starting an immunosuppressant. If vaccinated during immunosuppressant therapy, revaccinate at least 3 months after immunosuppressant discontinuation. Consider therapy modification
Vaccines (Live): Leflunomide may enhance the adverse/toxic effect of Vaccines (Live). Leflunomide may diminish the therapeutic effect of Vaccines (Live). Management: The ACIP guidelines state that live-attenuated vaccines should generally be avoided for at least 3 months after cessation of immunosuppressant therapy. However, the ACR does not recommend avoiding live vaccines in patients being treated with leflunomide. Consider therapy modification
Vitamin K Antagonists (eg, warfarin): Leflunomide may enhance the anticoagulant effect of Vitamin K Antagonists. Leflunomide may diminish the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Voxilaprevir: OATP1B1/1B3 (SLCO1B1/1B3) Inhibitors may increase the serum concentration of Voxilaprevir. Avoid combination
Adverse Reactions
>10%:
Central nervous system: Headache (7% to 13%)
Dermatologic: Alopecia (9% to 17%), skin rash (10% to 12%)
Gastrointestinal: Diarrhea (17% to 27%), nausea (9% to 13%)
1% to 10%:
Cardiovascular: Hypertension (9% to 10%)
Central nervous system: Dizziness (4% to 7%)
Dermatologic: Pruritus (4% to 6%)
Gastrointestinal: Gastrointestinal pain (5% to 8%), abdominal pain (5% to 6%), oral mucosa ulcer (3% to 5%), vomiting (3% to 5%)
Hepatic: Abnormal hepatic function tests (5% to 10%), increased serum ALT (>3 x ULN: 2% to 4%; reversible)
Hypersensitivity: Hypersensitivity reaction (1% to 5%)
Neuromuscular & skeletal: Back pain (5% to 8%), weakness (3% to 6%), tenosynovitis (2% to 5%)
Respiratory: Bronchitis (5% to 8%), rhinitis (2% to 5%)
Frequency not defined:
Cardiovascular: Chest pain, increased blood pressure, leg thrombophlebitis, palpitations, varicose veins
Central nervous system: Drowsiness, malaise
Endocrine & metabolic: Increased gamma-glutamyl transferase
Gastrointestinal: Anorexia, enlargement of salivary glands, flatulence, sore throat, xerostomia
Genitourinary: Vulvovaginal candidiasis
Hematologic & oncologic: Leukocytosis, thrombocytopenia
Hepatic: Hyperbilirubinemia, increased serum alkaline phosphatase, increased serum AST
Hypersensitivity: Anaphylaxis
Infection: Abscess
Ophthalmic: Blurred vision, eye disease, papilledema, retinal hemorrhage, retinopathy
Respiratory: Dyspnea, flu-like symptoms
<1%, postmarketing and/or case reports: Agranulocytosis, angioedema, cholestasis, colitis (including microscopic colitis), cutaneous lupus erythematosus, DRESS syndrome, erythema multiforme, exacerbation of psoriasis, hepatitis, hepatotoxicity (rare, including hepatic necrosis and hepatic failure), interstitial pneumonitis, interstitial pulmonary disease, jaundice, leukopenia, necrotizing angiitis (cutaneous), neutropenia, opportunistic infection, pancreatitis, pancytopenia, peripheral neuropathy, pulmonary fibrosis, pulmonary hypertension, pustular psoriasis, sepsis (including Pneumocystis jirovecii pneumonia and aspergillosis), severe infection, Stevens-Johnson syndrome, toxic epidermal necrolysis, vasculitis
Warnings/Precautions
Concerns related to adverse effects:
- Dermatologic reactions: Rare cases of dermatologic reactions (including Stevens-Johnson syndrome, toxic epidermal necrolysis, and drug reaction with eosinophilia and systemic symptoms) have been reported; discontinue if evidence of severe dermatologic reaction occurs, and begin accelerated drug elimination procedures.
- Hepatotoxicity: [US Boxed Warning]: Severe liver injury, including fatal liver failure, has been reported in some patients treated with leflunomide. Leflunomide is contraindicated in patients with severe hepatic impairment. Concomitant use of leflunomide with other potentially hepatotoxic drugs may increase the risk of liver injury. Patients with preexisting acute or chronic liver disease, or those with ALT >2 times the ULN before initiating treatment, are at increased risk and should not be treated with leflunomide. Monitor ALT levels at least monthly for 6 months after starting leflunomide, and thereafter every 6 to 8 weeks. If ALT elevation >3 times the ULN occurs, interrupt therapy and investigate the cause. If leflunomide-induced liver injury is suspected, stop leflunomide treatment, start an accelerated drug elimination procedure, and monitor liver tests weekly until normalized. If leflunomide-induced liver injury is unlikely because another cause has been found, resumption of leflunomide therapy may be considered. If given concomitantly with methotrexate, follow the American College of Rheumatology guidelines for monitoring methotrexate liver toxicity with ALT, AST, and serum albumin testing.
- Hematologic toxicities: Pancytopenia, agranulocytosis, and thrombocytopenia have been reported with leflunomide therapy alone; most frequently hematologic toxicity occurs in patients receiving concomitant therapy with methotrexate or other immunosuppressive agents, or who had recently discontinued these therapies. In some cases, patients had a history of a significant hematologic abnormality. All patients should have platelet, WBC, and hemoglobin or hematocrit monitored at baseline and monthly for 6 months following therapy initiation and then every 6 to 8 weeks thereafter. If used with concomitant methotrexate or other potential immunosuppressive agents, increase chronic monitoring to monthly. If evidence of bone marrow suppression occurs, stop treatment and initiate an accelerated drug elimination procedure. Avoid use in patients with bone marrow dysplasia.
- Hypertension: Blood pressure elevations have been observed; assess blood pressure at baseline and monitor periodically during therapy.
- Infections: May increase susceptibility to infection, including opportunistic pathogens (especially Pneumocystis jirovecii pneumonia, tuberculosis [including extrapulmonary tuberculosis], and aspergillosis). Severe infections, sepsis, and fatalities have been reported. Not recommended in patients with severe immunodeficiency or severe, uncontrolled infections. Caution should be exercised when considering the use in patients with a history of new/recurrent infections, with conditions that predispose them to infections, or with chronic, latent, or localized infections. Patients who develop a new infection while undergoing treatment should be monitored closely; consider interrupting therapy and initiating accelerated drug elimination procedures if infection is serious. Patients should be screened for tuberculosis (active and latent) and if necessary, treated prior to initiating leflunomide therapy. Safety has not been established in patients with latent tuberculosis infection.
- Interstitial lung disease: Interstitial lung disease and worsening of preexisting interstitial lung disease have been reported (with some fatalities). The risk is increased in patients with a history of interstitial lung disease. Further investigate etiology in patients who develop new-onset or worsening of pulmonary symptoms (eg, cough and dyspnea, with or without associated fever). Accelerated drug elimination procedures should be considered if leflunomide is discontinued due to interstitial lung disease.
- Malignancy: Use of some immunosuppressive medications may increase the risk of malignancies, especially lymphoproliferative disorders; impact of leflunomide on the development and course of malignancies is not fully defined.
- Peripheral neuropathy: Cases of peripheral neuropathy have been reported; most patients recover after treatment discontinuation, but symptoms may persist in some patients. The risk for peripheral neuropathy may be increased in patients >60 years of age, receiving concomitant neurotoxic medications or patients with diabetes. If peripheral neuropathy occurs, consider discontinuing leflunomide and consider accelerated drug elimination procedures.
Disease-related concerns:
- Renal impairment: Use with caution in patients with renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
- Immunizations: No clinical data are available on the efficacy and safety of vaccinations during leflunomide treatment. Vaccination with live vaccines is not recommended; consider the long elimination half-life of the leflunomide active metabolite (eg, teriflunomide) when considering live vaccine administration after leflunomide discontinuation.
Special populations:
- Females of reproductive potential: [US Boxed Warning]: Leflunomide is contraindicated in pregnant females because of the potential for fetal harm. Adverse events were observed in animal reproduction studies with doses lower than the expected human exposure. Discontinue leflunomide and use an accelerated elimination procedure if pregnancy occurs during treatment. Exclude pregnancy before the start of treatment in females of reproductive potential. Advise females of reproductive potential to use effective contraception during treatment and during an accelerated elimination procedure after treatment is discontinued.
Other warnings/precautions:
- Drug elimination procedure: Due to slow elimination and variations in clearance, it may take up to 2 years to reach low levels of leflunomide metabolite (eg, teriflunomide) serum concentrations. An accelerated drug elimination procedure using cholestyramine or activated charcoal is recommended when a more rapid elimination is needed (eg, severe adverse reaction, suspected hypersensitivity or pregnancy). Refer to the manufacturer's labeling for detailed accelerated elimination procedure. Verify plasma teriflunomide concentrations are <0.02 mg/L by tests at least 14 days apart. If concentrations are >0.02 mg/L, repeat the accelerated elimination procedure. Use of accelerated drug elimination may potentially result in return of disease activity if the patient has been responding to leflunomide treatment.
Monitoring Parameters
Rheumatoid arthritis:
Manufacturer's labeling: Pregnancy test to rule out pregnancy prior to initiating therapy (in females of reproductive potential); baseline evaluation for active tuberculosis and screen patients for latent tuberculosis; blood pressure (baseline and periodically thereafter); signs/symptoms of severe infection or pulmonary symptoms (eg, cough, dyspnea); CBC (WBC, platelet count, hemoglobin, or hematocrit) at baseline and monthly during the initial 6 months of treatment; if stable, monitoring frequency may be decreased to every 6 to 8 weeks thereafter (continue monthly when used in combination with other immunosuppressive agents [eg, methotrexate]); hepatic function (transaminases) at least monthly for the first 6 months of treatment, then every 6 to 8 weeks thereafter (discontinue if ALT >3 times ULN, treat with accelerated elimination procedure, and monitor liver function at least weekly until normal).
Alternate recommendations: CBC, serum creatinine, serum transaminases: Baseline and every 2 to 4 weeks during the initial 3 months after initiation or following dose increases, then every 8 to 12 weeks during 3 to 6 months of treatment, followed by every 12 weeks beyond 6 months of treatment; monitor more frequently if clinically indicated (ACR [Singh 2016]).
BK virus and cytomegalovirus disease (off-label uses): Monitor serum trough concentrations of active metabolite (also see Reference Range) (AST-IDCOP [Hirsch 2019]; Kable 2017; Nesselhauf 2016).
Pregnancy
Pregnancy Considerations
[US Boxed Warning]: Leflunomide is contraindicated in pregnant females because of the potential for fetal harm. Adverse events were observed in animal reproduction studies with doses lower than the expected human exposure. Discontinue leflunomide and use an accelerated elimination procedure if pregnancy occurs during treatment. The accelerated elimination procedure may decrease potential risks to the fetus by decreasing the plasma concentration teriflunomide, of the active metabolite of leflunomide. Following treatment, pregnancy should be avoided until undetectable serum concentrations (<0.02 mg/L) are verified. Limited outcome information following in utero fetal exposure to leflunomide is available (Bérard 2018; Chambers 2010; Weber-Schoendorfer 2017).
[US Boxed Warning]: Exclude pregnancy before the start of treatment in females of reproductive potential. Advise females of reproductive potential to use effective contraception during treatment and during an accelerated elimination procedure after treatment is discontinued. Females of reproductive potential should not receive therapy until pregnancy has been excluded, they have been counseled concerning fetal risk, and reliable contraceptive measures have been confirmed. Following treatment, pregnancy should be avoided until undetectable serum concentrations (<0.02 mg/L) are verified. This may be accomplished by the use of an enhanced drug elimination procedure using cholestyramine. Serum concentrations <0.02 mg/L should be verified by 2 separate tests performed at least 14 days apart. If serum concentrations are >0.02 mg/L, additional cholestyramine treatment should be considered. Use of the accelerated elimination procedure is recommended in all females of reproductive potential upon discontinuation of leflunomide.
Health care providers are encouraged to enroll women exposed to leflunomide during pregnancy in the Pregnancy Registry (877-311-8972 or http://www.pregnancystudies.org/participate-ina-study/).
Patient Education
What is this drug used for?
- It is used to treat rheumatoid arthritis.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Diarrhea
- Hair loss
- Abdominal pain
- Fatigue
- Back pain
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin
- Severe headache
- Severe dizziness
- Passing out
- Vision changes
- Burning or numbness feeling
- Pale skin
- Bruising
- Bleeding
- Severe loss of strength and energy
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes
- Severe pulmonary disorder like lung or breathing problems like trouble breathing, shortness of breath, or a cough that is new or worse
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.