Boxed Warning
Experienced physician:
Physicians planning to use penicillamine should thoroughly familiarize themselves with its toxicity, special dosage considerations, and therapeutic benefits. Penicillamine should never be used casually. Each patient should remain constantly under the close supervision of the physician.
Toxicity symptoms:
Patients should be warned to report promptly any symptoms suggesting toxicity.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
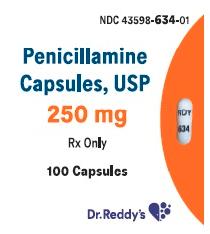
Capsule, Oral:
Cuprimine: 250 mg [contains fd&c yellow #10 (quinoline yellow)]
Generic: 250 mg
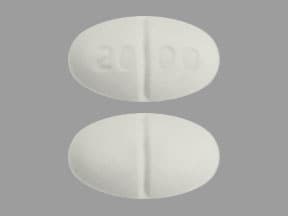
Tablet, Oral:
D-Penamine: 125 mg [DSC] [gluten free]
Depen Titratabs: 250 mg [scored]
Generic: 250 mg
Pharmacology
Mechanism of Action
Chelates with lead, copper, mercury and other heavy metals to form stable, soluble complexes that are excreted in urine; depresses circulating IgM rheumatoid factor, depresses T-cell but not B-cell activity; combines with cystine to form a compound which is more soluble, thus cystine calculi are prevented
Pharmacokinetics/Pharmacodynamics
Absorption
Rapid but incomplete (40% to 70%); reduced by food, antacids, and iron
Metabolism
Hepatic (small amounts metabolized to s-methyl-d-penicillamine)
Excretion
Urine (primarily as disulfides)
Onset of Action
Rheumatoid arthritis: 2 to 3 months; Wilson disease: 1 to 3 months
Time to Peak
Plasma: 1 to 3 hours
Half-Life Elimination
1.7 to 7 hours (Roberts 2008); large variations exist and a slow elimination phase lasting 4 to 6 days may occur after prolonged treatment has been stopped
Protein Binding
>80% to albumin and ceruloplasmin
Use: Labeled Indications
Treatment of Wilson's disease, cystinuria
Contraindications
Renal insufficiency (in patients with rheumatoid arthritis); patients with previous penicillamine-related aplastic anemia or agranulocytosis; breast-feeding; pregnancy (in patients with rheumatoid arthritis)
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to penicillamine or any component of the formulation; use in patients with chronic lead poisoning who have radiographic evidence of lead-containing substances in the GI tract; pregnancy (in patients with chronic lead poisoning); concomitant use with gold therapy, antimalarial or cytotoxic drugs, oxyphenbutazone or phenylbutazone
Dosage and Administration
Dosing: Adult
Note: Dose reduction to 250 mg/day may be considered prior to surgical procedures (including prior to cesarean delivery in pregnant patients with Wilson disease). May resume normal recommended dosing postoperatively once wound healing is complete. Penicillamine administration increases requirement for pyridoxine. Patients may require a daily supplement of pyridoxine.
Cystinuria: Oral: 1 to 4 g/day in 4 divided doses; usual dose: 2 g/day; initiation of therapy at 250 mg/day with gradual upward titration may reduce the risk of unwanted effects. Note: Adjust dose to limit cystine excretion to 100 to 200 mg/day (<100 mg/day with history of stone formation).
Wilson disease: Oral: Note: Dose that results in an initial 24-hour urinary copper excretion >2 mg/day should be continued for ~3 months; maintenance dose defined by amount resulting in <10 mcg serum free copper/dL.
To increase tolerability, therapy may be initiated at 250 to 500 mg/day then titrated upward in 250 mg increments every 4 to 7 days; usual maintenance dose: 750 mg to 1 g/day in 2 divided doses; maximum: 1 to 1.5 g/day in 2 to 4 divided doses (AASLD [Roberts 2008]).
Pregnancy: Decrease the dose to the minimum effective dose; consider reducing by 25% to 50% of the prepregnancy dose (AASLD [Roberts 2008]; Dathe 2016; EASL 2012).
Manufacturer's labeling: Dosing in the prescribing information may not reflect current clinical practice. 750 mg to 1.5 g/day in divided doses; maximum dose: 2 g/day. Note: Limit daily dose to 750 mg/day in pregnant women; if planned cesarean delivery, limit dose to 250 mg/day during the last 6 weeks of pregnancy and postoperatively until wound healing is complete.
Dosing: Geriatric
Therapy should be initiated at low end of dosing range and titrated upward cautiously. Refer to adult dosing.
Dosing: Pediatric
Note: Penicillamine administration increases requirement for pyridoxine. Patients may require a daily supplement of pyridoxine. A dose reduction (to 250 mg/day in adults) may be considered prior to surgical procedures. May resume normal recommended dosing postoperatively once wound healing is complete.
Wilson disease:
Diagnosis (adjunct): Penicillamine Challenge Test: Limited data available: Children ≥2 years and Adolescents: Oral: 500 mg/dose for 2 doses; administer first immediately prior to a 24-hour urine collection and repeat 12 hours later. Urinary copper excretion >1,600 mcg copper/24 hour (>25 µmol/24 hours) is consistent with Wilson disease (AASLD [Roberts 2008]; EASL 2012; Martins da Costa 1992; Müller 2007).
Treatment: Children and Adolescents: Oral: 20 mg/kg/day in 2 to 3 divided doses, round off to the nearest 250 mg dose; reduce dose by 25% when clinically stable; adult maximum daily dose: 1,500 mg/day (AASLD [Roberts 2008]; EASL 2012)
Cystinuria: Children and Adolescents: Oral: 20 to 40 mg/kg/day in 4 divided doses; maximum daily dose: 40 mg/kg/day (DeBerardinis 2008); adult maximum daily dose: 4,000 mg/day. Manufacturer recommends if 4 equal doses are not possible, give the larger portion at bedtime and suggests dose should be adjusted to limit cysteine excretion to <100 to 200 mg/day (<100 mg/day with history of stone formation and/or pain). A retrospective chart review of 11 patients (age range: 1.2 to 12.5 years) with urolithiasis and high urinary cysteine receiving long-term penicillamine (~3 to 18 years) suggests that gradual initiation of penicillamine effectively lowers urinary cysteine concentrations and may limit toxicity associated with treatment. Therapy was initiated at 5 mg/kg/day and increased weekly by 5 mg/kg/day to a final dose of 20 mg/kg/day; five patients required further increases up to 40 mg/kg/day. Urinary cysteine concentrations decreased 5% to 81% while on treatment. Five patients did not reach the goal urinary cysteine concentration of <1,200 micromolar. Six patients experienced acute stone crisis or had evidence of new stone formation on ultrasound; however, in all cases this was during periods of noncompliance to therapy (DeBerardinis 2008).
Lead poisoning: Note: For the treatment of high blood lead levels in children, the CDC recommends chelation treatment when blood lead levels are >45 mcg/dL (ACCLPP 2012; CDC 2002). AAP considers penicillamine a 3rd line agent for children when blood lead levels are >45 mcg/dL and <70 mcg/dL; children with blood lead levels >70 mcg/dL or symptomatic lead poisoning should be treated with parenteral agents (AAP 2005).
Children and Adolescents: Limited data available, optimal dose not defined: Oral: Initial: 10 mg/kg/day divided twice daily for 2 weeks increase dose to 25 to 40 mg/kg/day (Kliegman 2016); increasing the dose over a few weeks has been suggested to improve tolerability (Shannon 1998). A reduced dosage of 15 mg/kg/day in 2 divided doses has been shown to be effective in the treatment of mild to moderate lead poisoning (blood lead concentration 20 to 40 mcg/dL) with a reduction in adverse effects (Shannon 2000); lower doses (10 to 15 mg/kg/day for 4 to 12 weeks) has also been suggested for treating lead concentrations of 45 to 69 mcg/dL (Chandran 2010).
Extemporaneously Prepared
A 50 mg/mL oral suspension may be made with capsules. Mix the contents of sixty 250 mg capsules with 3 g carboxymethylcellulose, 150 g sucrose, 300 mg citric acid, and parabens (methylparaben 120 mg, propylparaben 12 mg). Add quantity of propylene glycol sufficient to make 100 mL, then add quantity of purified water sufficient to make 300 mL. Cherry flavor may be added. Label "shake well" and "refrigerate". Stable for 30 days refrigerated.
DeCastro FJ, Jaeger RQ, and Rolfe UT, "An Extemporaneously Prepared Penicillamine Suspension Used to Treat Lead Intoxication," Hosp Pharm, 1977, 2:446-8.
Administration
Oral: Doses ≤500 mg may be administered as a single dose; doses >500 mg should be administered in divided doses. For patients who have difficulty swallowing, the contents of the capsules may be administered in 15 to 30 mL of chilled puréed fruit or fruit juice within 5 minutes of preparation. Administer on an empty stomach (1 hour before or 2 hours after meals) and at least 1 hour apart from other drugs, milk, antacids, iron-containing products, and zinc-containing products.
Cystinuria: If administering 4 equal doses is not feasible, administer the larger dose at bedtime. Patients should drink about one pint of fluid at bedtime and another pint during the night.
Dietary Considerations
Should be taken at least 1 hour before or 2 hours after meals on an empty stomach (Note: Canadian labeling recommends administration at least 2 hours before meals in patients with lead poisoning). Pyridoxine supplementation is recommended. Patients with Wilson's disease should receive 25 to 50 mg/day of pyridoxine (Roberts, 2008); a multivitamin (without copper) may also be considered. Patients with cystinuria or patients with rheumatoid arthritis and impaired nutritional intake should receive 25 mg/day of pyridoxine. For Wilson's disease, decrease copper in diet to <1 to 2 mg/day and omit chocolate, nuts, shellfish, mushrooms, liver, raisins, broccoli, copper-enriched cereal, multivitamins with copper, and molasses. May consider short courses of iron supplementation if dietary modifications (eg, low copper diet in Wilson’s disease, low methionine diet in cystinuria) results in iron deficiency; pediatric patients and menstruating women may be particularly susceptible to iron deficiency. Allow at least 1 hour between administration of iron supplementation and penicillamine as iron may decrease drug absorption. For cystinuria, increase daily fluid intake, including 1 pint (~500 mL) of fluid prior to bedtime and 1 additional pint during the night. For lead poisoning, decrease calcium in diet.
Storage
Store in tight, well-closed containers.
PenicillAMINE Images
Drug Interactions
Digoxin: PenicillAMINE may decrease the serum concentration of Digoxin. Monitor therapy
Gold Sodium Thiomalate: May enhance the adverse/toxic effect of PenicillAMINE. Specifically, this combination may increase the risk for serious hematologic and/or renal adverse reactions. Avoid combination
Polyvalent Cation Containing Products: May decrease the serum concentration of PenicillAMINE. Management: Separate the administration of penicillamine and oral polyvalent cation containing products by at least 1 hour. Consider therapy modification
Adverse Reactions
Frequency may vary by indication.
>10%:
Gastrointestinal: Diarrhea (17%), dysgeusia (12%)
1% to 10%:
Dermatologic: Skin rash (early and late: 5%)
Genitourinary: Proteinuria (6%)
Hematologic & oncologic: Thrombocytopenia (4%), leukopenia (2%)
Frequency not defined.
Cardiovascular: Local thrombophlebitis, vasculitis (including renal vasculitis)
Central nervous system: Anxiety, agitation, dystonia, Guillain-Barre syndrome, hyperpyrexia, myasthenia (including extraocular muscles), myasthenia gravis, neurological deterioration, neuropathy, psychiatric disturbance
Dermatologic: Alopecia, cheilosis, exfoliative dermatitis, fragile skin (friability increased), lichen planus, papule (white papules at venipuncture and surgical sites), pemphigus, pruritus, skin atrophy (anetoderma), toxic epidermal necrolysis, urticaria, wrinkling of skin (excessive), yellow nail syndrome
Endocrine & metabolic: Hypoglycemia, increased lactate dehydrogenase, thyroiditis
Gastrointestinal: Anorexia, epigastric pain, glossitis, nausea, oral mucosa ulcer, pancreatitis, peptic ulcer (reactivation), stomatitis (gingivostomatitis), vomiting
Genitourinary: Breast disease (mammary hyperplasia), Goodpasture's syndrome, hematuria, nephrotic syndrome
Hematologic & oncologic: Agranulocytosis, aplastic anemia, change in platelet count (increase), eosinophilia, hemolytic anemia, increased monocytes, leukocytosis, lymphadenopathy, positive ANA titer, pure red cell aplasia, sideroblastic anemia, thrombotic thrombocytopenic purpura
Hepatic: Increased serum alkaline phosphatase, hepatic failure, intrahepatic cholestasis, toxic hepatitis
Neuromuscular & skeletal: Arthralgia, connective tissue disease (elastosis perforans serpiginosa), dermatomyositis, lupus-like syndrome, polyarthralgia (migratory, often with objective synovitis), polymyositis
Ophthalmic: Blepharoptosis, diplopia, optic neuritis, visual disturbance
Otic: Tinnitus
Renal: Renal failure
Respiratory: Asthma, bronchiolitis obliterans, hypersensitivity pneumonitis, interstitial pneumonitis, pulmonary fibrosis
Miscellaneous: Fever
Warnings/Precautions
Concerns related to adverse effects:
- Allergic reactions: Approximately 33% of patients will experience an allergic reaction. Rash may occur early (more commonly) or late in therapy; early-onset rash typically resolves within days of discontinuation of therapy and does not recur upon rechallenge with reduced dose; discontinue therapy for late-onset rash (eg, after >6 months) and do not rechallenge; rash typically recurs with rechallenge. Discontinue therapy for skin reactions accompanied by lymphadenopathy, fever, arthralgia, or other allergic reactions.
- Bronchiolitis obliterans: Has been reported rarely with use; instruct patients to report pulmonary symptoms (eg, unexplained wheezing or cough, exertional dyspnea) and consider pulmonary function testing in such patients.
- Dermatologic: Penicillamine increases the amount of soluble collagen; may increase skin friability, particularly at sites subject to pressure or trauma (eg, knees, elbows shoulders). Purpuric areas with localized bleeding (if skin is broken) or vesicles with dark blood may be observed. Effects are considered localized and do not necessitate discontinuation of therapy; may not recur with dose reduction. Macular cutaneous eruptions are sometimes observed in conjunction with drug fever, usually 2 -3 weeks after therapy initiation. Dose reduction may be considered prior to surgical procedures. May resume normal recommended dosing postoperatively once wound healing is complete.
- Drug fever: Drug fever may be observed, usually 2-3 weeks after therapy initiation. Discontinue use in patients with rheumatoid arthritis, Wilson's disease, or cystinuria who develop a marked febrile response. Consider alternative therapy for patients with rheumatoid arthritis due to high incidence of fever reoccurrence with penicillamine rechallenge. May resume therapy at a reduced dose in Wilson's disease or cystinuria upon resolution of fever; dose should then be gradually titrated to effective dose.
- Gastrointestinal: Taste alteration may occur (rare in Wilson's disease); usually self-limited with continued therapy, however may last ≥2 months and result in total loss of taste. Oral ulceration (eg, stomatitis) may occur; typically recurs on rechallenge but often resolves with dose reduction. Other dose-related lesions (eg, glossitis, gingivostomatitis) have been observed with use and may require therapy discontinuation.
- Goodpasture's syndrome: Penicillamine has been associated with fatalities due to Goodpasture's syndrome. Discontinue therapy immediately in patients with abnormal urinary findings in association with hemoptysis and pulmonary infiltrates on chest x-ray.
- Hematologic toxicities: Penicillamine has been associated with fatalities due to agranulocytosis, aplastic anemia, and thrombocytopenia. Discontinue therapy for WBC <3500/mm3. Withhold therapy at least temporarily for platelet counts <100,000/mm3 or a progressive fall in WBC or platelets in 3 successive determinations, even though values may remain within the normal range. Monitor for signs/symptoms of leukopenia and thrombocytopenia.
- Hepatotoxicity: Monitor liver function tests periodically due to rare reports of intrahepatic cholestasis or toxic hepatitis. More frequent monitoring is required during the first year of therapy in patients with Wilson’s disease.
- Lupus erythematosus-like syndrome: May be observed in some patients; positive antinuclear antibody (ANA) test does not necessitate therapy discontinuation but should alert clinicians of possible future development of lupus erythematosus-like syndrome.
- Pemphigus: May occur early or late in therapy; discontinue use with suspicion of pemphigus. May treat with high-dose corticosteroids alone, or in conjunction with an immunosuppressant; treatment duration can range from weeks to >1 year.
- Penicillin cross-sensitivity: Patients with a penicillin allergy may theoretically have cross-sensitivity to penicillamine; however, the possibility has been eliminated now that penicillamine is produced synthetically and no longer contains trace amounts of penicillin.
- Proteinuria/hematuria: Proteinuria or hematuria may develop; monitor for membranous glomerulopathy which can lead to nephrotic syndrome. In rheumatoid arthritis patients, discontinue if gross hematuria or persistent microscopic hematuria develop and discontinue therapy or reduce dose for proteinuria that is either >1 g/day or progressively increasing. Dose reduction may lead to resolution of proteinuria.
- Myasthenia gravis: Penicillamine has been associated with myasthenic syndrome, and in some cases, progression to myasthenia gravis. Resolution of symptoms has been observed in most cases following discontinuation of therapy.
- Toxicity symptoms: [US Boxed Warning]: Patients should be warned to report promptly any symptoms suggesting toxicity (fever, sore throat, chills, bruising, or bleeding); toxicity may be dose related.
Disease-related concerns:
- Cystinuria: Continue treatment on a daily basis; interruptions of even a few days have been followed by hypersensitivity with reinstitution of therapy. Patients should receive pyridoxine supplementation (25 mg/day).
- Lead poisoning: Investigate, identify, and remove sources of lead exposure and confirm lead-containing substances are absent from the GI tract prior to initiating therapy. Do not permit patients to re-enter the contaminated environment until lead abatement has been completed. Penicillamine is considered to be a third-line agent for the treatment of lead poisoning in children due to the overall toxicity associated with its use (AAP, 2005; Chandran, 2010); penicillamine should only be used when unacceptable reactions have occurred with edetate CALCIUM disodium and succimer. Primary care providers should consult experts in the chemotherapy of lead toxicity before using chelation drug therapy.
- Rheumatoid arthritis: Patients with rheumatoid arthritis and impaired nutrition should receive pyridoxine supplementation (25 mg/day).
- Wilson's disease: Continue treatment on a daily basis; interruptions of even a few days have been followed by hypersensitivity with reinstitution of therapy. Worsening of neurologic symptoms may occur during initiation of therapy however discontinuation of therapy is not recommended; may consider concomitant use of short term dimercaprol in patients whose symptoms continue to worsen 1 month following therapy initiation. Patients should receive pyridoxine supplementation (25-50 mg/day; Roberts, 2008).
Concurrent drug therapy issues:
- Hematopoietic-depressant drugs: Use with caution in patients on other hematopoietic-depressant drugs (eg, gold, immunosuppressants, antimalarials, phenylbutazone; Canadian labeling contraindicates concomitant use with these agents); hematologic and renal adverse reactions are similar.
Special populations:
- Elderly: Use with caution in the elderly; may be more susceptible to skin rash and/or taste alterations.
Other warnings/precautions:
- Experienced physician: [US Boxed Warning]: Should be administered under the close supervision of a physician familiar with the toxicity and dosage considerations.
Monitoring Parameters
Urinalysis, CBC with differential, platelet count, skin, lymph nodes, and body temperature twice weekly during the first month of therapy, then every 2 weeks for 5 months, then monthly; LFTs every 6 months; signs/symptoms of hypersensitivity
Cystinuria: Urinary cystine, annual X-ray for renal stones
Lead poisoning: Serum lead concentration (baseline and 7-21 days after completing chelation therapy); hemoglobin or hematocrit, iron status, free erythrocyte protoporphyrin or zinc protoporphyrin; neurodevelopmental changes
Wilson's disease: Serum non-ceruloplasmin bound copper, 24-hour urinary copper excretion, LFTs every 3 months (at least) during the first year of treatment; periodic ophthalmic exam
Urinalysis: Monitor for proteinuria and hematuria. A quantitative 24-hour urine protein at 1- to 2-week intervals initially (first 2-3 months) is recommended if proteinuria develops.
Pregnancy
Pregnancy Considerations
Penicillamine-disulphide and cysteine-penicillamine were present in the urine of a newborn following maternal use of penicillamine throughout pregnancy for the treatment of cystinuria (Crawhall 1967).
Birth defects, including congenital cutix laxa and associated defects, have been reported in infants following penicillamine exposure during pregnancy; however, outcome information related to use in pregnancy is limited (AASLD [Roberts 2008]; Dathe 2016).
Continued treatment of Wilson disease during pregnancy protects the mother against relapse. Discontinuation has detrimental maternal and fetal effects. Penicillamine should be decreased to the minimum effective dose during pregnancy to limit fetal exposure during the first trimester, to prevent fetal copper deficiency, and to help promote maternal wound healing if cesarean delivery is planned. Doses may be 25% to 50% of the prepregnancy dose. Close monitoring is recommended (AASLD [Roberts 2008]; EASL 2012).
Use for the treatment of rheumatoid arthritis during pregnancy is contraindicated. Penicillamine should be used for the treatment of cystinuria only if the possible benefits to the mother outweigh the potential risks to the fetus.
Patient Education
What is this drug used for?
- It is used to treat Wilson's disease.
- It is used to get rid of a protein called cystine from the body.
- It is used to treat rheumatoid arthritis.
- It may be given for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Nausea
- Vomiting
- Diarrhea
- Change in taste
- Abdominal pain
- Mouth irritation
- Mouth sores
- Lack of appetite
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Infection
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe or persistent bleeding
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain
- Lupus like rash on the cheeks or other body parts, sunburn easy, muscle or joint pain, chest pain or shortness of breath, or swelling in the arms or legs
- Severe pulmonary disorder like lung or breathing problems like difficulty breathing, shortness of breath, or a cough that is new or worse
- Kidney stone like back pain, abdominal pain, or blood in the urine
- Severe loss of strength and energy
- Skin changes
- Swollen glands
- Muscle weakness
- Burning or numbness feeling
- Noise or ringing in the ears
- Mood changes
- Tremors
- Trouble moving
- Rigidity
- Joint pain
- Vision changes
- Eyelid droop
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.