Boxed Warning
Exacerbation of ischemic heart disease following abrupt withdrawal:
Hypersensitivity to catecholamines has been observed in patients withdrawn from beta-blocker therapy; exacerbation of angina and, in some cases, myocardial infarction have occurred after abrupt discontinuation of such therapy. When discontinuing nadolol administered long term, particularly in patients with ischemic heart disease, gradually reduce the dosage over a period of 1 to 2 weeks and carefully monitor the patient. If angina markedly worsens or acute coronary insufficiency develops, reinstitute nadolol administration promptly, at least temporarily, and take other measures appropriate for the management of unstable angina. Warn patients against interruption or discontinuation of therapy without the health care provider's advice. Because coronary artery disease is common and may be unrecognized, it may be prudent not to discontinue nadolol therapy abruptly, even in patients treated only for hypertension.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Tablet, Oral:
Corgard: 20 mg [DSC]
Corgard: 20 mg [scored; contains fd&c blue #2 (indigotine)]
Corgard: 40 mg [DSC]
Corgard: 40 mg [scored; contains fd&c blue #2 (indigotine)]
Corgard: 80 mg [DSC]
Corgard: 80 mg [scored; contains fd&c blue #2 (indigotine)]
Generic: 20 mg, 40 mg, 80 mg
Pharmacology
Mechanism of Action
Competitively blocks response to beta1- and beta2-adrenergic stimulation; does not exhibit any membrane stabilizing or intrinsic sympathomimetic activity. Nonselective beta-adrenergic blockers (propranolol, nadolol) reduce portal pressure by producing splanchnic vasoconstriction (beta2 effect) thereby reducing portal blood flow.
Pharmacokinetics/Pharmacodynamics
Absorption
~30%
Distribution
Vd: ~2 L/kg
Metabolism
Not metabolized
Excretion
Urine (as unchanged drug)
Time to Peak
Serum: 3 to 4 hours
Duration of Action
17 to 24 hours
Half-Life Elimination
Infants 3 to 22 months (n=3): 3.2 to 4.3 hours (Mehta 1992)
Children 10 years (n=1): 15.7 hours (Mehta 1992)
Children ~15 years (n=1): 7.3 hours (Mehta 1992)
Adults: 20 to 24 hours; prolonged with renal impairment; (up to 45 hours in severe impairment) (Herrera 1979)
Protein Binding
30%
Use: Labeled Indications
Angina: Treatment of angina pectoris
Hypertension: Management of hypertension. Note: Beta-blockers are not recommended as first-line therapy (ACC/AHA [Whelton 2017]).
Use: Off Label
Atrial fibrillation (rate control)yes
Based on the 2014 American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for the management of patients with atrial fibrillation (AF), the use of beta-blockers, including nadolol, for ventricular rate control in patients with paroxysmal, persistent, or permanent AF is effective and recommended for this condition.
Catecholaminergic polymorphic ventricular tachycardia (prevention)cyes
In patients with catecholaminergic polymorphic ventricular tachycardia (CPVT), data from an observational study suggests that beta-blockers, especially nadolol, may be beneficial at reducing the risk of cardiac events Hayashi 2009. Additional data may be necessary to further define the role of nadolol in this condition.
Based on the American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for management of patients with ventricular arrhythmias and prevention of sudden cardiac death, beta-blockers are effective for control of CPVT.
Gastroesophageal variceal hemorrhage prophylaxis in patients with cirrhosisbyes
Data from a meta-analysis and randomized controlled trials support the use of nadolol for primary prophylaxis against first variceal hemorrhage Lo 2004, Lo 2010, Poynard 1991 and secondary prophylaxis against recurrent variceal hemorrhage de la Peña 2005.
Based on the American Association for the Study of Liver Diseases guidelines on the management of portal hypertensive bleeding in cirrhosis and the British Society of Gastroenterology guidelines on the management of variceal hemorrhage in cirrhotic patients, use of nonselective beta-blockers, such as nadolol, is effective and recommended for primary and secondary prophylaxis of variceal hemorrhage
Migraine prophylaxisyes
Based on the American Academy of Neurology and the American Headache Society evidence-based guideline update: Pharmacologic treatment for episodic migraine prevention in adults, the use of nadolol (among other beta-blockers) is probably effective and may be considered for migraine prevention. No specific dosing recommendations provided.
Supraventricular tachycardia (atrioventricular nodal reentrant tachycardia, atrioventricular reentrant tachycardia, atrial flutter, focal atrial tachycardia)yes
Based on the American College of Cardiology/American Heart Association/Heart Rhythm Society guidelines for the management of patients with supraventricular arrhythmias, the use of an oral beta-blocker, including nadolol, is effective and recommended for the ongoing management of a variety of symptomatic supraventricular tachycardias (atrioventricular nodal reentrant tachycardia [AVNRT], atrioventricular reentrant tachycardia [AVRT], focal atrial tachycardia [AT]) without pre-excitation in patients who are not candidates for, or prefer not to undergo catheter ablation. Oral beta-blockers, including nadolol, may also be useful for the ongoing management (rate control) in hemodynamically stable patients with atrial flutter.
Thyrotoxicosisyes
Based on the 2016 American Thyroid Association guidelines for diagnosis and management of hyperthyroidism and other causes of thyrotoxicosis, beta-blockers, including nadolol, are effective and recommended in the treatment symptomatic thyrotoxicosis. However, experience with nadolol is limited compared to other beta-blockers. Beta-blockers should also be considered in asymptomatic patients who are at increased risk of complications due to worsening hyperthyroidism Ross 2016.
Ventricular arrhythmias due to congenital long QT syndrome (prevention)cyes
In patients with congenital long QT syndrome (LQTS), data from observational studies suggest that beta-blockers may be beneficial at reducing the risk of cardiac events, including ventricular arrhythmias, especially in patients with congenital LQTS type 1 or type 2 Chockalingam 2012, Goldenberg 2010, Moss 2000, Sauer 2007. Additional data may be necessary to further define the role of nadolol in this condition. Atenolol, nadolol, and propranolol may be preferred for patients with LQTS based on the currently available data.
Based on the American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for management of patients with ventricular arrhythmias and prevention of sudden cardiac death, beta-blockers are effective for control of ventricular arrhythmias in patients with congenital LQTS.
Ventricular premature beat (suppression)yes
Based on the American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for management of patients with ventricular arrhythmias and prevention of sudden cardiac death, beta-blockers are effective for control of ventricular premature beats.
Ventricular tachycardia (prevention)yes
Based on the American Heart Association/American College of Cardiology/Heart Rhythm Society (AHA/ACC/HRS) guideline for management of patients with ventricular arrhythmias and prevention of sudden cardiac death, beta-blockers are effective for prevention of ventricular tachycardia.
Contraindications
Bronchial asthma; sinus bradycardia; heart block greater than first degree (except in patients with a functioning artificial pacemaker); cardiogenic shock; uncompensated cardiac failure
Documentation of allergenic cross-reactivity for beta-blockers is limited. However, because of similarities in chemical structure and/or pharmacologic actions, the possibility of cross-sensitivity cannot be ruled out with certainty.
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to nadolol or any component of the formulation; cor pulmonale; anesthesia with agents that produce myocardial depression; allergic rhinitis, bronchospasm, or severe chronic obstructive pulmonary disease (COPD)
Dosage and Administration
Dosing: Adult
Angina: Oral: Initial: 40 mg once daily, increase dosage gradually by 40 to 80 mg increments at 3- to 7-day intervals until optimum clinical response is obtained; usual dose: 40 to 80 mg once daily; doses may be titrated up to 160 or 240 mg once daily
Atrial fibrillation (rate control) (off-label use): Oral: Usual maintenance dose: 10 to 240 mg once daily (AHA/ACC/HRS [January 2014])
Catecholaminergic polymorphic ventricular tachycardia (prevention) (off-label use): Oral: 40 to 320 mg once daily (AHA/ACC/HRS [Al-Khatib 2017]; Claudio 2018; Hyashi 2009)
Gastroesophageal variceal hemorrhage prophylaxis in patients with cirrhosis (off-label use): Oral: Initial: 40 mg once daily (de la Peña 2005; Garcia-Tsao 2017; Lo 2004; Lo 2009; Lo 2010; Lo 2012); consider starting with 20 mg once daily if concern for hypotension (Garcia-Tsao 2017; Sanyal 2018); adjust every 2 to 3 days to maximal tolerated dose or until heart rate is ~55 to 60 beats per minute (Garcia-Tsao 2017). If systolic blood pressure is <90 mm Hg, reduce dose or discontinue. Some experts recommend a maximum dose of 160 mg/day in patients without ascites and 80 mg/day in patients with ascites (Garcia-Tsao 2017). Note: May use for primary or secondary prophylaxis. Primary prophylaxis is indicated for patients with cirrhosis and medium/large varices, variceal red wale markings on endoscopy, or decompensation and small varices (Garcia-Tsao 2017).
Hypertension (alternative agent): Oral: Initial: 40 mg once daily; titrate as needed based on patient response by 40 to 80 mg increments; usual dosage range: 40 to 120 mg once daily (ACC/AHA [Whelton 2017]). Doses up to 320 mg once daily may be necessary.
Supraventricular tachycardia (off-label use): Oral: Initial: 40 mg once daily; maximum maintenance dose: 320 mg once daily (ACC/AHA/HRS [Page 2015])
Thyrotoxicosis (off-label use): Oral: 40 to 160 mg once daily (Ross 2016)
Ventricular arrhythmias due to congenital long QT syndrome (prevention) (off-label use): Oral: 40 to 320 mg daily (AHA/ACC/HRS [Al-Khatib 2017])
Ventricular premature beat (suppression) (off-label use): Oral: 40 to 320 mg daily (AHA/ACC/HRS [Al-Khatib 2017])
Ventricular tachycardia (prevention) (off-label use): Oral: 40 to 320 mg daily (AHA/ACC/HRS [Al-Khatib 2017])
Dosing: Geriatric
Refer to adult dosing. In the management of hypertension, consider lower initial doses (eg, 20 mg daily) and titrate to response (Aronow 2011).
Dosing: Pediatric
Supraventricular tachycardia (SVT), treatment: Limited data available: Infants, Children, and Adolescents: Oral: Initial: 0.5 to 1 mg/kg/day once daily or in 2 divided doses; increase dose gradually based on clinical response to a maximum of 2.5 mg/kg/day (Mehta 1992a; von Alvensleben 2017). Dosing based on a trial of 26 pediatric patients (age range: 3 months to 15 years) which showed SVT was well controlled with a median dose of 1 mg/kg/day (Mehta 1992a) and a retrospective study of 20 patients with SVT (age range: 10 to 390 days [median age: 30 days]) treated with nadolol 0.5 to 2 mg/kg/day (80% of patients responded to1 mg/kg/day) in 1 to 2 divided doses; 85% of patients were SVT free at 1 year (von Alvensleben 2017).
Extemporaneously Prepared
10 mg/mL oral solution
A 10 mg/mL nadolol oral suspension may be made with tablets in a 1:1 mixture of Ora-Plus and Ora-Sweet. Crush ten 80 mg nadolol tablets in a glass mortar and reduce to a fine powder. Prepare the vehicle by mixing 35 mL of Ora-Plus and 35 mL of Ora-Sweet; stir vigorously. Add a small amount of the vehicle to the powder to make a smooth suspension. Then add remaining vehicle in geometric proportions and mix well. Transfer the mixture to a 4-ounce amber plastic prescription bottle. Rinse mortar with a small quantity of the vehicle sufficient to make a final volume of 80 mL. Label "shake well" and "refrigerate." Stable for 30 days when stored in amber plastic prescription bottles under refrigeration.
Nahata MC, Pai VB. Pediatric Drug Formulations. 6th ed. Cincinnati, OH: Harvey Whitney Books, 2011.
Administration
Oral: May be administered without regard to meals.
Storage
Store at room temperature; avoid excessive heat. Protect from light.
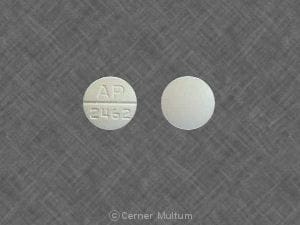
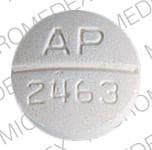
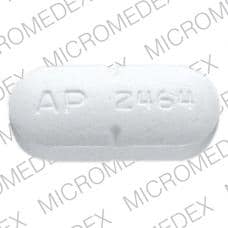
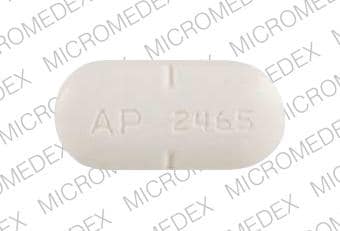
Nadolol Images
Drug Interactions
Acetylcholinesterase Inhibitors: May enhance the bradycardic effect of Beta-Blockers. Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alpha1-Blockers: Beta-Blockers may enhance the orthostatic hypotensive effect of Alpha1-Blockers. The risk associated with ophthalmic products is probably less than systemic products. Monitor therapy
Alpha2-Agonists: May enhance the AV-blocking effect of Beta-Blockers. Sinus node dysfunction may also be enhanced. Beta-Blockers may enhance the rebound hypertensive effect of Alpha2-Agonists. This effect can occur when the Alpha2-Agonist is abruptly withdrawn. Management: Closely monitor heart rate during treatment with a beta blocker and clonidine. Withdraw beta blockers several days before clonidine withdrawal when possible, and monitor blood pressure closely. Recommendations for other alpha2-agonists are unavailable. Exceptions: Apraclonidine. Consider therapy modification
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
Amiodarone: May enhance the bradycardic effect of Beta-Blockers. Possibly to the point of cardiac arrest. Amiodarone may increase the serum concentration of Beta-Blockers. Monitor therapy
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Beta2-Agonists: Beta-Blockers (Nonselective) may diminish the bronchodilatory effect of Beta2-Agonists. Avoid combination
Bradycardia-Causing Agents: May enhance the bradycardic effect of other Bradycardia-Causing Agents. Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Bupivacaine: Beta-Blockers may increase the serum concentration of Bupivacaine. Monitor therapy
Calcium Channel Blockers (Nondihydropyridine): May enhance the hypotensive effect of Beta-Blockers. Bradycardia and signs of heart failure have also been reported. Calcium Channel Blockers (Nondihydropyridine) may increase the serum concentration of Beta-Blockers. Exceptions: Bepridil. Monitor therapy
Cardiac Glycosides: Beta-Blockers may enhance the bradycardic effect of Cardiac Glycosides. Monitor therapy
Ceritinib: Bradycardia-Causing Agents may enhance the bradycardic effect of Ceritinib. Management: If this combination cannot be avoided, monitor patients for evidence of symptomatic bradycardia, and closely monitor blood pressure and heart rate during therapy. Exceptions are discussed in separate monographs. Consider therapy modification
Cholinergic Agonists: Beta-Blockers may enhance the adverse/toxic effect of Cholinergic Agonists. Of particular concern are the potential for cardiac conduction abnormalities and bronchoconstriction. Monitor therapy
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Dipyridamole: May enhance the bradycardic effect of Beta-Blockers. Monitor therapy
Disopyramide: May enhance the bradycardic effect of Beta-Blockers. Beta-Blockers may enhance the negative inotropic effect of Disopyramide. Monitor therapy
Dronedarone: May enhance the bradycardic effect of Beta-Blockers. Dronedarone may increase the serum concentration of Beta-Blockers. This likely applies only to those agents that are metabolized by CYP2D6. Management: Use lower initial beta-blocker doses; adequate tolerance of the combination, based on ECG findings, should be confirmed prior to any increase in beta-blocker dose. Consider therapy modification
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
EPINEPHrine (Nasal): Beta-Blockers (Nonselective) may enhance the hypertensive effect of EPINEPHrine (Nasal). Monitor therapy
EPINEPHrine (Oral Inhalation): Beta-Blockers (Nonselective) may enhance the hypertensive effect of EPINEPHrine (Oral Inhalation). Monitor therapy
Epinephrine (Racemic): Beta-Blockers (Nonselective) may enhance the hypertensive effect of Epinephrine (Racemic). Monitor therapy
EPINEPHrine (Systemic): Beta-Blockers (Nonselective) may enhance the hypertensive effect of EPINEPHrine (Systemic). Monitor therapy
Erdafitinib: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Ergot Derivatives: Beta-Blockers may enhance the vasoconstricting effect of Ergot Derivatives. Exceptions: Nicergoline. Consider therapy modification
Fexinidazole [INT]: Bradycardia-Causing Agents may enhance the arrhythmogenic effect of Fexinidazole [INT]. Avoid combination
Fingolimod: Beta-Blockers may enhance the bradycardic effect of Fingolimod. Management: Avoid the concomitant use of fingolimod and beta-blockers if possible. If coadministration is necessary, patients should have overnight continuous ECG monitoring conducted after the first dose of fingolimod. Monitor patients for bradycardia. Consider therapy modification
Floctafenine: May enhance the adverse/toxic effect of Beta-Blockers. Avoid combination
Grass Pollen Allergen Extract (5 Grass Extract): Beta-Blockers may enhance the adverse/toxic effect of Grass Pollen Allergen Extract (5 Grass Extract). More specifically, Beta-Blockers may inhibit the ability to effectively treat severe allergic reactions to Grass Pollen Allergen Extract (5 Grass Extract) with epinephrine. Some other effects of epinephrine may be unaffected or even enhanced (e.g., vasoconstriction) during treatment with Beta-Blockers. Consider therapy modification
Green Tea: May decrease the serum concentration of Nadolol. Management: Advise patients to minimize green tea consumption during nadolol treatment. The impact of separating nadolol doses from green tea consumption has not been investigated. Consider therapy modification
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Insulins: Beta-Blockers may enhance the hypoglycemic effect of Insulins. Monitor therapy
Ivabradine: Bradycardia-Causing Agents may enhance the bradycardic effect of Ivabradine. Monitor therapy
Lacosamide: Bradycardia-Causing Agents may enhance the AV-blocking effect of Lacosamide. Monitor therapy
Lasmiditan: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Avoid combination
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lidocaine (Systemic): Beta-Blockers may increase the serum concentration of Lidocaine (Systemic). Monitor therapy
Lidocaine (Topical): Beta-Blockers may increase the serum concentration of Lidocaine (Topical). Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Lumacaftor and Ivacaftor: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. Lumacaftor and Ivacaftor may increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Mepivacaine: Beta-Blockers may increase the serum concentration of Mepivacaine. Monitor therapy
Methacholine: Beta-Blockers may enhance the adverse/toxic effect of Methacholine. Monitor therapy
Methoxyflurane: May enhance the hypotensive effect of Beta-Blockers. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Midodrine: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
NIFEdipine: May enhance the hypotensive effect of Beta-Blockers. NIFEdipine may enhance the negative inotropic effect of Beta-Blockers. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May diminish the antihypertensive effect of Beta-Blockers. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Opioids (Anilidopiperidine): May enhance the bradycardic effect of Beta-Blockers. Opioids (Anilidopiperidine) may enhance the hypotensive effect of Beta-Blockers. Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
P-glycoprotein/ABCB1 Inducers: May decrease the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inducers may also further limit the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
P-glycoprotein/ABCB1 Inhibitors: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. P-glycoprotein inhibitors may also enhance the distribution of p-glycoprotein substrates to specific cells/tissues/organs where p-glycoprotein is present in large amounts (e.g., brain, T-lymphocytes, testes, etc.). Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Ranolazine: May increase the serum concentration of P-glycoprotein/ABCB1 Substrates. Monitor therapy
Regorafenib: May enhance the bradycardic effect of Beta-Blockers. Monitor therapy
Reserpine: May enhance the hypotensive effect of Beta-Blockers. Monitor therapy
Rivastigmine: May enhance the bradycardic effect of Beta-Blockers. Avoid combination
Ruxolitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Management: Ruxolitinib Canadian product labeling recommends avoiding use with bradycardia-causing agents to the extent possible. Monitor therapy
Siponimod: Bradycardia-Causing Agents may enhance the bradycardic effect of Siponimod. Management: Avoid coadministration of siponimod with drugs that may cause bradycardia. Consider therapy modification
Sulfonylureas: Beta-Blockers may enhance the hypoglycemic effect of Sulfonylureas. Cardioselective beta-blockers (eg, acebutolol, atenolol, metoprolol, and penbutolol) may be safer than nonselective beta-blockers. All beta-blockers appear to mask tachycardia as an initial symptom of hypoglycemia. Ophthalmic beta-blockers are probably associated with lower risk than systemic agents. Monitor therapy
Terlipressin: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Theophylline Derivatives: Beta-Blockers (Nonselective) may diminish the bronchodilatory effect of Theophylline Derivatives. Monitor therapy
Tofacitinib: May enhance the bradycardic effect of Bradycardia-Causing Agents. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Test Interactions
May lead to false-positive aldosterone/renin ratio (ARR) (Funder 2016)
Adverse Reactions
>10%: Central nervous system: Drowsiness, insomnia
1% to 10%:
Cardiovascular: Atrioventricular block, bradycardia, cardiac conduction disturbance, cardiac failure, cold extremities, edema, hypotension, palpitations, peripheral vascular insufficiency, Raynaud's phenomenon
Central nervous system: Depression, dizziness, fatigue, sedation
<1%, postmarketing, and/or case reports: Abdominal distress, anorexia, behavioral changes, bloating, blurred vision, bronchospasm, cardiac arrhythmia, chest pain, confusion (especially in the elderly), constipation, cough, decreased libido, diaphoresis, diarrhea, dyspepsia, dyspnea, facial edema, flatulence, hallucination, headache, impotence, nasal congestion, nausea, nervousness, paresthesia, pruritus, skin rash, slurred speech, thrombocytopenia, tinnitus, transient alopecia, vomiting, weight gain, xeroderma, xerophthalmia, xerostomia
Warnings/Precautions
Concerns related to adverse events:
- Anaphylactic reactions: Use caution with history of severe anaphylaxis to allergens; patients taking beta-blockers may become more sensitive to repeated challenges. Treatment of anaphylaxis (eg, epinephrine) in patients taking beta-blockers may be ineffective or promote undesirable effects.
Disease-related concerns:
- Bronchospastic disease: In general, patients with bronchospastic disease should not receive beta-blockers; if used at all, should be used cautiously with close monitoring.
- Conduction abnormality: Consider preexisting conditions such as sick sinus syndrome before initiating.
- Diabetes: Use with caution in patients with diabetes mellitus; may potentiate hypoglycemia and/or mask signs and symptoms.
- Heart failure (HF): Use with caution in patients with compensated heart failure and monitor for a worsening of the condition (efficacy of nadolol in HF has not been demonstrated).
- Myasthenia gravis: Use with caution in patients with myasthenia gravis.
- Peripheral vascular disease (PVD) and Raynaud disease: Can precipitate or aggravate symptoms of arterial insufficiency in patients with PVD and Raynaud disease. Use with caution and monitor for progression of arterial obstruction.
- Pheochromocytoma (untreated): Adequate alpha-blockade is required prior to use of any beta-blocker.
- Prinzmetal variant angina: Beta-blockers without alpha1-adrenergic receptor blocking activity should be avoided in patients with Prinzmetal variant angina since unopposed alpha1-adrenergic receptors mediate coronary vasoconstriction and can worsen anginal symptoms (Mayer 1998).
- Psoriasis: Beta-blocker use has been associated with induction or exacerbation of psoriasis, but cause and effect have not been firmly established.
- Renal impairment: Use with caution in patients with renal impairment; dosage adjustments are required.
- Thyroid disease: May mask signs of hyperthyroidism (eg, tachycardia). If hyperthyroidism is suspected, carefully manage and monitor; abrupt withdrawal may exacerbate symptoms of hyperthyroidism or precipitate thyroid storm.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Bradycardia may be observed more frequently in elderly patients (>65 years of age); dosage reductions may be necessary.
Other warnings/precautions:
- Abrupt withdrawal: [US Boxed Warning]: Beta-blocker therapy should not be withdrawn abruptly (particularly in patients with CAD), but gradually tapered to avoid acute tachycardia, hypertension, and/or ischemia. Severe exacerbation of angina, ventricular arrhythmias, and myocardial infarction (MI) have been reported following abrupt withdrawal of beta-blocker therapy. Temporary but prompt resumption of beta-blocker therapy may be indicated with worsening of angina or acute coronary insufficiency.
- Major surgery: Chronic beta-blocker therapy should not be routinely withdrawn prior to major surgery.
Monitoring Parameters
Heart rate, blood pressure, signs/symptom of angina exacerbation when discontinued
Hypertension: The 2017 Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults (ACC/AHA [Whelton 2017]):
Confirmed hypertension and known CVD or 10-year ASCVD risk ≥10%: Target blood pressure <130/80 mm Hg is recommended.
Confirmed hypertension without markers of increased ASCVD risk: Target blood pressure <130/80 mm Hg may be reasonable.
Pregnancy
Pregnancy Considerations
Exposure to beta-blockers during pregnancy may increase the risk for adverse events in the neonate. If maternal use of a beta-blocker is needed, fetal growth should be monitored during pregnancy and the newborn should be monitored for 48 hours after delivery for bradycardia, hypoglycemia, and respiratory depression (ESC [Regitz-Zagrosek 2018]).
Chronic maternal hypertension is also associated with adverse events in the fetus/infant. Chronic maternal hypertension may increase the risk of birth defects, low birth weight, premature delivery, stillbirth, and neonatal death. Actual fetal/neonatal risks may be related to duration and severity of maternal hypertension. Untreated chronic hypertension may also increase the risks of adverse maternal outcomes, including gestational diabetes, preeclampsia, delivery complications, stroke, and myocardial infarction (ACOG 203 2019).
When treatment of chronic hypertension in pregnancy is indicated, agents other than nadolol are preferred (ACOG 203 2019; ESC [Regitz-Zagrosek 2018]; Magee 2014). Females with preexisting hypertension may continue their medication during pregnancy unless contraindications exist (ESC [Regitz-Zagrosek 2018])
Patient Education
What is this drug used for?
- It is used to treat high blood pressure.
- It is used to treat a type of long-term chest pain (stable angina) in some people.
- It may be given to you for other reasons. Talk with the doctor.
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Severe dizziness
- Passing out
- Chest pain
- Sensation of cold
- Slow heartbeat
- Heart problems like cough or shortness of breath that is new or worse, swelling of the ankles or legs, abnormal heartbeat, weight gain of more than five pounds in 24 hours, dizziness, or passing out.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.