Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule, Oral:
Dialyvite Omega-3 Concentrate: 600 mg
Lovaza: 1 g [contains soybean oil, tocopherol, dl-alpha]
Ocean Blue MiniCaps Omega-3: 350 mg [gluten free, lactose free, sugar free; contains fd&c red #40, fd&c yellow #10 (quinoline yellow)]
Omega Power: 1050 mg [gluten free, lactose free, sugar free; contains fd&c red #40, fd&c yellow #10 (quinoline yellow); vanilla flavor]
Omega-3 2100: 1050 mg [odorless; orange flavor]
Triklo: 1 g [DSC]
Vascepa: 0.5 g, 1 g
Generic: 300 mg, 500 mg, 1000 mg, 1 g
Capsule, Oral [preservative free]:
Fish Oil Concentrate: 1000 mg [gluten free, lactose free, milk free, no artificial color(s), no artificial flavor(s), no artificial sweetener, sodium free, starch free, sugar free, wheat free, yeast free]
Maximum Red Krill: 300 mg [gluten free; contains soybean oil]
Omega-3 Fish Oil Ex St: 880 mg [gluten free]
Salmon Oil-1000: 200 mg [corn free, rye free, starch free, sugar free, wheat free]
Sam-E.P.A.: 200-300 MG [dye free]
Sea-Omega: 1000 mg [cholesterol free, corn free, gluten free, milk derivatives/products, no artificial color(s), no artificial flavor(s), sodium free, starch free, sugar free, yeast free; contains soybeans (glycine max)]
Generic: 200 mg, 1000 mg, 1200 mg
Capsule Delayed Release, Oral:
Odorless Coated Fish Oil: 1000 mg [gluten free, lactose free, milk free, no artificial color(s), no artificial flavor(s), no artificial sweetener, starch free, sugar free, wheat free, yeast free]
Pro Nutrients Omega 3: 332.5 mg
Generic: 1000 mg
Tablet Chewable, Oral:
Omega-3 IQ: 240 mg [fruit flavor]
Pharmacology
Mechanism of Action
Reduction in the hepatic production of triglyceride-rich very low-density lipoproteins. Possible cellular mechanisms include inhibition of acyl CoA:1,2 diacylglycerol acyltransferase, increased hepatic mitochondrial and peroxisomal beta-oxidation, and a reduction in the hepatic synthesis of triglycerides. The mechanisms contributing to reduction of cardiovascular events are not completely understood but are likely multi-factorial (eg, increased eicosapentaenoic acid [EPA] composition from carotid plaques, increased circulating EPA/arachidonic acid ratio, inhibition of platelet aggregation).
Pharmacokinetics/Pharmacodynamics
Absorption
Omega-3-carboxylic acids: Directly absorbed in the small intestine. Administration with a high-fat meal results in an increased overall exposure of total and free baseline-adjusted EPA by ~140% and 80%, respectively, compared to fasting conditions; a 40% increase in AUC occurred for baseline-adjusted free DHA.
Icosapent ethyl: De-esterified to active metabolite (EPA) which is absorbed in the small intestine
Distribution
Vdss: EPA: ~88 L
Metabolism
EPA and DHA are mainly oxidized in the liver similar to fatty acids derived from dietary sources. EPA: minor via CYP-450
Time to Peak
Plasma:
Omega-3-carboxylic acids: Following repeat dosing with low-fat meals for ~2 weeks (steady state): EPA: 5 to 8 hours; DHA: 5 to 9 hours
Icosapent ethyl: EPA: ~5 hours
Half-Life Elimination
EPA: ~37 to 89 hours; DHA: ~46 hours
Protein Binding
EPA: >99%
Use in Specific Populations
Special Populations: Gender
Females tended to have more uptake of EPA into serum phospholipids than males. The clinical significance of this is unknown.
Use: Labeled Indications
Cardiovascular risk reduction with mild hypertriglyceridemia (Vascepa): As an adjunct to maximally-tolerated statin therapy to reduce the risk of myocardial infarction, stroke, coronary revascularization, and unstable angina requiring hospitalization in adult patients with triglyceride levels ≥150 mg/dL and either established cardiovascular disease or type 2 diabetes mellitus with ≥2 risk factors for cardiovascular disease.
Dietary supplement: As dietary supplements for patients at early risk of coronary artery disease.
Note: Recommendations from the American Heart Association (AHA) state that patients without documented coronary heart disease (CHD) should eat a variety of fish, preferably oily fish (eg, salmon), at least twice a week, or daily in patients with documented CHD (AHA [Kris-Etherton 2002]).
Hypertriglyceridemia (Lovaza and Vascepa): As an adjunct to diet to reduce triglyceride levels in adults with severe (≥500 mg/dL) hypertriglyceridemia.
Note: The Endocrine Society recommends that omega-3 fatty acids may be considered for triglyceride levels >1,000 mg/dL and may be used alone or in combination with HMG-CoA reductase inhibitors (Berglund 2012). A number of OTC formulations containing omega-3 fatty acids are marketed as nutritional supplements; these do not have FDA-approved indications and may not contain the same amounts of the active ingredient.
Use: Off Label
IgA nephropathybyes
Data from a randomized, open-label, parallel-group clinical trial support the use of omega-3 fatty acids Lovaza in the treatment (ie, slowing rate of renal function loss) of IgA nephropathy Donadio 2001. A more recent meta-analysis does not confirm the efficacy for this indication, though it may likely be used for this indication Liu 2012. Additional trials may be necessary to further define the role of omega-3 fatty acids in the treatment of patients with IgA nephropathy.
Based on the Caring for Australasians with Renal Impairment guidelines early and prolonged treatment with fish oil may retard the rate of decline in renal function in adults with progressive IgA nephropathy; optimal dosing has yet to be established CARI [Harris 2006]. Routine use is currently not recommended (Laville 2004).
Contraindications
Hypersensitivity (eg, anaphylactic reaction) to omega-3 fatty acids or any component of formulation.
Dosage and Administration
Dosing: Adult
Cardiovascular risk reduction with mild hypertriglyceridemia (Vascepa) (adjunctive agent): Note: Consider in addition to maximally-tolerated statin therapy in patients with triglyceride levels ≥150 mg/dL and either established cardiovascular disease or type 2 diabetes mellitus with ≥2 risk factors for cardiovascular disease.
Oral: 2 g twice daily with meals (Bhatt 2019).
Hypertriglyceridemia: Oral:
Lovaza: 4 g (4 capsules) once daily or 2 g (2 capsules) twice daily.
Vascepa: 2 g (2 [1 g] capsules or 4 [0.5 g] capsules) twice daily with meals.
IgA nephropathy (off-label use): Oral: Lovaza: 4 g (4 capsules) once daily (Donadio 2001).
Dosing: Geriatric
Refer to adult dosing.
Administration
Lovaza: Administer with or without food. Administer whole; do not break, crush, dissolve, or chew.
Vascepa: Administer with meals. Administer whole; do not break, crush, dissolve, or chew.
Dietary Considerations
Dietary modification is important in the control of severe hypertriglyceridemia. Maintain standard cholesterol-lowering diet during therapy.
Storage
Lovaza: Store at 25°C (77°F); excursions are permitted to 15°C to 30°C (59°F to 86°F); do not freeze.
Vascepa: Store at 20°C to 25°C (68°F to 77°F); excursions are permitted to 15°C to 30°C (59°F to 86°F).
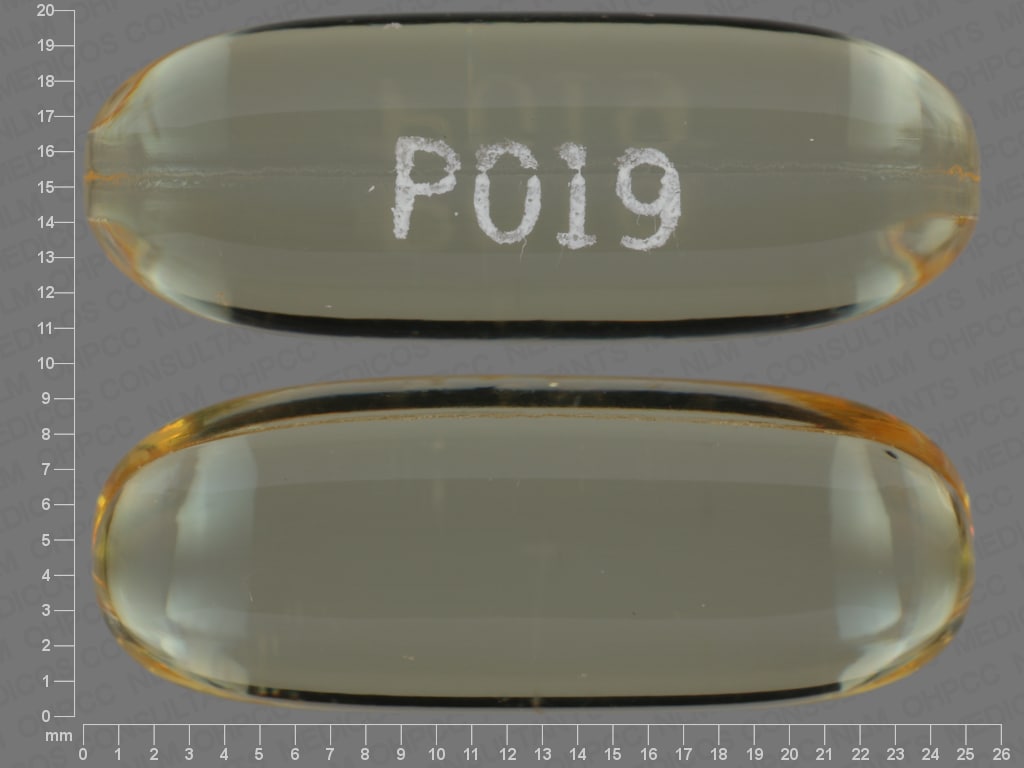
Omega-3 Fatty Acids Images
Drug Interactions
Agents with Antiplatelet Properties (e.g., P2Y12 inhibitors, NSAIDs, SSRIs, etc.): Omega-3 Fatty Acids may enhance the antiplatelet effect of Agents with Antiplatelet Properties. Monitor therapy
Anticoagulants: Omega-3 Fatty Acids may enhance the anticoagulant effect of Anticoagulants. Monitor therapy
Ibrutinib: Omega-3 Fatty Acids may enhance the antiplatelet effect of Ibrutinib. Monitor therapy
Adverse Reactions
>10%: Gastrointestinal: Diarrhea (7% to 15%)
1% to 10%:
Gastrointestinal: Nausea (4% to 6%), abdominal pain (3% to 5%), dysgeusia (4%), eructation (3% to 4%), dyspepsia (3%)
Neuromuscular & skeletal: Arthralgia (2%)
Frequency not defined:
Central nervous system: Fatigue
Dermatologic: Pruritus, skin rash
Endocrine & metabolic: Increased LDL cholesterol
Gastrointestinal: Abdominal distension, constipation, flatulence, gastrointestinal disease, vomiting
Hematologic & oncologic: Prolonged bleeding time
Hepatic: Increased serum alanine aminotransferase, increased serum aspartate aminotransferase
Respiratory: Nasopharyngitis, oropharyngeal pain
<1%, postmarketing, and/or case reports: Anaphylaxis, bleeding tendency disorder, cardiac arrhythmia, urticaria
Warnings/Precautions
Concerns related to adverse effects:
- Bleeding: Bleeding, including serious events, has been reported; risk may be increased with concomitant anticoagulant/antiplatelet use. Prolongation of bleeding time not exceeding normal limits has also been observed; use with caution in patients with coagulopathy. Monitor for signs and symptoms of bleeding.
- Fish allergy: Use with caution in patients with known allergy or sensitivity to fish and/or shellfish.
- Hepatic effects: ALT may increase without concurrent AST increase; periodically monitor hepatic transaminases in patients with hepatic impairment.
- Lipid effects: May increase LDL levels; periodically monitor LDL levels.
Disease-related concerns:
- Atrial fibrillation: Atrial fibrillation (AF) or flutter requiring hospitalization may occur; risk increased in patients with a history of AF or flutter and within the first 2 to 3 months of therapy.
- Conditions associated with abnormal lipids: Manage concurrent conditions (eg, diabetes, hypothyroidism, excessive alcohol intake) that may contribute to lipid abnormalities.
Other warnings/precautions:
- Appropriate use: Should be used as an adjunct to diet therapy and exercise. Secondary causes of hyperlipidemia should be ruled out prior to therapy. The effect, if any, of omega-3 fatty acids on the risk of pancreatitis or cardiovascular mortality and morbidity in patients with severe hypertriglyceridemia is not known.
Monitoring Parameters
Triglycerides and other lipids (LDL-C) should be monitored at baseline and periodically. In patients with hepatic impairment, monitor hepatic transaminase levels, particularly ALT, periodically. Signs/symptoms of bleeding.
2013 ACC/AHA Blood Cholesterol Guideline recommendations (Stone 2013): Consider evaluation for GI disturbances and skin changes during therapy.
Pregnancy
Pregnancy Considerations
Adequate intake of omega-3 fatty acids is recommended during pregnancy (IOM 2005; Nordgren 2017). Maternal use of supplements or dietary consumption of omega-3 fatty acids (containing eicosapentaenoic acid and docosahexaenoic acid) influences fetal concentrations (Büyükuslu 2017; Coletta 2010; Miles 2011).
Triglyceride concentrations increase during pregnancy as required for normal fetal development. When increases are greater than expected, supervised dietary interventions that include omega-3 fatty acids may be initiated. In women who develop very severe hypertriglyceridemia and are at risk for pancreatitis, use of prescription omega-3 fatty acid products may be considered (Avis 2009; Berglund 2012; Jacobson 2015; Wong 2015).
Patient Education
What is this drug used for?
- It is used to lower triglycerides.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Burping
- Change in taste
- Nausea
- Abdominal pain
- Joint pain
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Abnormal heartbeat
- Bruising
- Bleeding
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.