Boxed Warning
Complex sleep behaviors:
Complex sleep behaviors including sleep-walking, sleep-driving, and engaging in other activities while not fully awake may occur following the use of zolpidem. Some of these events may result in serious injuries, including death. Discontinue zolpidem immediately if a patient experiences a complex sleep behavior.
Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Solution, Oral, as tartrate:
Zolpimist: 5 mg/actuation (7.7 mL [DSC]) [contains benzoic acid, propylene glycol]
Zolpimist: 5 mg/actuation (4.5 mL, 7.7 mL) [contains benzoic acid, propylene glycol; cherry flavor]
Tablet, Oral, as tartrate:
Ambien: 5 mg [contains fd&c red #40, polysorbate 80]
Ambien: 10 mg
Generic: 5 mg, 10 mg
Tablet Extended Release, Oral, as tartrate:
Ambien CR: 6.25 mg
Ambien CR: 12.5 mg [contains fd&c blue #2 (indigotine)]
Generic: 6.25 mg, 12.5 mg
Tablet Sublingual, Sublingual, as tartrate:
Edluar: 5 mg, 10 mg [contains saccharin sodium]
Intermezzo: 1.75 mg, 3.5 mg
Generic: 1.75 mg, 3.5 mg
Pharmacology
Mechanism of Action
Zolpidem, an imidazopyridine hypnotic that is structurally dissimilar to benzodiazepines, enhances the activity of the inhibitory neurotransmitter, γ-aminobutyric acid (GABA), via selective agonism at the benzodiazepine-1 (BZ1) receptor; the result is increased chloride conductance, neuronal hyperpolarization, inhibition of the action potential, and a decrease in neuronal excitability leading to sedative and hypnotic effects. Because of its selectivity for the BZ1 receptor site over the BZ2 receptor site, zolpidem exhibits minimal anxiolytic, myorelaxant, and anticonvulsant properties (effects largely attributed to agonism at the BZ2 receptor site).
Pharmacokinetics/Pharmacodynamics
Absorption
Cmax and AUC is increased by ~45% in females compared to male subjects.
Immediate release and sublingual: Rapid.
Extended release: Biphasic absorption; rapid initial absorption (similar to immediate release product); then provides extended concentrations in the plasma beyond 3 hours postadministration.
Distribution
Vd:
Children 2 to 6 years: 1.8 ± 0.8 L/kg (Blumer 2008).
Children >6 to 12 years: 2.2 ± 1.7 L/kg (Blumer 2008).
Adolescents: 1.2 ± 0.4 L/kg (Blumer 2008).
Adults: 0.54 L/kg (Holm 2000).
Metabolism
Hepatic methylation and hydroxylation via CYP3A4 (~60%), CYP2C9 (~22%), CYP1A2 (~14%), CYP2D6 (~3%), and CYP2C19 (~3%) to 3 inactive metabolites (Holm 2000).
Excretion
Urine (48% to 67%, primarily as metabolites); feces (29% to 42%, primarily as metabolites).
Clearance, apparent:
Children 2 to 6 years: 11.7 ± 7.9 mL/minute/kg (Blumer 2008).
Children >6 to 12 years: 9.7 ± 10.3 mL/minute/kg (Blumer 2008).
Adolescents: 4.8 ± 2 mL/minute/kg (Blumer 2008).
Adults: Intermezzo: Males: 4 mL/minute/kg; Females: 2.7 mL/minute/kg.
Onset of Action
Immediate release: 30 minutes.
Time to Peak
Children 2 to 6 years: Immediate release: 0.9 hours (Blumer 2008).
Children >6 to 12 years: Immediate release: 1.1 hours (Blumer 2008).
Adolescents: Immediate release: 1.3 hours (Blumer 2008).
Adults:
Immediate release: 1.6 hours; 2.2 hours with food.
Extended release: 1.5 hours; 4 hours with food.
Spray: ~0.9 hours.
Sublingual tablet: Edluar: ~1.4 hours, ~1.8 hours with food; Intermezzo: 0.6 to 1.3 hours, ~3 hours with food.
Duration of Action
Immediate release: 6 to 8 hours.
Half-Life Elimination
Children 2 to 6 years: Immediate release: 1.8 hours (Blumer 2008).
Children >6 years and Adolescents: Immediate release: 2.3 hours (Blumer 2008).
Adults:
Immediate release, Extended release: ~2.5 hours (range: 1.4 to 4.5 hours); Cirrhosis: Up to 9.9 hours; Elderly: Prolonged up to 32%.
Spray: ~3 hours (range: 1.7 to 8.4).
Sublingual tablet: ~3 hours (range: 1.4 to 6.7 hours).
Protein Binding
~93%.
Use in Specific Populations
Special Populations: Hepatic Function Impairment
Cmax and AUC were found to be 2 and 5 times higher, respectively, in hepatically compromised patients. The mean half-life in cirrhotic patients of 9.9 hours was greater than that observed in normal subjects of 2.2 hours.
Special Populations: Elderly
Immediate release: Cmax, half-life, and AUC were significantly increased when compared with results in younger adults.
Extended release: Mean Cmax and mean AUC are 70.6 ng/mL and 413 ng•h/mL, respectively, while the median Tmax is 2 hours.
Special Populations: Gender
Cmax and AUC were higher when comparing the same dose in women with men. Women clear zolpidem from the body at a lower rate than men. In geriatric patients, clearance is similar between men and women.
Use: Labeled Indications
Insomnia:
IR and sublingual tablets (Edluar only) and oral spray: Short-term treatment of insomnia with difficulty of sleep onset
ER tablet: Treatment of insomnia with difficulty of sleep onset and/or sleep maintenance
Sublingual tablet (Intermezzo only): "As needed" treatment of insomnia when middle-of-the-night awakening is followed by difficulty returning to sleep and the patient has ≥4 hours of sleep time remaining
Sublingual tablet (Sublinox only [Canadian product]): Short-term treatment of insomnia (with difficulty of sleep onset, frequent awakenings, and/or early awakenings)
Contraindications
Hypersensitivity to zolpidem or any component of the formulation; patients who have experienced complex sleep behaviors after taking zolpidem
Canadian labeling: Additional contraindications (not in US labeling): Significant obstructive sleep apnea syndrome and acute and/or severe impairment of respiratory function; myasthenia gravis; severe hepatic impairment; personal or family history of sleepwalking
Dosage and Administration
Dosing: Adult
Insomnia: Oral: Note: Intended for short-term use (≤4 to 8 weeks), preferably in conjunction with nonpharmacologic therapies (ACP [Qaseem 2016]; ESRS [Riemann 2017]). Chronic use should be limited to cases where nonpharmacologic treatments are not available or not effective and benefits are felt to outweigh risks (AASM [Sateia 2017]). Some experts advise against extended use of pharmacologic therapy for insomnia (ACP [Qaseem 2016]). Use of the higher dose can increase the risk of next-day impairment of driving and activities requiring full alertness.
Sleep-onset insomnia:
ER tablet: Initial: 6.25 mg (females) or 6.25 to 12.5 mg (males) immediately before bedtime with at least 7 to 8 hours of planned sleep before waking. Use lowest effective dose, not to exceed 12.5 mg.
IR tablet, spray, sublingual tablet: Initial: 5 mg (females) or 5 to 10 mg (males) immediately before bedtime with at least 7 to 8 hours of planned sleep before waking. Use lowest effective dose, not to exceed 10 mg.
Sleep-maintenance insomnia, 7 to 8 hours planned sleep:
ER tablet: Initial: 6.25 mg (females) or 6.25 to 12.5 mg (males) immediately before bedtime with at least 7 to 8 hours of planned sleep before waking. Use lowest effective dose, not to exceed 12.5 mg.
IR tablet, spray, sublingual tablet: Initial: 5 mg (females) or 5 to 10 mg (males) immediately before bedtime with at least 7 to 8 hours of planned sleep before waking. Use lowest effective dose, not to exceed 10 mg.
Sleep-maintenance insomnia, awakening with 4 hours planned sleep: IR sublingual tablet: 1.75 mg (females) or 1.75 to 3.5 mg (males) once per night upon awakening in the middle of the night with 4 hours of planned sleep remaining.
Discontinuation of therapy: For patients taking higher doses of zolpidem (eg, 10 or 12.5 mg/day) for an extended period, slowly tapering zolpidem in conjunction with providing Cognitive Behavioral Therapy for Insomnia is encouraged. Zolpidem can be reduced by ~25% of the original dose each week or every other week (Belanger 2009).
Dosing: Geriatric
Avoid use (Beers Criteria [AGS 2019]).
Dosing: Pediatric
Note: The lowest effective dose should be used; higher doses may be more likely to impair next-morning activities.
Insomnia:
Children and Adolescents ≤17 years: Limited data available; efficacy results variable and have not been demonstrated in randomized placebo-controlled trials (Anand 2017). Oral: Immediate-release tablets: Usual reported dose: 0.25 mg/kg at bedtime; maximum dose: 10 mg/dose (Blumer 2008; Blumer 2009; Hanna 2018); dosing based on reported experience from an open-label, dose escalation pharmacokinetic evaluation showed zolpidem was well-tolerated in pediatric patients 2 to 18 years of age and recommended a dose of 0.25 mg/kg at bedtime for evaluation in future efficacy trials (Blumer 2008). However, zolpidem has not been shown to be effective in a randomized placebo-controlled trial (n=201) of children aged 6 to 17 years with ADHD-associated insomnia; zolpidem 0.25 mg/kg/dose (maximum dose: 10 mg) administered nightly did not decrease sleep latency; in addition, hallucinations occurred in 7.4% of patients (Blumer 2009). A comparative, randomized controlled trial of zolpidem and haloperidol in pediatric burn patients (n=40, mean age: 9.4 ± 0.7 years) showed zolpidem dosed at 0.5 mg/kg nightly for 1 week (maximum dose: 20 mg) minimally increased Stage 3/4 sleep and REM but not total sleep time; the authors no longer use zolpidem to try to improve sleep in their pediatric burn patients (Armour 2008). A retrospective study compared effectiveness of zolpidem (no dose noted in study) in pediatric burn patients (n=46, mean age: 11 ± 3.7 years) with and without ADHD and found that sleep dysfunction was similar between the groups and those with ADHD required a sleep medication change sooner, concluding that zolpidem was not an effective drug in managing sleep in pediatric burn patients with or without ADHD (Cronin 2015). A prospective, randomized double-blind clinical trial of children between ages 2 to 9 years reported that zolpidem at 0.25 mg/kg (maximum dose: 10 mg/dose) was similar to midazolam with regards to anxiety scoring and inferior with regard to mask acceptance score when used as premedication for perioperative anxiety (Hanna 2018).
Adolescents ≥18 years (non-debilitated patients): Note: The lowest effective dose should be used; higher doses may be more likely to impair next morning activities.
Oral:
Immediate-release tablet (eg, Ambien), spray (Zolpimist): 5 mg (females) or 5 to 10 mg (males) immediately before bedtime; maximum dose: 10 mg/dose
Extended-release tablet (eg, Ambien CR): 6.25 mg (females) or 6.25 to 12.5 mg (males) immediately before bedtime; maximum dose: 12.5 mg/dose
Sublingual tablet:
Edluar: 5 mg (females) or 5 to 10 mg (males) immediately before bedtime; maximum daily dose: 10 mg/day
Intermezzo: Note: Should be taken if patient awakens in middle of night, has difficulty returning to sleep, and has at least 4 hours left before waking.
Females: 1.75 mg once per night as needed; maximum dose: 1.75 mg/night
Males: 3.5 mg once per night as needed; maximum dose: 3.5 mg/night
Dosage adjustment with concomitant CNS depressants: Females and males: 1.75 mg once per night as needed; dose adjustment of concomitant CNS depressant(s) may be necessary
Administration
Oral: Administer immediately before bedtime due to rapid onset of action. Regardless of dosage form, do not administer with or immediately after a meal (may delay onset). With the exception of Intermezzo, zolpidem should be taken as a single dose at bedtime with at least 7 to 8 hours remaining before planned time of awakening and should not be readministered during the same night. Intermezzo should be taken in bed if patient awakes in the middle of the night (ie, if ≥4 hours left before waking) and there is difficulty in returning to sleep.
ER tablet: Swallow tablet whole; do not divide, crush, or chew.
Sublingual tablet: Place sublingual tablet under the tongue and allow to disintegrate; do not swallow or administer Edluar or Sublinox with water.
Oral spray: Spray directly into the mouth over the tongue. Prior to initial use, prime pump by spraying 5 times. If pump is not used for at least 14 days, reprime pump with 1 spray.
Dietary Considerations
Do not administer with or immediately after a meal (may delay onset).
Storage
IR and sublingual tablets: Store at 20°C to 25°C (68°F to 77°F). Protect sublingual tablets from light and moisture.
ER tablet: Store at 15°C to 25°C (59°F to 77°F); limited excursions permitted up to 30°C (86°F).
Oral spray: Store upright at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F). Do not freeze. Avoid prolonged exposure to temperatures >30°C (86°F).
Sublingual tablet (Sublinox [Canadian product]): Store at 15°C to 30°C (59°F to 86°F); protect from light and moisture.
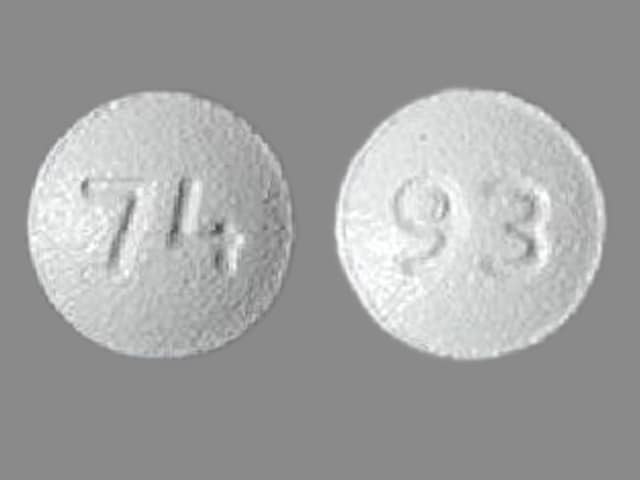
Zolpidem Images
Drug Interactions
Alizapride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Azelastine (Nasal): CNS Depressants may enhance the CNS depressant effect of Azelastine (Nasal). Avoid combination
Blonanserin: CNS Depressants may enhance the CNS depressant effect of Blonanserin. Consider therapy modification
Bosentan: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Brimonidine (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromopride: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Bromperidol: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
Buprenorphine: CNS Depressants may enhance the CNS depressant effect of Buprenorphine. Management: Consider reduced doses of other CNS depressants, and avoiding such drugs in patients at high risk of buprenorphine overuse/self-injection. Initiate buprenorphine at lower doses in patients already receiving CNS depressants. Consider therapy modification
Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Cannabis: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
CarBAMazepine: Zolpidem may enhance the CNS depressant effect of CarBAMazepine. CarBAMazepine may decrease the serum concentration of Zolpidem. Management: Monitor zolpidem response closely. Reduce the Intermezzo brand sublingual zolpidem dose to 1.75 mg for men who are also receiving carbamazepine. No such dose change is recommended for women. Monitor therapy
Chlormethiazole: May enhance the CNS depressant effect of CNS Depressants. Management: Monitor closely for evidence of excessive CNS depression. The chlormethiazole labeling states that an appropriately reduced dose should be used if such a combination must be used. Consider therapy modification
Chlorphenesin Carbamate: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Ciprofloxacin (Systemic): May increase the serum concentration of Zolpidem. Management: Consider avoiding the combination of ciprofloxacin and zolpidem if possible. If combined, monitor for signs of zolpidem toxicity (eg, somnolence, dizziness, lethargy). Consider therapy modification
CNS Depressants: May enhance the CNS depressant effect of Zolpidem. Management: Reduce the Intermezzo brand sublingual zolpidem adult dose to 1.75 mg for men who are also receiving other CNS depressants. No such dose change is recommended for women. Avoid use with other CNS depressants at bedtime; avoid use with alcohol. Consider therapy modification
CYP3A4 Inducers (Moderate): May decrease the serum concentration of Zolpidem. Monitor therapy
CYP3A4 Inducers (Strong): May decrease the serum concentration of Zolpidem. Monitor therapy
CYP3A4 Inhibitors (Strong): May increase the serum concentration of Zolpidem. Monitor therapy
Dabrafenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Seek alternatives to the CYP3A4 substrate when possible. If concomitant therapy cannot be avoided, monitor clinical effects of the substrate closely (particularly therapeutic effects). Consider therapy modification
Deferasirox: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Dimethindene (Topical): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Dronabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Droperidol: May enhance the CNS depressant effect of CNS Depressants. Management: Consider dose reductions of droperidol or of other CNS agents (eg, opioids, barbiturates) with concomitant use. Exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Consider therapy modification
Enzalutamide: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Concurrent use of enzalutamide with CYP3A4 substrates that have a narrow therapeutic index should be avoided. Use of enzalutamide and any other CYP3A4 substrate should be performed with caution and close monitoring. Consider therapy modification
Erdafitinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Flunitrazepam: CNS Depressants may enhance the CNS depressant effect of Flunitrazepam. Consider therapy modification
FluvoxaMINE: May enhance the CNS depressant effect of Zolpidem. FluvoxaMINE may increase the serum concentration of Zolpidem. Monitor therapy
HYDROcodone: CNS Depressants may enhance the CNS depressant effect of HYDROcodone. Management: Avoid concomitant use of hydrocodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Itraconazole: May increase the serum concentration of Zolpidem. Monitor therapy
Ivosidenib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Kava Kava: May enhance the adverse/toxic effect of CNS Depressants. Monitor therapy
Ketoconazole (Systemic): May increase the serum concentration of Zolpidem. Management: Consider using a lower starting dose of zolpidem in patients receiving ketoconazole and monitor for increased zolpidem effects/toxicities if these agents are combined. Consider therapy modification
Lemborexant: May enhance the CNS depressant effect of CNS Depressants. Management: Dosage adjustments of lemborexant and of concomitant CNS depressants may be necessary when administered together because of potentially additive CNS depressant effects. Close monitoring for CNS depressant effects is necessary. Consider therapy modification
Lofexidine: May enhance the CNS depressant effect of CNS Depressants. Management: Drugs listed as exceptions to this monograph are discussed in further detail in separate drug interaction monographs. Monitor therapy
Lorlatinib: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Avoid concurrent use of lorlatinib with any CYP3A4 substrates for which a minimal decrease in serum concentrations of the CYP3A4 substrate could lead to therapeutic failure and serious clinical consequences. Consider therapy modification
Magnesium Sulfate: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Melatonin: May enhance the sedative effect of Hypnotics (Nonbenzodiazepine). Monitor therapy
Methotrimeprazine: CNS Depressants may enhance the CNS depressant effect of Methotrimeprazine. Methotrimeprazine may enhance the CNS depressant effect of CNS Depressants. Management: Reduce adult dose of CNS depressant agents by 50% with initiation of concomitant methotrimeprazine therapy. Further CNS depressant dosage adjustments should be initiated only after clinically effective methotrimeprazine dose is established. Consider therapy modification
MetyroSINE: CNS Depressants may enhance the sedative effect of MetyroSINE. Monitor therapy
Minocycline (Systemic): May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Mitotane: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Management: Doses of CYP3A4 substrates may need to be adjusted substantially when used in patients being treated with mitotane. Consider therapy modification
Nabilone: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Orphenadrine: CNS Depressants may enhance the CNS depressant effect of Orphenadrine. Avoid combination
Oxomemazine: May enhance the CNS depressant effect of CNS Depressants. Avoid combination
OxyCODONE: CNS Depressants may enhance the CNS depressant effect of OxyCODONE. Management: Avoid concomitant use of oxycodone and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Paraldehyde: CNS Depressants may enhance the CNS depressant effect of Paraldehyde. Avoid combination
Perampanel: May enhance the CNS depressant effect of CNS Depressants. Management: Patients taking perampanel with any other drug that has CNS depressant activities should avoid complex and high-risk activities, particularly those such as driving that require alertness and coordination, until they have experience using the combination. Consider therapy modification
Piribedil: CNS Depressants may enhance the CNS depressant effect of Piribedil. Monitor therapy
Pramipexole: CNS Depressants may enhance the sedative effect of Pramipexole. Monitor therapy
RifAMPin: May decrease the serum concentration of Zolpidem. Avoid combination
Ritonavir: May increase the serum concentration of Zolpidem. Monitor therapy
ROPINIRole: CNS Depressants may enhance the sedative effect of ROPINIRole. Monitor therapy
Rotigotine: CNS Depressants may enhance the sedative effect of Rotigotine. Monitor therapy
Rufinamide: May enhance the adverse/toxic effect of CNS Depressants. Specifically, sleepiness and dizziness may be enhanced. Monitor therapy
Sarilumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Selective Serotonin Reuptake Inhibitors: CNS Depressants may enhance the adverse/toxic effect of Selective Serotonin Reuptake Inhibitors. Specifically, the risk of psychomotor impairment may be enhanced. Monitor therapy
Siltuximab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Sodium Oxybate: Hypnotics (Nonbenzodiazepine) may enhance the CNS depressant effect of Sodium Oxybate. Avoid combination
St John's Wort: May decrease the serum concentration of Zolpidem. Avoid combination
Suvorexant: CNS Depressants may enhance the CNS depressant effect of Suvorexant. Management: Dose reduction of suvorexant and/or any other CNS depressant may be necessary. Use of suvorexant with alcohol is not recommended, and the use of suvorexant with any other drug to treat insomnia is not recommended. Consider therapy modification
Tapentadol: May enhance the CNS depressant effect of CNS Depressants. Management: Avoid concomitant use of tapentadol and benzodiazepines or other CNS depressants when possible. These agents should only be combined if alternative treatment options are inadequate. If combined, limit the dosages and duration of each drug. Consider therapy modification
Tetrahydrocannabinol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Tetrahydrocannabinol and Cannabidiol: May enhance the CNS depressant effect of CNS Depressants. Monitor therapy
Thalidomide: CNS Depressants may enhance the CNS depressant effect of Thalidomide. Avoid combination
Tocilizumab: May decrease the serum concentration of CYP3A4 Substrates (High risk with Inducers). Monitor therapy
Test Interactions
Increased aminotransferase [ALT/AST], bilirubin (S); decreased RAI uptake
Adverse Reactions
As reported with oral administration, unless otherwise noted.
>10%: Central nervous system: Headache (oral: 7% to 19%; sublingual: 3%), drowsiness (2% to 15%), dizziness (1% to 12%)
1% to 10%:
Cardiovascular: Palpitations (2%), chest discomfort (1%), chest pain (1%), increased blood pressure (1%), edema (≤1%), hypertension (≤1%), orthostatic hypotension (≤1%), syncope (≤1%), tachycardia (≤1%)
Central nervous system: Anxiety (2% to 6%), hallucination (4%), disorientation (3%), fatigue (oral: 3%; sublingual: 1%), intoxicated feeling (3%), lethargy (3%), memory impairment (3%), balance impairment (2%), depression (2%), disturbance in attention (2%), hypoesthesia (2%), psychomotor retardation (2%), vertigo (2%), confusion (>1%), euphoria (>1%), insomnia (>1%), abnormal dreams (1%), amnesia (1%), ataxia (1%), depersonalization (1%), disinhibition (1%), eating disorder (1%; binge eating), increased body temperature (1%), paresthesia (1%), sleep disorder (1%), stress (1%), agitation (≤1%), cerebrovascular disease (≤1%), cognitive dysfunction (≤1%), dysarthria (≤1%), emotional lability (≤1%), falling (≤1%), illusion (≤1%), malaise (≤1%), migraine (≤1%), nervousness (≤1%), speech disturbance (≤1%), stupor (≤1%)
Dermatologic: Skin rash (1% to 2%), diaphoresis (≤1%), pallor (≤1%), pruritus (≤1%), urticaria (≤1%), wrinkling of skin (1%)
Endocrine & metabolic: Heavy menstrual bleeding (1%), hyperglycemia (≤1%), increased thirst (≤1%), menstrual disease (≤1%)
Gastrointestinal: Nausea (7%), xerostomia (3%), diarrhea (1% to 3%), constipation (2%), dyspepsia (>1%), hiccups (>1%), abdominal distress (1%), abdominal tenderness (1%), change in appetite (1%), frequent bowel movements (1%), gastroenteritis (1%), gastroesophageal reflux disease (1%), vomiting (1%), anorexia (≤1%), dysgeusia (≤1%), dysphagia (≤1%), flatulence (≤1%)
Genitourinary: Urinary tract infection (>1%), cystitis (≤1%), urinary incontinence (≤1%), vaginitis (≤1%)
Hematologic & oncologic: Bruise (1%)
Hepatic: Abnormal hepatic function tests (≤1%), increased serum alanine aminotransferase (≤1%)
Hypersensitivity: Hypersensitivity reaction (4%)
Infection: Influenza (3%), infection (≤1%)
Neuromuscular & skeletal: Myalgia (4%), back pain (3% to 4%), arthralgia (>1%), asthenia (1%), neck pain (1%), arthritis (≤1%), lower limb cramp (≤1%), tremor (≤1%)
Ophthalmic: Visual disturbance (1% to 3%; including altered depth perception), blurred vision (2%), eye redness (2%), diplopia (>1%), asthenopia (1%), eye irritation (≤1%), eye pain (≤1%), scleritis (≤1%)
Otic: Labyrinthitis (1%), tinnitus (1%)
Respiratory: Sinusitis (4%), pharyngitis (3%), flu-like symptoms (1% to 2%), lower respiratory tract infection (>1%), upper respiratory tract infection (>1%), throat irritation (1%), bronchitis (≤1%), cough (≤1%), dyspnea (≤1%), rhinitis (≤1%)
Miscellaneous: Fever (≤1%), trauma (≤1%)
<1%, postmarketing, and/or case reports: Abnormal gait, abnormal lacrimation, abnormality in thinking, abscess, accommodation disturbance, acne vulgaris, acute myocardial infarction, acute renal failure, aggressive behavior, alteration of saliva, altered sense of smell, anaphylactic shock, anaphylaxis, anemia, angina pectoris, angioedema, apathy, arteritis, behavioral changes, breast fibroadenosis, breast neoplasm, bronchospasm, bullous rash, cardiac arrhythmia, central nervous system depression, cholestatic hepatitis, circulatory shock, complex sleep-related disorder, conjunctivitis, corneal ulcer, decreased libido, delusion, dementia, dental caries, dermatitis, drug tolerance, drug withdrawal, dysphasia, dysuria, enteritis, epistaxis, eructation, esophageal spasm, exacerbation of hypertension, extrasystoles, facial edema, flushing, furunculosis, gastritis, glaucoma, gout, hemorrhoids, hepatic injury, hepatocellular hepatitis, herpes simplex infection, herpes zoster infection, hot flash, hyperbilirubinemia, hypercholesteremia, hyperhemoglobinemia, hyperlipidemia, hypokinesia, hypotension, hypotonia, hypoxia, hysteria, impotence, increased appetite, increased blood urea nitrogen, increased erythrocyte sedimentation rate, increased serum alkaline phosphatase, increased serum aspartate aminotransferase, intestinal obstruction, laryngitis, leukopenia, lymphadenopathy, macrocytic anemia, manic reaction, mastalgia, myasthenia, neuralgia, neuritis, neuropathy, neurosis, nocturia, numbness of tongue, osteoarthritis, otitis externa, otitis media, pain, panic disorder, paresis, periorbital edema, personality disorder, phlebitis, photopsia, pneumonia, polyuria, pulmonary edema, pulmonary embolism, purpuric disease, pyelonephritis, rectal hemorrhage, renal pain, respiratory depression, restless leg syndrome, rigors, sciatica, sialorrhea, skin photosensitivity, strange feeling, suicidal ideation, suicidal tendencies, tendonitis, tenesmus, tetany, thrombosis, urinary frequency, urinary retention, varicose veins, ventricular tachycardia, weight loss, yawning
Warnings/Precautions
Concerns related to adverse effects:
- Abnormal thinking/behavioral changes: Hypnotics/sedatives have been associated with abnormal thinking and behavior changes including decreased inhibition (eg, aggressiveness and extroversion that seemed out of character), bizarre behavior, agitation, visual and auditory hallucinations, and depersonalization. These changes may occur unpredictably and may indicate previously unrecognized psychiatric disorders; evaluate appropriately.
- Complex sleep behaviors: [US Boxed Warning]: Complex sleep behaviors including sleep-walking, sleep-driving, and engaging in other activities while not fully awake may occur following the use of zolpidem. Some of these events may result in serious injuries, including death. Other complex sleep behaviors (eg, preparing and eating food, making phone calls, having sex) while asleep have also been reported. Patients usually do not remember these events. May occur with first use and at recommended dosages with or without the use of alcohol or other CNS depressants. Discontinue immediately if a patient experiences a complex sleep behavior; use is contraindicated in patients who have experienced these events.
- CNS depression: May cause CNS depression impairing physical and mental capabilities; patients must be cautioned about performing tasks which require mental alertness (operating machinery or driving). The risk of next-day psychomotor impairment is increased if patient is unable to stay in bed for a full night of sleep (7 to 8 hours); if coadministered with other CNS depressants and/or taken with other drugs that increase blood levels of zolpidem; or if a higher than recommended dose is taken. Dose adjustment may be necessary if taking concomitant CNS depressants; use with alcohol is not recommended.
- Hypersensitivity reactions: Hypersensitivity reactions, including anaphylaxis as well as angioedema, have been reported after taking the first or subsequent doses. Do not rechallenge patient if such reactions occur.
Disease-related concerns:
- Depression: Use with caution in patients with depression; worsening of depression, including suicide or suicidal ideation has been reported with the use of hypnotics. Intentional overdose may be an issue in this population. The minimum dose that will effectively treat the individual patient should be used. Prescriptions should be written for the smallest quantity consistent with good patient care.
- Drug abuse: Use with caution in patients with a history of drug dependence. Risk of abuse is increased in patients with a history or family history of alcohol or drug abuse or mental illness.
- Hepatic impairment: GABA agonists, including zolpidem, have been associated with precipitation of hepatic encephalopathy in patients with hepatic impairment. Patients with hepatic impairment do not clear zolpidem as rapidly as patients with normal hepatic function. Use with caution in patients with mild to moderate hepatic impairment; dose adjustment recommended. Avoid use of immediate and extended-release tablets in patients with severe hepatic impairment; may result in encephalopathy.
- Myasthenia gravis: Use with caution in patients with myasthenia gravis.
- Respiratory disease: Use with caution in patients with respiratory compromise, COPD, or sleep apnea.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Debilitated: Use with caution in debilitated patients; potential for oversedation, impaired coordination, and confusion with use; dosage adjustment recommended.
- Elderly: Use with caution in elderly patients; dose adjustment recommended. Monitor for impaired cognitive and/or motor performance, confusion, and potential for falling.
- Females: Dosage adjustment is recommended for females; pharmacokinetic studies involving zolpidem showed a significant increase in maximum concentration and exposure in females compared to males at the same dose.
- Pediatric: When studied for the unapproved use of insomnia associated with ADHD in children, a higher incidence (~7%) of hallucinations was reported. In addition, sleep latency did not decrease compared to placebo.
Dosage form specific issues:
- Polysorbate 80: Some dosage forms may contain polysorbate 80 (also known as Tweens). Hypersensitivity reactions, usually a delayed reaction, have been reported following exposure to pharmaceutical products containing polysorbate 80 in certain individuals (Isaksson 2002; Lucente 2000; Shelley 1995). Thrombocytopenia, ascites, pulmonary deterioration, and renal and hepatic failure have been reported in premature neonates after receiving parenteral products containing polysorbate 80 (Alade 1986; CDC 1984). See manufacturer's labeling.
Other warnings/precautions:
- Appropriate use: Symptomatic treatment of insomnia should be initiated only after careful evaluation of potential causes of sleep disturbance. Failure of sleep disturbance to resolve after 7 to 10 days may indicate the need for psychiatric and/or medical illness reevaluation.
- Rapid onset: Because of the rapid onset of action, administer Intermezzo immediately prior to bedtime, after the patient has gone to bed and is having difficulty falling asleep, or during the middle of the night when at least 4 hours are left before waking.
- Withdrawal: Abrupt discontinuance or rapid dose decrease may lead to withdrawal symptoms.
Monitoring Parameters
Daytime alertness; fall risk, respiratory rate (patients with compromised respiration); behavior profile; tolerance, abuse, and dependence; reevaluate if insomnia persists after 7 to 10 days of use.
Pregnancy
Pregnancy Considerations
Zolpidem crosses the placenta (Juric 2009).
Severe neonatal respiratory depression and sedation have been reported when zolpidem was used at the end of pregnancy, especially when used concurrently with other CNS depressants. Children born of mothers taking sedative/hypnotics may be at risk for withdrawal; neonatal flaccidity has been reported in infants following maternal use of sedative/hypnotics during pregnancy. Additional adverse effects to the fetus/newborn have been noted in some studies (Sharma 2011; Wang 2010; Wikner 2011). Exposed neonates should be monitored for excess sedation, hypotonia, and respiratory depression.
Patient Education
What is this drug used for?
- It is used to treat sleep problems.
Frequently reported side effects of this drug
- Dizziness
- Fatigue
- Headache
- Nausea
- Diarrhea
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Mood changes
- Behavioral changes
- Depression
- Thoughts of suicide
- Sensing things that seem real but are not
- Confusion
- Impaired thinking
- Difficulty breathing
- Slow breathing
- Shallow breathing
- Change in balance
- Vision changes
- Trouble with memory
- Severe loss of strength and energy
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.