Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Tablet, Oral, as calcium [strength expressed as base]:
Livalo: 1 mg, 2 mg, 4 mg
Tablet, Oral, as magnesium [strength expressed as base]:
Zypitamag: 1 mg, 2 mg, 4 mg
Pharmacology
Mechanism of Action
Inhibitor of 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase, the rate-limiting enzyme in cholesterol synthesis (reduces the production of mevalonic acid from HMG-CoA); this then results in a compensatory increase in the expression of LDL receptors on hepatocyte membranes and a stimulation of LDL catabolism. In addition to the ability of HMG-CoA reductase inhibitors to decrease levels of high-sensitivity C-reactive protein (hsCRP), they also possess pleiotropic properties including improved endothelial function, reduced inflammation at the site of the coronary plaque, inhibition of platelet aggregation, and anticoagulant effects (de Denus 2002; Ray 2005).
Pharmacokinetics/Pharmacodynamics
Distribution
Vd: ~148 L
Metabolism
Hepatic, via UGT1A3 and UGT2B7; minimal metabolism via CYP2C9 and CYP2C8
Excretion
Feces (79%); urine (15%)
Time to Peak
~1 hour
Half-Life Elimination
~12 hours
Protein Binding
>99%, primarily to albumin and alpha 1-acid glycoprotein
Use in Specific Populations
Special Populations: Renal Function Impairment
Cmax and AUC were 60% and 102% higher in patients with GFR 30 to 59 mL/minute/1.73 m2 and 40% and 86% higher in patients with ESRD on hemodialysis, respectively.
Special Populations: Hepatic Function Impairment
Half-life was 15 and 10 hours for patients with moderate and mild impairment, respectively.
Special Populations: Elderly
Cmax and AUC were 10% and 30% higher, respectively, in elderly patients compared with younger patients.
Special Populations: Gender
Cmax and AUC were 60% and 54% higher, respectively, in women compared with men.
Special Populations: Race
Cmax and AUC were 21% and 5% lower, respectively, in black patients compared with white patients.
Use: Labeled Indications
Primary hyperlipidemia and mixed dyslipidemia: As an adjunctive therapy to diet to reduce elevated total cholesterol, low-density lipoprotein cholesterol (LDL-C), apolipoprotein B (apo B), and triglycerides (TG), and to increase high-density lipoprotein cholesterol (HDL-C) in adults with primary hyperlipidemia or mixed dyslipidemia.
Heterozygous familial hypercholesterolemia: As an adjunctive therapy to diet to reduce elevated total cholesterol, LDL-C, and apo B in children and adolescents ≥8 years of age.
Use: Off Label
Cardiac risk reduction for noncardiac surgery (perioperative therapy)yes
Based on the 2014 American College of Cardiology/American Heart Association (ACC/AHA) guidelines on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery, perioperative initiation of statins is reasonable for patients undergoing vascular surgery and may be considered in patients with clinical indications according to guideline-directed medical therapy who are undergoing elevated risk procedures. In patients undergoing non-cardiac surgery who are currently receiving a statin, the statin should be continued.
Noncardioembolic stroke/Transient ischemic attack (secondary prevention)yes
Based on the American Heart Association/American Stroke Association (AHA/ASA) guidelines for the prevention of stroke in patients with stroke and transient ischemic attack, statin therapy with intensive lipid-lowering effects is recommended to reduce the risk of recurrent stroke and future cardiovascular events in patients with ischemic stroke or TIA presumed to be of atherosclerotic origin who have an LDL-C concentration ≥100 mg/dL (with or without evidence for other clinical atherosclerotic cardiovascular disease [ASCVD]) or who have an LDL-C concentration <100 mg/dL (without evidence for other clinical ASCVD).
Primary and secondary prevention of atherosclerotic cardiovascular disease (ASCVD)yes
Based on the American College of Cardiology/American Heart Association (ACC/AHA) Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults and the National Lipid Association Recommendations for Patient-Centered Management of Dyslipidemia, pitavastatin given for primary and secondary prevention of atherosclerotic cardiovascular disease (ASCVD) is effective and recommended in the management of this condition. Based on the US Preventive Services Task Force (USPSTF) recommendation statement on Statin Use for the Primary Prevention of Cardiovascular Disease (CVD) in Adults, initiation of low to moderate dose statin therapy is recommended in adults 40 to 75 years without a history of CVD who have ≥1 CVD risk factors (dyslipidemia, diabetes, hypertension, or smoking) and a calculated 10-year CVD event risk of ≥10%. Based on the American Heart Association (AHA) scientific statement for the secondary prevention after coronary artery bypass graft surgery, statin therapy (unless contraindicated) is recommended for all coronary artery bypass graft (CABG) surgery patients to help maintain long-term graft patency and help obtain the highest level of physical health and quality of life.
Contraindications
Hypersensitivity to pitavastatin or any component of the formulation; active liver disease, including unexplained persistent elevations of hepatic transaminase levels; pregnancy; lactation; coadministration with cyclosporine
Dosage and Administration
Dosing: Adult
Note: Individualize dose according to the baseline LDL-cholesterol levels, recommended goal of therapy, and patient response.
Primary hyperlipidemia and mixed dyslipidemia: Oral: Initial: 2 mg once daily; 4 weeks after initiation or upon titration, analyze lipid levels and adjust dose accordingly; Maintenance: 1 to 4 mg once daily; maximum: 4 mg/day.
Prevention of cardiovascular disease/reduce the risk of atherosclerotic cardiovascular disease (off-label use): Oral:
ACC/AHA Blood Cholesterol Guideline recommendations (ACC/AHA [Grundy 2018]; ACC/AHA [Stone 2013]):
Note: When choosing to initiate therapy and selecting dose-intensity, consider atherosclerotic cardiovascular disease (ASCVD) risk, risk-enhancing factors, possibility for side effects, and drug interactions.
Primary prevention:
LDL-C ≥190 mg/dL and age 20 to 75 years: High-intensity therapy necessary; use alternate statin therapy (eg, atorvastatin or rosuvastatin)
Diabetes, age 40 to 75 years and an estimated 10-year ASCVD risk <7.5%: Moderate-intensity therapy: 2 to 4 mg once daily
Diabetes, age 40 to 75 years, and an estimated 10-year ASCVD risk ≥7.5%: High-intensity therapy necessary; use alternate statin therapy (eg, atorvastatin or rosuvastatin)
LDL-C 70 to 189 mg/dL, age 40 to 75 years, and an estimated 10-year ASCVD risk ≥7.5%: Moderate to high-intensity therapy: 2 to 4 mg once daily or consider using high-intensity statin therapy (eg, atorvastatin or rosuvastatin)
Secondary prevention:
Patient has clinical ASCVD (eg, coronary heart disease, stroke/TIA, or peripheral arterial disease presumed to be of atherosclerotic origin) or is post-CABG (AHA [Kulik 2015]) and:
Age ≤75 years: High-intensity therapy necessary; use alternate statin therapy (eg, atorvastatin or rosuvastatin)
Age >75 years: Moderate- to high-intensity therapy: 2 to 4 mg once daily or consider using high-intensity statin therapy (eg, atorvastatin or rosuvastatin); if moderate-intensity therapy is started and tolerated, increase to a high-intensity statin therapy within 3 months (Rosenson 2019).
US Preventive Services Task Force Recommendations (USPSTF 2016): Age 40 to 75 years, no history of CVD, with ≥1 CVD risk factor (dyslipidemia, diabetes, hypertension, or smoking), and calculated 10-year CVD event risk of ≥10%:
Primary prevention:
Low-intensity therapy: 1 mg once daily
Moderate-intensity therapy: 2 to 4 mg once daily
Note: These recommendations do not pertain to patients with very high cholesterol levels (eg, LDL >190 mg/dL, familial hypercholesterolemia; were excluded from primary prevention trials); use clinical judgment in the treatment of these patients. In patients with a calculated 10-year CVD event risk of 7.5% to 10%, statin use may be considered based on patient characteristics.
Dosage adjustment with concomitant medications:
Erythromycin: Maximum pitavastatin dose: 1 mg/day
Rifampin: Maximum pitavastatin dose: 2 mg/day
Dosing: Geriatric
Refer to adult dosing.
Dosing: Pediatric
Note: Dosage should be individualized according to the baseline LDL-C level, the recommended goal of therapy, and patient response; adjustments should be made at intervals of 4 weeks. Lifestyle changes are recommended to be implemented for at least 6 to 12 months before beginning pharmacotherapy (AACE [Jellinger 2017]). Pitavastatin is available in 2 salt forms (calcium and magnesium); dosing expressed as mg of pitavastatin base.
Heterozygous familial hypercholesterolemia (HeFH): Children ≥8 years and Adolescents: Livalo (pitavastatin calcium): Oral: Initial: 2 mg once daily; evaluate lipids after 4 weeks and titrate dose accordingly; maximum daily dose: 4 mg/day; lipid levels should be evaluated 4 weeks after any dose adjustment.
Dosage adjustment with concomitant medications: Children ≥8 years and Adolescents: Livalo (pitavastatin calcium): Oral:
Erythromycin: Maximum daily pitavastatin dose: 1 mg/day.
Rifampin: Maximum daily pitavastatin dose: 2 mg/day.
Dosing adjustment for toxicity: Muscle symptoms (potential myopathy): Children ≥8 years and Adolescents: Discontinue use until symptoms can be evaluated; check CPK level; based on experience in adult patients, also evaluate patient for conditions that may increase the risk for muscle symptoms (eg, hypothyroidism; reduced renal or hepatic function; rheumatologic disorders such as polymyalgia rheumatica, steroid myopathy, vitamin D deficiency, or primary muscle diseases). Upon resolution (symptoms and any associated CPK abnormalities), resume the original dose or consider a lower dose of pitavastatin and retitrate. If muscle symptoms recur, discontinue pitavastatin use. After muscle symptom resolution, may then reinitiate a different statin at an initial low dose; gradually increase if tolerated. Based on experience in adult patients, if muscle symptoms or elevated CPK persists for 2 months in the absence of continued statin use, consider other causes of muscle symptoms. If determined to be due to another condition aside from statin use, may resume statin therapy at the original dose (NHLBI 2011; ACC/AHA [Stone 2013]).
Dosing: Adjustment for Toxicity
Severe muscle symptoms or fatigue: Promptly discontinue use; evaluate CPK, creatinine, and urinalysis for myoglobinuria (ACC/AHA [Stone 2013]).
Mild to moderate muscle symptoms: Discontinue use until symptoms can be evaluated; evaluate patient for conditions that may increase the risk for muscle symptoms (eg, hypothyroidism, reduced renal or hepatic function, rheumatologic disorders such as polymyalgia rheumatica, steroid myopathy, vitamin D deficiency, or primary muscle diseases). Upon resolution, resume the original or lower dose of pitavastatin. If muscle symptoms recur, discontinue pitavastatin use. After muscle symptom resolution, may then use a low dose of a different statin; gradually increase if tolerated. In the absence of continued statin use, if muscle symptoms or elevated CPK continues after 2 months, consider other causes of muscle symptoms. If determined to be due to another condition aside from statin use, may resume statin therapy at the original dose (ACC/AHA [Stone 2013]).
Administration
Administer with or without food; may take without regard to time of day.
Dietary Considerations
Red yeast rice contains variable amounts of several compounds that are structurally similar to HMG-CoA reductase inhibitors, primarily monacolin K (or mevinolin) which is structurally identical to lovastatin; concurrent use of red yeast rice with HMG-CoA reductase inhibitors may increase the incidence of adverse and toxic effects (Lapi 2008; Smith 2003).
Storage
Store at 15°C to 30°C (59°F to 86°F). Protect from light.
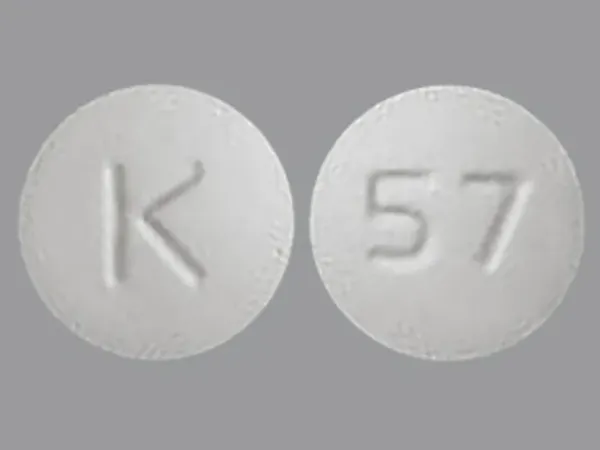
Pitavastatin Images
Drug Interactions
Acipimox: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Asunaprevir: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Atazanavir: May increase the serum concentration of Pitavastatin. Monitor therapy
Bezafibrate: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Bezafibrate may increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). More specifically, bezafibrate may increase the serum concentration of fluvastatin Management: Monitor patients closely for myopathy with concomitant use of bezafibrate and HMG-CoA reductase inhibitors. Concomitant use is contraindicated in patients predisposed to myopathy and alternative therapy should be considered. Consider therapy modification
Ciprofibrate: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Management: Avoid the use of HMG-CoA reductase inhibitors and ciprofibrate if possible. If concomitant therapy is considered, benefits should be carefully weighed against the risks, and patients should be monitored closely for signs/symptoms of muscle toxicity. Consider therapy modification
Clarithromycin: May increase the serum concentration of Pitavastatin. Monitor therapy
Cobicistat: May increase the serum concentration of Pitavastatin. Monitor therapy
Colchicine: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Colchicine may increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Consider therapy modification
CycloSPORINE (Systemic): May increase the serum concentration of Pitavastatin. Avoid combination
Daclatasvir: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
DAPTOmycin: HMG-CoA Reductase Inhibitors (Statins) may enhance the adverse/toxic effect of DAPTOmycin. Specifically, the risk of skeletal muscle toxicity may be increased. Management: Consider temporarily stopping HMG-CoA reductase inhibitor therapy prior to daptomycin. If used together, regular (i.e., at least weekly) monitoring of CPK concentrations is recommended. Consider therapy modification
Eltrombopag: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Erythromycin (Systemic): May increase the serum concentration of Pitavastatin. Management: Limit pitavastatin to a maximum of 1 mg/day (adult dose) when used in combination with erythromycin. If this combination is used, monitor patients more closely for evidence of pitavastatin toxicity. Consider therapy modification
Etravirine: May increase the serum concentration of Pitavastatin. Monitor therapy
Fenofibrate and Derivatives: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Fusidic Acid (Systemic): May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Specifically, the risk for muscle toxicities, including rhabdomyolysis may be significantly increased. Management: Avoid concurrent use whenever possible. Use is listed as contraindicated in product characteristic summaries in several countries, although UK labeling suggests that use could be considered under exceptional circumstances and with close supervision. Avoid combination
Gemfibrozil: May enhance the myopathic (rhabdomyolysis) effect of Pitavastatin. Gemfibrozil may increase the serum concentration of Pitavastatin. Avoid combination
Glecaprevir and Pibrentasvir: May increase the serum concentration of HMG-CoA Reductase Inhibitors (Statins). Management: Use the lowest statin dose possible if combined with glecaprevir/pibrentasvir and monitor for increased statin effects/toxicities. Avoid concomitant use with atorva-, simva-, or lovastatin. Limit rosuvastatin to 10 mg daily and reduce pravastatin dose 50% Consider therapy modification
Lanthanum: HMG-CoA Reductase Inhibitors (Statins) may decrease the serum concentration of Lanthanum. Management: Administer HMG-CoA reductase inhibitors at least two hours before or after lanthanum. Consider therapy modification
Letermovir: May increase the serum concentration of Pitavastatin. Avoid combination
Niacin: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Niacinamide: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Ombitasvir, Paritaprevir, Ritonavir, and Dasabuvir: May increase the serum concentration of Pitavastatin. Management: Canadian product labeling recommends use of the lowest pitavastatin dose with this combination. Monitor therapy
Raltegravir: May enhance the myopathic (rhabdomyolysis) effect of HMG-CoA Reductase Inhibitors (Statins). Monitor therapy
Red Yeast Rice: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Avoid combination
Repaglinide: HMG-CoA Reductase Inhibitors (Statins) may increase the serum concentration of Repaglinide. Monitor therapy
Rifamycin Derivatives: May increase the serum concentration of Pitavastatin. Management: Limit pitavastatin dose to a maximum of 2 mg/day with concurrent rifampin. Consider therapy modification
Rupatadine: May enhance the adverse/toxic effect of HMG-CoA Reductase Inhibitors (Statins). Specifically, the risk for increased CPK and/or other muscle toxicities may be increased. Monitor therapy
Simeprevir: May increase the serum concentration of Pitavastatin. Monitor therapy
Telithromycin: May increase the serum concentration of Pitavastatin. Monitor therapy
Teriflunomide: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Monitor therapy
Tolvaptan: May increase the serum concentration of OATP1B1/1B3 (SLCO1B1/1B3) Substrates. Consider therapy modification
Trabectedin: HMG-CoA Reductase Inhibitors (Statins) may enhance the myopathic (rhabdomyolysis) effect of Trabectedin. Monitor therapy
Vitamin K Antagonists (eg, warfarin): HMG-CoA Reductase Inhibitors (Statins) may enhance the anticoagulant effect of Vitamin K Antagonists. Monitor therapy
Voxilaprevir: May increase the serum concentration of Pitavastatin. Avoid combination
Adverse Reactions
1% to 10%:
Gastrointestinal: Constipation (4%), diarrhea (3%)
Neuromuscular & skeletal: Back pain (4%), myalgia (2% to 3%)
Frequency not defined:
Central nervous system: Headache
Dermatologic: Pruritus, skin rash, urticaria
Endocrine & metabolic: Increased serum glucose
Hepatic: Increased serum alkaline phosphatase, increased serum bilirubin, increased serum transaminases
Hypersensitivity: Hypersensitivity reaction
Infection: Influenza
Neuromuscular & skeletal: Arthralgia, increased creatine phosphokinase in blood specimen
Respiratory: Nasopharyngitis
<1%, postmarketing, and/or case reports: Abdominal distress, abdominal pain, amnesia, angioedema, asthenia, cognitive dysfunction, confusion, depression, dizziness, dyspepsia, elevated glycosylated hemoglobin, erectile dysfunction, fatigue, forgetfulness, hepatic failure, hepatitis, hypoesthesia, immune-mediated necrotizing myopathy, insomnia, interstitial pulmonary disease, jaundice, malaise, memory impairment, muscle spasm, myopathy, nausea, peripheral neuropathy, rhabdomyolysis
Warnings/Precautions
Concerns related to adverse effects:
- Diabetes mellitus: Increases in HbA1c and fasting blood glucose have been reported; however, the benefits of statin therapy far outweigh the risk of dysglycemia. Optimize lifestyle measures including exercise, maintaining a healthy body weight, and making healthy food choices.
- Hepatotoxicity: Elevations in serum transaminases have been reported; elevations were transient and resolved or improved on continued therapy or after a brief interruption in therapy in most cases. Postmarketing reports of fatal and nonfatal hepatic failure have been reported and are rare. If serious hepatotoxicity with clinical symptoms and/or hyperbilirubinemia or jaundice occurs during treatment, interrupt therapy promptly. Consider baseline and periodic liver enzyme tests, as clinically indicated. Ethanol may enhance the potential of adverse hepatic effects; instruct patients to avoid excessive ethanol consumption.
- Hypersensitivity: Hypersensitivity reactions, including rash, pruritus, and urticaria, have been reported.
- Myopathy/Rhabdomyolysis: Myopathy with CPK >10 times the ULN and rhabdomyolysis (sometimes fatal) with or without acute renal failure secondary to myoglobinuria have been reported; patients should be monitored closely. This risk is dose-related (doses >4 mg) and is increased with concurrent use of colchicine, erythromycin, fibrates, niacin (doses ≥1 g/day), or rifampin. If concurrent use is warranted, consider lower starting and maintenance doses of pitavastatin; use is contraindicated with cyclosporine and not recommended with gemfibrozil. Use caution in patients ≥65 years of age, uncontrolled hypothyroidism, and renal impairment; these patients are predisposed to myopathy. Immune-mediated necrotizing myopathy (IMNM) associated with HMG-CoA reductase inhibitors use has also been reported rarely. Patients should be instructed to report unexplained muscle pain, tenderness, weakness, or brown urine, particularly if accompanied by malaise or fever or if muscle signs and symptoms persist after discontinuing pitavastatin. Temporarily withhold therapy in any patient with an acute, serious condition suggestive of myopathy or predisposing to the development of renal failure secondary to rhabdomyolysis (eg, sepsis; shock; severe hypovolemia; major surgery; trauma; severe metabolic, endocrine, electrolyte disorders; uncontrolled epilepsy). Discontinue therapy if markedly elevated CPK levels occur or myopathy is diagnosed/suspected.
Disease-related concerns:
- Hepatic impairment: Use is contraindicated in patients with active liver disease or unexplained persistent elevations of serum transaminases; use with caution in patients who consume large amounts of ethanol or have a history of liver disease.
- Renal impairment: Use with caution in patients with renal impairment; these patients are predisposed to myopathy and rhabdomyolysis. Dosage adjustment required in patients with GFR <60 mL/minute/1.73 m2 including end-stage renal disease receiving hemodialysis.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special Populations:
- Elderly: Use with caution in patients ≥65 years of age; these patients are predisposed to myopathy and rhabdomyolysis.
- Surgical patients: The manufacturer recommends temporary discontinuation for elective major surgery, acute medical or surgical conditions, or in any patient experiencing an acute or serious condition predisposing to renal failure (eg, sepsis; shock; severe hypovolemia; trauma; severe metabolic, endocrine, electrolyte disorders; uncontrolled epilepsy). Based on current research and clinical guidelines, HMG-CoA reductase inhibitors should be continued in the perioperative period for noncardiac and cardiac surgery (ACC/AHA [Fleisher 2014]; ACC/AHA [Hillis 2011]). Perioperative discontinuation of statin therapy is associated with an increased risk of cardiac morbidity and mortality.
Other warnings/precautions:
- Appropriate use: The effect on cardiovascular morbidity and mortality has not been determined.
- Hyperlipidemia: Secondary causes of hyperlipidemia should be ruled out prior to therapy.
Monitoring Parameters
ACC/AHA Blood Cholesterol Guideline recommendations (ACC/AHA [Grundy 2018]; ACC/AHA [Stone 2013]):
Lipid panel (total cholesterol, HDL, LDL, triglycerides): Lipid profile (fasting or nonfasting) before initiating treatment. Fasting lipid profile should be rechecked 4 to 12 weeks after starting therapy and every 3 to 12 months thereafter. If 2 consecutive LDL levels are <40 mg/dL, consider decreasing the dose.
Hepatic transaminase levels: Baseline measurement of hepatic transaminase levels (AST and ALT); measure AST, ALT, total bilirubin, and alkaline phosphatase if symptoms suggest hepatotoxicity (eg, unusual fatigue or weakness, loss of appetite, abdominal pain, dark-colored urine or yellowing of skin or sclera) during therapy.
CPK: CPK should not be routinely measured. Baseline CPK measurement is reasonable for some individuals (eg, family history of statin intolerance or muscle disease, clinical presentation, concomitant drug therapy that may increase risk of myopathy). May measure CPK in any patient with symptoms suggestive of myopathy (pain, tenderness, stiffness, cramping, weakness, or generalized fatigue).
Evaluate for new-onset diabetes mellitus during therapy; if diabetes develops, continue statin therapy and encourage adherence to a heart-healthy diet, physical activity, a healthy body weight, and tobacco cessation.
If patient develops a confusional state or memory impairment, may evaluate patient for nonstatin causes (eg, exposure to other drugs), systemic and neuropsychiatric causes, and the possibility of adverse effects associated with statin therapy.
Pregnancy
Pregnancy Considerations
Pitavastatin is contraindicated in pregnant females.
There are reports of congenital anomalies following maternal use of HMG-CoA reductase inhibitors in pregnancy; however, maternal disease, differences in specific agents used, and the low rates of exposure limit the interpretation of the available data (Godfrey 2012; Lecarpentier 2012). Cholesterol biosynthesis may be important in fetal development; serum cholesterol and triglycerides increase normally during pregnancy. The discontinuation of lipid lowering medications temporarily during pregnancy is not expected to have significant impact on the long term outcomes of primary hypercholesterolemia treatment.
Pitavastatin should be discontinued immediately if an unplanned pregnancy occurs during treatment.
Adequate contraception is recommended if an HMG-CoA reductase inhibitor is required in females of reproductive potential. Females planning a pregnancy should discontinue the HMG-CoA reductase inhibitor 1 to 2 months prior to attempting to conceive (AHA/ACC [Grundy 2018]).
Patient Education
What is this drug used for?
- It is used to lower bad cholesterol and raise good cholesterol (HDL).
- It is used to lower triglycerides.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Back pain
- Constipation
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Unable to pass urine
- Change in amount of urine passed
- Muscle pain
- Muscle tenderness
- Muscle weakness
- Liver problems like dark urine, feeling tired, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin or eyes.
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.