Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling.
Suspension, Oral:
CaroSpir: 25 mg/5 mL (118 mL, 473 mL) [contains saccharin sodium; banana flavor]
Tablet, Oral:
Aldactone: 25 mg
Aldactone: 50 mg, 100 mg [scored]
Generic: 25 mg, 50 mg, 100 mg
Pharmacology
Mechanism of Action
Competes with aldosterone for receptor sites in the distal renal tubules, increasing sodium chloride and water excretion while conserving potassium and hydrogen ions; may block the effect of aldosterone on arteriolar smooth muscle as well
Pharmacokinetics/Pharmacodynamics
Metabolism
Rapid and extensive; hepatic to multiple metabolites, including active metabolites canrenone, 7-alpha-spirolactone, and 6-beta-hydroxy-7-alpha
Excretion
Urine (primarily as metabolites) and bile (secondary)
Time to Peak
Serum:
Tablet: 2.6 to 4.3 hours (primarily as active metabolites)
Suspension: Spironolactone: 0.5 to 1.5 hours; Canrenone: 2.5 to 5 hours
Duration of Action
Tablet: 2 to 3 days
Half-Life Elimination
Tablet: Spironolactone: 1.4 hours; Canrenone: 16.5 hours (terminal); 7-alpha-spirolactone: 13.8 hours (terminal)
Suspension: Spironolactone: 1 to 2 hours; Canrenone, 7-alpha-spirolactone, and 6-beta-hydroxy-7-alpha: 10 to 35 hours
Protein Binding
>90%
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Terminal half-life is increased in patients with cirrhotic ascites.
Use: Labeled Indications
Ascites due to cirrhosis: Management of edema in cirrhosis of the liver unresponsive to fluid and sodium restriction.
Heart failure with reduced ejection fraction: To increase survival, manage edema, and reduce need for hospitalization in patients with heart failure with reduced ejection fraction and New York Heart Association class III to IV symptoms; usually administered in conjunction with other heart failure therapies.
Hypertension: Management of hypertension unresponsive to other therapies.
Primary hyperaldosteronism (tablet only): Short-term preoperative treatment of primary hyperaldosteronism; long-term maintenance therapy for patients with discrete aldosterone-producing adrenal adenomas who are not candidates for surgery; long-term maintenance therapy for bilateral micro- or macronodular adrenal hyperplasia (idiopathic hyperaldosteronism).
Use: Off Label
Acne vulgaris, femalescyes
Data from a limited number of patients in a small number of randomized, placebo-controlled trials suggest that spironolactone may be beneficial in the treatment of moderate to severe acne in women Goodfellow 1984, Muhlemann 1986.
Based on the
Heart failure with preserved ejection fractionbyes
Data from a randomized, double-blind, placebo-controlled trial of patients with heart failure with preserved ejection fraction (HFpEF) suggest that spironolactone may be effective at reducing hospitalizations for heart failure, which was one component of the composite primary end point. A subgroup of patients who were enrolled on the basis of natriuretic peptide criteria displayed a reduction in the composite primary end point (cardiovascular death, aborted cardiac arrest, or hospitalization for heart failure) Pitt 2014.
Based on the American College of Cardiology (ACC)/American Heart Association (AHA)/Heart Failure Society of America update of the guideline for the management of heart failure, spironolactone may be effective and might be considered to reduce hospitalizations for heart failure in appropriately selected patients with symptomatic HFpEF (ejection fraction ≥45%) who have elevated serum natriuretic peptide level or have been hospitalized for HF in the last 12 months.
Heart failure with reduced ejection fraction (New York Heart Association class II)yes
Based on the American College of Cardiology Foundation (ACCF)/AHA guideline for the management of heart failure, spironolactone (along with other guideline-directed medical therapies) is effective and recommended to reduce morbidity and mortality in patients with heart failure (New York Heart Association class II to IV) with a left ventricular ejection fraction (LVEF) ≤35%.
Hirsutism, femalesbyes
Data from a systematic review and network meta-analysis of published randomized trials of adult females with hirsutism (including idiopathic hirsutism and hirsutism in women with polycystic ovary syndrome or nonclassic congenital adrenal hyperplasia) support the use of spironolactone in the treatment of hirsutism Barrionuevo 2018.
Based on the Endocrine Society clinical practice guideline on the evaluation and treatment of hirsutism in premenopausal women, spironolactone is effective and may be considered among other antiandrogens in the management of this condition. Spironolactone may be considered for initial therapy, either as monotherapy in women who are not at risk for becoming pregnant or in combination with an oral contraceptive in select women with severe hirsutism causing distress and/or a prior history of inadequate response to oral contraceptive therapy. Spironolactone may also be considered for add-on therapy in women who fail to achieve a satisfactory response to initial oral contraceptive monotherapy Endocrine Society [Martin 2018].
Hormone therapy for transgender females, male-to-femaleyes
Based on the Endocrine Society clinical practice guideline for endocrine treatment of gender dysphoric/gender incongruent persons, spironolactone is effective when used in combination with estrogen to block androgens in transgender females, thereby reducing testosterone levels into the normal range for females. The result is decreased hair growth, muscle mass, sexual desire, sperm production, spontaneous erections, and testicular volume, as well as breast growth, male sexual dysfunction, redistribution of body fat, and skin and voice changes ES [Hembree 2017].
Post myocardial infarction, complicated by reduced ejection fractionyes
According to the ACCF/AHA guideline for the management of ST-elevation myocardial infarction and the AHA/ACC guideline for the management of non–ST-elevation acute coronary syndromes, an aldosterone antagonist should be given to post-myocardial infarction patients (without significant renal dysfunction) who are already on an angiotensin-converting enzyme inhibitor and beta-blocker, who have an LVEF ≤40%, and either symptomatic heart failure or diabetes mellitus.
Contraindications
Hyperkalemia; Addison disease; concomitant use with eplerenone.
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to spironolactone or any component of the formulation; acute renal insufficiency; severe renal impairment (eGFR <30 mL/minute/1.73 m2); anuria; concomitant use with heparin or low molecular weight heparin; pregnancy; breastfeeding.
Dosage and Administration
Dosing: Adult
Note: Suspension is not therapeutically equivalent to tablets. Suspension results in 15% to 37% higher serum concentration compared to tablets. Doses of suspension >100 mg may result in higher than expected serum concentrations. In patients requiring >100 mg/dose, use tablets only.
Acne vulgaris, females (alternative agent) (off-label use):
Tablet: Oral: Initial: 25 to 50 mg/day in 1 to 2 divided doses; titrate as needed based on response and tolerability to a usual effective dose of 50 to 100 mg/day in 1 to 2 divided doses; maximum dose: 200 mg/day (AAD [Zaenglein 2016]; Goodfellow 1984; Graber 2019; Muhlemann 1986; Shaw 2000; Yemisci 2005).
Ascites due to cirrhosis:
Note: Generally used in combination with furosemide, but may be used as monotherapy for patients with hypokalemia. For combination therapy, a dosing ratio of spironolactone 100 mg to furosemide 40 mg should generally be maintained, but can be adjusted for electrolyte abnormalities (AASLD [Runyon 2013]; Runyon 2019).
Tablet: Oral: Initial: 100 mg once daily; titrate every 3 to 5 days based on response and tolerability; usual maximum dose: 400 mg once daily (AASLD [Runyon 2013]; Runyon 2019). For small-volume ascites in patients who weigh ≤50 kg, some experts recommend a starting dose of 50 mg once daily (Runyon 2019).
Heart failure:
Note: When initiating therapy, verify the following: serum creatinine ≤2.5 mg/dL in men and ≤2 mg/dL in women or eGFR >30 mL/minute/1.73 m2and serum potassium <5 mEq/L. If patient develops hyperkalemia (serum potassium >5.5 mEq/L), reduce the dose, change to every-other-day dosing, or discontinue therapy. If renal function worsens, consider dose reduction or discontinuation (ACC/AHA/HFSA [Yancy 2017]; ACCF/AHA [Yancy 2013]).
Heart failure with preserved ejection fraction (off-label use):
Note: May be considered for use in patients with symptomatic heart failure with preserved ejection fraction (≥45%) who have an elevated serum natriuretic peptide level or have been hospitalized for heart failure in the last 12 months (ACC/AHA/HFSA [Yancy 2017]; Pitt 2014). Some experts recommend initiating therapy only if serum potassium is ≤4.7 mEq/L and eGFR is ≥30 mL/minute/1.73 m2. The same experts recommend dose reduction when serum potassium is >5 mEq/L and discontinuation when serum potassium is >5.5 mEq/L (Borlaug 2019).
Tablet: Oral: Initial: 12.5 mg once daily; may double the dose every 4 weeks if serum potassium remains <5 mEq/L and renal function is stable, up to a maximum target dose of 50 mg/day in 1 or 2 divided doses (ACC/AHA/HFSA [Yancy 2017]; Borlaug 2019; Pitt 2014). Some experts recommend up-titrating therapy only if serum potassium is ≤4.5 mEq/L (Borlaug 2019).
Heart failure with reduced ejection fraction:
Note: Should be considered for use in patients with symptomatic (New York Heart Association class II to IV) heart failure with reduced ejection fraction (≤35%) who are already taking optimal doses of other heart failure therapies (ACC/AHA/HFSA [Yancy 2017]; ACCF/AHA [Yancy 2013]).
Tablet: Oral: Initial: 12.5 to 25 mg once daily; may double the dose every 4 weeks if serum potassium remains <5 mEq/L and renal function is stable, up to a maximum target dose of 50 mg/day in 1 to 2 divided doses (ACC/AHA/HFSA [Yancy 2017]; ACCF/AHA [Yancy 2013]; Pitt 1999).
Suspension: Oral: Initial: 10 to 20 mg once daily. Consider a starting dose of 10 mg once daily in patients at increased risk of hyperkalemia. May titrate to 37.5 mg once daily if serum potassium remains <5 mEq/L and renal function is stable (ACCF/AHA [Yancy 2013]; Colucci 2019; manufacturer labeling).
Post-myocardial infarction, complicated by reduced ejection fraction (off-label use):
Note: Should be considered for use following acute myocardial infarction (MI) in patients with left ventricular ejection fraction ≤40% plus symptoms of heart failure or diabetes. Use in addition to other pharmacologic therapies post MI (ACCF/AHA [O’Gara 2013]; ACCF/AHA [Yancy 2013]).
Tablet: Oral: Initial: 12.5 to 25 mg once daily; may double the dose every 4 weeks if serum potassium remains <5 mEq/L and renal function is stable, up to a maximum target dose of 50 mg/day in 1 to 2 divided doses (ACCF/AHA [Yancy 2013]).
Suspension: Oral: Initial: 10 to 20 mg once daily. Consider a starting dose of 10 mg once daily in patients at increased risk of hyperkalemia. May titrate to 37.5 mg once daily if serum potassium remains <5 mEq/L and renal function is stable (ACCF/AHA [Yancy 2013]; Colucci 2019).
Hirsutism, females (alternative agent) (off-label use):
Note: Typically given in addition to oral contraceptives (OCs) if inadequate response to OCs is observed after 6 months. May be considered as initial therapy for females who cannot conceive or who are using reliable contraception (Barbieri 2019; ES [Martin 2018]).
Tablet: Oral: Initial: 50 mg twice daily; may increase to 100 mg twice daily as needed. Assess response at 6-month intervals before adjusting dose, adding additional agents, or switching to alternative therapy (Barbieri 2019; ES [Martin 2018]).
Hormone therapy for transgender females, male-to-female (adjunctive agent) (off-label use):
Tablet: Oral: Initial: 25 mg once or twice daily in combination with other appropriate agents. Increase at 1-week intervals based on response and tolerability to a usual dose of 100 to 300 mg/day in 2 divided doses; maximum dose: 400 mg/day. Adjust dose with a goal of suppressing serum testosterone levels into the normal range for females (<50 ng/dL) (Deutsch 2016; ES [Hembree 2017]; Prior 1989).
Hypertension (alternative agent):
Note: Not recommended for initial management but may be considered as additional therapy for resistant hypertension in patients who do not respond adequately to combination therapy with preferred agents (ACC/AHA [Whelton 2018]; Bazoukis 2018).
Tablet: Oral: Initial: 25 mg once daily; titrate as needed based on response and tolerability up to 100 mg once daily (ACC/AHA [Whelton 2018]; Bazoukis 2018; Oxlund 2013; Williams 2015). Some experts recommend a starting dose of 12.5 mg once daily and generally do not exceed 50 mg once daily in the absence of primary aldosteronism (Calhoun 2019).
Suspension: Oral: Initial: 20 to 75 mg/day in 1 or 2 divided doses; may titrate at 2-week intervals as needed based on response and tolerability.
Primary aldosteronism:
Tablet: Oral: Initial: 12.5 to 25 mg once daily (ES [Funder 2016]); gradually titrate to the lowest effective dose; usual maximum dose: 400 mg/day (Young 2019). For surgical candidates, the last dose should be administered the day of surgery; discontinue spironolactone on postoperative day 1 (ES [Funder 2016]; Young 2019).
Dosing: Geriatric
Heart failure: Oral: Avoid use of tablets >25 mg/day (or equivalent dose of suspension) (ACCF/AHA [Yancy 2013]).
Dosing: Pediatric
Note: Although spironolactone is commercially available in a suspension, it is NOT therapeutically equivalent to the tablets; commercially available suspension results in 15% to 37% higher serum concentration compared to the tablet; pediatric dosing is based on experience with tablets and extemporaneously compounded suspension. Multiple concentrations of oral suspension exist; use extra precaution and prescribe in mg (not mL).
Bronchopulmonary dysplasia (BPD): Limited data available; efficacy results variable. Although the benefits of diuretic therapy in the management of BPD are variable (eg, optimal duration of therapy, impact on pulmonary endpoints), diuretics continue to be used in clinical practice (Slaughter 2013). Infants: Oral: 1.5 mg/kg/dose every 12 hours (Albersheim 1989; Engelhardt 1989; Hoffman 2000; Stewart 2011).
Edema (diuresis): Limited data available: Infants, Children, and Adolescents: Oral: Initial: 1 to 3 mg/kg/day divided every 6 to 24 hours; titrate as needed; reported maximum daily dose range: 4 to 6 mg/kg/day in divided doses every 6 to 12 hours or 400 mg/day, whichever is less (Giefer 2011; Kliegman 2016; Sabri 2003; van der Vorst 2006)
Hypertension: Limited data available: Infants, Children, and Adolescents: Oral: Initial: 1 mg/kg/day divided every 12 to 24 hours; titrate as needed up to a maximum daily dose: 3.3 mg/kg/day or 100 mg/day, whichever is less (NHBPEP 2004; Park 2014)
Primary aldosteronism (caused by adrenal hyperplasia), treatment: Limited data available: Infants, Children, and Adolescents: Oral: 1 to 3 mg/kg/day; maximum daily dose: 100 mg/day (Kliegman 2016)
Extemporaneously Prepared
5 mg/mL Oral Suspension (ASHP Standard Concentration) (ASHP 2017)
A 5 mg/mL oral suspension may be made with tablets. Crush twelve 50 mg tablets in a mortar and reduce to a fine powder. Add small portions of distilled water and mix to a uniform paste; mix while adding cherry syrup to almost 120 mL; transfer to a calibrated glass bottle, rinse mortar with cherry syrup, and add quantity of cherry syrup sufficient to make 120 mL. Label "shake well" and "refrigerate." Stable for 28 days at room temperature or refrigerated (Mathur 1989).
Mathur LK, Wickman A. Stability of extemporaneously compounded spironolactone suspensions. Am J Hosp Pharm. 1989;46(10):2040-2042.2816959
1 mg/mL Oral Suspension
A 1 mg/mL oral suspension may be made with tablets. Crush ten 25 mg tablets in a mortar and reduce to a fine powder. Add a small amount of purified water and soak for 5 minutes; add 50 mL 1.5% carboxymethylcellulose, 100 mL syrup NF, and mix to a uniform paste; mix while adding purified water in incremental proportions to almost 250 mL; transfer to a calibrated bottle, rinse mortar with purified water, and add quantity of purified water sufficient to make 250 mL. Label "shake well." Stable for 3 months at room temperature or refrigerated (Nahata 1993).
Nahata MC, Morosco RS, and Hipple TF, "Stability of Spironolactone in an Extemporaneously Prepared Suspension at Two Temperatures," Ann Pharmacother. 1993, 27(10):1198-9.8251687
25 mg/mL Oral Suspension
A 25 mg/mL oral suspension may be made with tablets and either a 1:1 mixture of Ora-Sweet and Ora-Plus or a 1:1 mixture of Ora-Sweet SF and Ora-Plus. Crush one-hundred-twenty 25 mg tablets in a mortar and reduce to a fine powder. Add small portions of chosen vehicle and mix to a uniform paste; mix while adding vehicle in incremental proportions to almost 120 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add quantity of vehicle sufficient to make 120 mL. Store in amber bottles; label "shake well" and "refrigerate." Stable for 60 days refrigerated (Allen 1996).
Allen LV Jr and Erickson MA 3rd, "Stability of Ketoconazole, Metolazone, Metronidazole, Procainamide Hydrochloride, and Spironolactone in Extemporaneously Compounded Oral Liquids," Am J Health Syst Pharm. 1996, 53(17):2073-8.8870895
Administration
Oral:
Tablet: Administer with or without food; however, administer consistently with respect to food.
Suspension: Shake well before administering dose. Administer with or without food; however, administer consistently with respect to food.
Dietary Considerations
Administration with food increases the bioavailability of spironolactone. Excessive potassium intake (eg, salt substitutes, low-salt foods, bananas, nuts) should be avoided.
Storage
Tablet: Store below 25°C (77°F).
Suspension: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
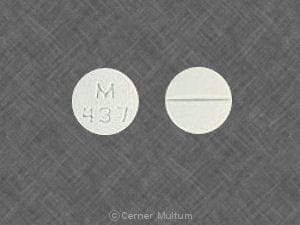
Spironolactone Images
Drug Interactions
Abiraterone Acetate: Spironolactone may diminish the therapeutic effect of Abiraterone Acetate. Monitor therapy
Alfuzosin: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Alpha-/Beta-Agonists: Spironolactone may diminish the vasoconstricting effect of Alpha-/Beta-Agonists. Monitor therapy
Amifostine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Amifostine. Management: When amifostine is used at chemotherapy doses, blood pressure lowering medications should be withheld for 24 hours prior to amifostine administration. If blood pressure lowering therapy cannot be withheld, amifostine should not be administered. Consider therapy modification
AMILoride: May enhance the hyperkalemic effect of Spironolactone. Avoid combination
Ammonium Chloride: Potassium-Sparing Diuretics may enhance the adverse/toxic effect of Ammonium Chloride. Specifically the risk of systemic acidosis. Consider therapy modification
Amphetamines: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Angiotensin II Receptor Blockers: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
Angiotensin-Converting Enzyme Inhibitors: Potassium-Sparing Diuretics may enhance the hyperkalemic effect of Angiotensin-Converting Enzyme Inhibitors. Monitor therapy
Antipsychotic Agents (Second Generation [Atypical]): Blood Pressure Lowering Agents may enhance the hypotensive effect of Antipsychotic Agents (Second Generation [Atypical]). Monitor therapy
Aspirin: May diminish the therapeutic effect of Spironolactone. Monitor therapy
AtorvaSTATin: May enhance the adverse/toxic effect of Spironolactone. Specifically, there is a theoretical potential for enhanced effects on reducing endogenous steroid activity. Monitor therapy
Barbiturates: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Benperidol: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Brigatinib: May diminish the antihypertensive effect of Antihypertensive Agents. Brigatinib may enhance the bradycardic effect of Antihypertensive Agents. Monitor therapy
Brimonidine (Topical): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Bromperidol: Blood Pressure Lowering Agents may enhance the hypotensive effect of Bromperidol. Bromperidol may diminish the hypotensive effect of Blood Pressure Lowering Agents. Avoid combination
Cardiac Glycosides: Potassium-Sparing Diuretics may diminish the therapeutic effect of Cardiac Glycosides. In particular, the inotropic effects of digoxin appear to be diminished. Potassium-Sparing Diuretics may increase the serum concentration of Cardiac Glycosides. This particular effect may be unique to Spironolactone. Monitor therapy
Cholestyramine Resin: May enhance the adverse/toxic effect of Spironolactone. Specifically, the risks of developing metabolic acidosis and hyperkalemia may be elevated with this combination. Monitor therapy
Ciprofloxacin (Systemic): Spironolactone may enhance the arrhythmogenic effect of Ciprofloxacin (Systemic). Monitor therapy
Cosyntropin: Spironolactone may diminish the diagnostic effect of Cosyntropin. Management: Patients receiving spironolactone should omit their pre-test dose on the day selected for cosyntropin testing. Consider therapy modification
CycloSPORINE (Systemic): Potassium-Sparing Diuretics may enhance the hyperkalemic effect of CycloSPORINE (Systemic). Avoid combination
Dexmethylphenidate: May diminish the therapeutic effect of Antihypertensive Agents. Monitor therapy
Diacerein: May enhance the therapeutic effect of Diuretics. Specifically, the risk for dehydration or hypokalemia may be increased. Monitor therapy
Diazoxide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Digoxin: Spironolactone may increase the serum concentration of Digoxin. Spironolactone (and/or its metabolites) may also interfere with the assays used to determine Digoxin concentrations, falsely increasing or decreasing Digoxin concentrations. Monitor therapy
Drospirenone: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
DULoxetine: Blood Pressure Lowering Agents may enhance the hypotensive effect of DULoxetine. Monitor therapy
Eplerenone: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Management: This combination is contraindicated in patients receiving eplerenone for treatment of hypertension. Consider therapy modification
Heparin: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Management: Monitor serum potassium concentrations closely. The spironolactone Canadian product monograph lists its combination with heparin or low molecular weight heparins as contraindicated. Monitor therapy
Heparins (Low Molecular Weight): May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Management: Monitor serum potassium concentrations closely. The spironolactone Canadian product monograph lists its combination with heparin or low molecular weight heparins as contraindicated. Monitor therapy
Herbs (Hypertensive Properties): May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Herbs (Hypotensive Properties): May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Hypotension-Associated Agents: Blood Pressure Lowering Agents may enhance the hypotensive effect of Hypotension-Associated Agents. Monitor therapy
Levodopa-Containing Products: Blood Pressure Lowering Agents may enhance the hypotensive effect of Levodopa-Containing Products. Monitor therapy
Lormetazepam: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Methylphenidate: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Mitotane: Spironolactone may diminish the therapeutic effect of Mitotane. Management: Consideration should be given to discontinuing spironolactone prior to initiating mitotane in order to eliminate the risk of therapeutic failure of the mitotane. Consider therapy modification
Molsidomine: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Naftopidil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Neuromuscular-Blocking Agents (Nondepolarizing): Spironolactone may enhance the neuromuscular-blocking effect of Neuromuscular-Blocking Agents (Nondepolarizing). Monitor therapy
Nicergoline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nicorandil: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
Nicorandil: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Nitroprusside: Blood Pressure Lowering Agents may enhance the hypotensive effect of Nitroprusside. Monitor therapy
Nonsteroidal Anti-Inflammatory Agents: May diminish the antihypertensive effect of Potassium-Sparing Diuretics. Nonsteroidal Anti-Inflammatory Agents may enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
Obinutuzumab: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Management: Consider temporarily withholding blood pressure lowering medications beginning 12 hours prior to obinutuzumab infusion and continuing until 1 hour after the end of the infusion. Consider therapy modification
Opioid Agonists: May enhance the adverse/toxic effect of Diuretics. Opioid Agonists may diminish the therapeutic effect of Diuretics. Monitor therapy
Pentoxifylline: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Pholcodine: Blood Pressure Lowering Agents may enhance the hypotensive effect of Pholcodine. Monitor therapy
Phosphodiesterase 5 Inhibitors: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Potassium Salts: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Consider therapy modification
Prostacyclin Analogues: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
Quinagolide: May enhance the hypotensive effect of Blood Pressure Lowering Agents. Monitor therapy
QuiNIDine: Potassium-Sparing Diuretics may diminish the therapeutic effect of QuiNIDine. Monitor therapy
Sodium Phosphates: Diuretics may enhance the nephrotoxic effect of Sodium Phosphates. Specifically, the risk of acute phosphate nephropathy may be enhanced. Management: Consider avoiding this combination by temporarily suspending treatment with diuretics, or seeking alternatives to oral sodium phosphate bowel preparation. If the combination cannot be avoided, hydrate adequately and monitor fluid and renal status. Consider therapy modification
Tacrolimus (Systemic): Potassium-Sparing Diuretics may enhance the hyperkalemic effect of Tacrolimus (Systemic). Monitor therapy
Tolvaptan: May enhance the hyperkalemic effect of Potassium-Sparing Diuretics. Monitor therapy
Triamterene: May enhance the hyperkalemic effect of Spironolactone. Avoid combination
Trimethoprim: May enhance the hyperkalemic effect of Spironolactone. Monitor therapy
Yohimbine: May diminish the antihypertensive effect of Antihypertensive Agents. Monitor therapy
Test Interactions
May interfere with the radioimmunoassay for digoxin; may lead to false negative aldosterone/renin ratio (ARR) (Funder 2016; Mulatero 2002)
Adverse Reactions
1% to 10%:
Endocrine & metabolic: Gynecomastia (9%)
Frequency not defined.
Cardiovascular: Vasculitis
Central nervous system: Ataxia, confusion, dizziness, drowsiness, headache, lethargy, nipple pain
Dermatologic: Alopecia, chloasma, erythematous maculopapular rash, pruritus, Stevens-Johnson syndrome, toxic epidermal necrolysis, urticaria
Endocrine & metabolic: Amenorrhea, asymptomatic hyperuricemia, decreased libido, electrolyte disorder, gout, hyperglycemia, hyperkalemia, hyperuricemia, hypocalcemia, hypomagnesemia, hyponatremia, hypovolemia
Gastrointestinal: Abdominal cramps, diarrhea, gastritis, gastrointestinal hemorrhage, gastrointestinal ulcer, nausea, vomiting
Genitourinary: Erectile dysfunction, irregular menses, mastalgia, postmenopausal bleeding
Hematologic & oncologic: Agranulocytosis, leukopenia, thrombocytopenia
Hepatic: Hepatotoxicity
Hypersensitivity: Anaphylaxis
Immunologic: Drug reaction with eosinophilia and systemic symptoms
Neuromuscular & skeletal: Lower limb cramp
Renal: Renal failure syndrome, renal insufficiency
Miscellaneous: Fever
Postmarketing: Metabolic acidosis (in patients with cirrhosis [Feinfeld 1978; Gabow 1979])
Warnings/Precautions
Concerns related to adverse effects:
- Fluid/electrolyte imbalance: Fluid and electrolyte imbalance (eg, hypomagnesemia, hyponatremia, hypocalcemia, hyperglycemia, hyperkalemia) may occur. Patients with heart failure, renal disease, or cirrhosis may be particularly susceptible. Monitor and correct electrolyte disturbances; adjust dose to avoid dehydration.
- Gout: Asymptomatic hyperuricemia may occur and gout may be precipitated (rare).
- Gynecomastia: May occur; risk increases based on dose and onset is variable (after 1 to 2 months to over a year of therapy); usually reversible following discontinuation of therapy.
- Hyperkalemia: Hyperkalemia may occur; risk of hyperkalemia is increased with renal impairment, excessive potassium intake, and patients taking certain drugs (eg, angiotensin-converting enzyme [ACE] inhibitors, angiotensin-receptor blockers [ARBs], nonsteroidal anti-inflammatory drugs). Monitor serum potassium closely. The concurrent use of larger doses of ACE inhibitors (eg, lisinopril ≥10 mg daily in adults) also increases the risk of hyperkalemia (ACC/AHA [Yancy 2013]). Dose reduction or interruption of therapy may be necessary with development of hyperkalemia. Use is contraindicated in patients with hyperkalemia; use caution in conditions known to cause hyperkalemia.
- Tumorigenic: Shown to be a tumorigen in chronic toxicity animal studies. Avoid unnecessary use.
Disease-related concerns:
- Adrenal vein catheterization: Discontinue use prior to adrenal vein catheterization.
- Heart failure: When evaluating a heart failure patient for spironolactone treatment, eGFR should be >30 mL/minute/1.73 m2 or creatinine should be ≤2.5 mg/dL (men) or ≤2 mg/dL (women) with no recent worsening and potassium <5 mEq/L with no history of severe hyperkalemia (ACC/AHA [Yancy 2013]). Serum potassium levels require close monitoring and management if elevated. American College of Cardiology/American Heart Association recommends considering discontinuation upon the development of serum potassium >5.5 mEq/L or worsening renal function with careful evaluation of the entire medical regimen. Avoid triple therapy with the combined use of an ACE inhibitor, ARB, and spironolactone. Therapy may need to be modified during an episode of diarrhea or dehydration or when loop diuretic therapy is interrupted (ACC/AHA [Yancy 2013]).
- Hepatic impairment: Use with caution in patients with hepatic impairment; minor alterations of fluid and electrolyte balance may precipitate hepatic coma.
- Renal impairment: Risk of hyperkalemia is increased with declining renal function and with the concurrent use of larger doses of ACE inhibitors (eg, lisinopril ≥10 mg daily in adults) (ACC/AHA [Yancy 2013]). Use with caution in patients with renal impairment.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Avoid use of tablets >25 mg/day in elderly patients with heart failure or with reduced renal function (eg, CrCl <30 mL/minute or eGFR ≤30 mL/minute/1.73 m2 [ACC/AHA (Yancy 2013)]).
Other warnings/precautions:
- Suspension: Suspension is NOT therapeutically equivalent to tablets. In patients requiring >100 mg/dose, use tablets (>100 mg/dose of suspension may result in spironolactone concentration higher than expected).
Monitoring Parameters
Blood pressure, serum electrolytes (potassium [within 1 week of initiation or dose titration and regularly thereafter], sodium), uric acid, glucose, renal function, volume status
Heart failure: Serum potassium and renal function should be checked in 3 days after initiation, at 1 week after initiation, at least monthly for the first 3 months of therapy, and every 3 months thereafter. If adding or increasing the dose of concomitant ACE inhibitors or ARBs, a new cycle of monitoring should be done. If serum potassium increases to >5.5 mEq/L or renal function worsens, hold doses until potassium is <5 mEq/L and consider restarting with a reduced dose after confirming resolution of hyperkalemia/renal insufficiency for at least 72 hours (ACC/AHA [Yancy 2013]).
Transgender hormone therapy: Serum testosterone levels (goal: <50 ng/dL) every 3 months during the first year and then annually or biannually; serum electrolytes every 3 months for the first year then annually; routine cancer and laboratory screening as in non-transgender individuals for all tissues present (ES [Hembree 2017]).
Pregnancy
Pregnancy Considerations
Spironolactone crosses the placenta (Regitz-Zagrosek [ESC 2018]).
Based on the mechanism of action and data from animal reproduction studies, in utero exposure to spironolactone may cause feminization of a male fetus (limited human data; Liszewski 2019).
Chronic maternal hypertension is associated with adverse events in the fetus/infant. The risk of birth defects, low birth weight, premature delivery, stillbirth, and neonatal death may be increased with chronic hypertension in pregnancy. Actual risks may be related to duration and severity of maternal hypertension. The use of mineralocorticoid receptor antagonists for the treatment of hypertension in pregnancy is generally not recommended (ACOG 203 2019).
The treatment of edema associated with chronic heart failure during pregnancy is similar to that of nonpregnant patients. However, the use of mineralocorticoid receptor antagonists is not recommended. Patients diagnosed after delivery can be treated according to heart failure guidelines (ESC [Bauersachs 2016]; ESC [Regitz-Zagrosek 2018]).
Information related to the use of mineralocorticoid receptor antagonists for the treatment of primary hyperaldosteronism in pregnancy is limited. Women who require use of spironolactone for the treatment of primary hyperaldosteronism should use the lowest effective dose prior to a planned pregnancy, then stop treatment during the first trimester once the pregnancy is confirmed. Use of a mineralocorticoid receptor antagonist can be considered again in the second and third trimesters if necessary; high doses have been associated with intrauterine growth restriction (monitor) (Riester 2015).
Use of spironolactone is associated with menstrual irregularities (dose dependent); contraception is recommended when used in premenopausal women for the treatment of conditions such as hirsutism and acne (AAD [Zaenglein 2016]; Endocrine Society [Martin 2018]).
Patient Education
What is this drug used for?
- It is used to get rid of extra fluid.
- It is used to raise potassium stores in the body.
- It is used to treat heart failure (weak heart).
- It is used to treat high blood pressure.
- It is used to treat some people with high aldosterone levels.
- It is used to treat some kidney problems.
- It may be given to you for other reasons. Talk with the doctor.
Frequently reported side effects of this drug
- Diarrhea
- Fatigue
- Headache
- Hair loss
- Nausea
- Vomiting
- Abdominal cramps
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Fluid and electrolyte problems like mood changes, confusion, muscle pain or weakness, abnormal heartbeat, dizziness, passing out, fast heartbeat, increased thirst, seizures, loss of strength and energy, lack of appetite, unable to pass urine or change in amount of urine passed, dry mouth, dry eyes, nausea, or vomiting.
- Kidney problems like unable to pass urine, blood in the urine, change in amount of urine passed, or weight gain.
- Stevens-Johnson syndrome/toxic epidermal necrolysis like red, swollen, blistered, or peeling skin (with or without fever); red or irritated eyes; or sores in mouth, throat, nose, or eyes.
- Liver problems like dark urine, fatigue, lack of appetite, nausea, abdominal pain, light-colored stools, vomiting, or yellow skin.
- Bleeding like vomiting blood or vomit that looks like coffee grounds; coughing up blood; blood in the urine; black, red, or tarry stools; bleeding from the gums; abnormal vaginal bleeding; bruises without a reason or that get bigger; or any severe bleeding or persistent bleeding.
- Severe dizziness
- Passing out
- Confusion
- Change in balance
- Decreased sex drive
- Sexual dysfunction
- Chills
- Sore throat
- Menstrual changes
- Breast pain
- Enlarged breasts (males)
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.