Dosage Forms
Excipient information presented when available (limited, particularly for generics); consult specific product labeling. [DSC] = Discontinued product
Capsule Extended Release 24 Hour, Oral:
Theo-24: 100 mg [contains fd&c yellow #6 (sunset yellow)]
Theo-24: 200 mg [contains fd&c yellow #10 (quinoline yellow)]
Theo-24: 300 mg [contains brilliant blue fcf (fd&c blue #1), fd&c red #40]
Theo-24: 400 mg [contains fd&c red #40]
Elixir, Oral:
Elixophyllin: 80 mg/15 mL (473 mL) [contains alcohol, usp, fd&c red #40, saccharin sodium; mixed fruit flavor]
Solution, Intravenous:
Generic: 400 mg (500 mL)
Solution, Oral:
Generic: 80 mg/15 mL (15 mL, 473 mL)
Tablet Extended Release 12 Hour, Oral:
Theochron: 100 mg, 200 mg, 300 mg [scored]
Generic: 100 mg [DSC], 200 mg [DSC], 300 mg, 450 mg
Tablet Extended Release 24 Hour, Oral:
Generic: 400 mg, 600 mg
Pharmacology
Mechanism of Action
Theophylline has two distinct actions; smooth muscle relaxation (ie, bronchodilation) and suppression of the response of the airways to stimuli (ie, non-bronchodilator prophylactic effects). Bronchodilation is mediated by inhibition of two isoenzymes, phosphodiesterase (PDE III and, to a lesser extent, PDE IV) while non-bronchodilation effects are mediated through other molecular mechanisms. Theophylline increases the force of contraction of diaphragmatic muscles through enhancement of calcium uptake through adenosine-mediated channels.
Pharmacokinetics/Pharmacodynamics
Absorption
Oral: Oral (solution and immediate release): Rapid and complete
Distribution
~0.45 L/kg based on ideal body weight; distributes poorly into body fat; Vd may increase in premature neonates, hepatic cirrhosis, acidemia (uncorrected), elderly, and third trimester of pregnancy.
Metabolism
Hepatic via demethylation (CYP 1A2) and hydroxylation (CYP 2E1 and 3A4); forms active metabolites (caffeine and 3-methylxanthine
Excretion
Urine (~50% as unchanged drug [Neonates]; ~10% as unchanged drug [Infants >3 months, Adolescents, and Adults])
Clearance: Certain conditions may significantly alter theophylline clearance; severe and potentially fatal theophylline toxicity may occur if reduced theophylline clearance occurs.
Decreased theophylline clearance: Neonates; infants <3 months with decreased renal function; infants <1 year; elderly >60 years; acute pulmonary edema, cor pulmonale; fever (≥ 102°F for ≥24 hours or lesser temperature elevations for longer periods); heart failure; hepatic impairment (eg, cirrhosis, acute hepatitis, cholestasis); hypothyroidism; patients following cessation of smoking; sepsis with multiple organ failure; shock; third trimester of pregnancy.
Increased theophylline clearance: Hyperthyroidism; cystic fibrosis; smoking (ie, marijuana or tobacco).
Onset of Action
IV: <30 minutes
Time to Peak
Serum: Oral (solution and immediate release): 1 to 2 hours; IV: Within 30 minutes
Half-Life Elimination
Highly variable and dependent upon age, hepatic function, cardiac function, lung disease, and smoking history (Hendeles 1995):
Premature infants, postnatal age 3 to 15 days: 30 hours (range: 17 to 43 hours)
Premature infants, postnatal age 25 to 57 days: 20 hours (range: 9.4 to 30.6 hours)
Term infants, postnatal age 1 to 2 days: 25.7 hours (range: 25 to 26.5 hours)
Term infants, postnatal age 3 to 30 weeks: 11 hours (range: 6 to 29 hours)
Children 1 to 4 years: 3.4 hours (range: 1.2 to 5.6 hours)
Children and Adolescents 6 to 17 years: 3.7 hours (range: 1.5 to 5.9 hours)
Adults ≥18 years to ≤60 years (nonsmoking, asthmatic, otherwise healthy): 8.7 hours (range: 6.1 to 12.8 hours)
Elderly >60 years (nonsmoking, healthy): 9.8 hours (range: 1.6 to 18 hours)
Protein Binding
~40%, primarily to albumin; decreased in neonates (due to a greater percentage of fetal albumin), hepatic cirrhosis, acidemia (uncorrected), third trimester of pregnancy, and elderly
Use: Labeled Indications
Reversible airflow obstruction:
Oral: Treatment of symptoms and reversible airflow obstruction associated with chronic asthma, or other chronic lung diseases (eg, emphysema, chronic bronchitis).
Injection: Treatment of acute exacerbations of the symptoms and reversible airflow obstruction associated with asthma and other chronic lung diseases (eg, chronic bronchitis, emphysema) as an adjunct to inhaled beta-2 selective agonists and systemically administered corticosteroids. Guideline recommendations:
Guideline recommendations:
Asthma: The 2018 Global Initiative for Asthma Guidelines (GINA) and the 2007 National Heart, Lung and Blood Institute Asthma Guidelines recommends against oral theophylline as a long-term control medication for asthma in children ≤5 years of age. Additionally, GINA guidelines do not recommend oral theophylline for asthma in children 6 to 11 years of age. Oral theophylline is a potential alternative option (not preferred) in adolescents and adults as a long-term control medication in mild asthma or as an add-on long-term control medication in moderate to severe asthma; however, a stepwise approach using inhaled corticosteroids (+/- inhaled long-acting beta agonists depending on asthma severity) is preferred to theophylline due to efficacy concerns and potential for adverse events (GINA 2018). Both guidelines recommend against theophylline for the treatment of asthma exacerbations due to poor efficacy and safety concerns (GINA 2018; NAEPP 2007).
COPD: The Global Initiative for Chronic Obstructive Lung Disease Guidelines (2018) suggest that while higher doses of slow release formulations of theophylline have been proven to be effective for use in COPD, it is not a preferred agent for COPD exacerbations due to its potential for toxicity. There is evidence for a modest bronchodilator effect when used for stable COPD.
Use: Off Label
Bradycardia, heart transplantationcyes
Data from small observational studies suggest that theophylline may be beneficial for the treatment of bradycardia following heart transplantation Bertolet 1996, Ellenbogen 1988, Redmond 1993.
Based on the 2018 American College of Cardiology/American Heart Association/Heart Rhythm Society (ACC/AHA/HRS) Guideline on the evaluation and management of patients with bradycardia and cardiac conduction delay and the 2010 International Society of Heart and Lung Transplantation guidelines for the care of heart transplant recipients, theophylline is recommended and may be effective for the treatment of sinus bradycardia following heart transplantation.
Reversal of dipyridamole-, or regadenoson-induced adverse reactions (eg, angina, hypotension) during nuclear cardiac stress testing (alternative agent)c
For dipyridamole- or regadenoson-induced adverse reactions when aminophylline is not available (eg, due to shortage), theophylline may be used as an alternative Johnson 2011, Singleton 2018. Reversal of adenosine should rarely be required given adenosine's short half-life ASNC [Henzlova 2016].
Contraindications
Hypersensitivity to theophylline or any component of the formulation; allergy to corn-related products (injection only).
Canadian labeling: Additional contraindications (not in US labeling): Hypersensitivity to xanthine derivatives; coronary artery disease (where cardiac stimulation might prove harmful); peptic ulcers; coadministration with ephedrine in children.
Dosage and Administration
Dosing: Adult
Note: Individualize dose based on steady-state serum concentrations; use ideal body weight (theophylline distributes poorly into body fat) to calculate dose.
Bradycardia, heart transplantation (off-label use): Based on limited data and clinical experience: Oral: Initial: 150 mg twice daily; titrate as needed based on heart rate response and tolerability; daily doses of up to 900 mg/day have been reported (ACC/AHA/HRS [Kusumoto 2018]; Bertolet 1996; Redmond 1993).
Reversible airflow obstruction, acute symptoms:
Loading dose: IV, Oral (immediate release solution):
Asthma exacerbations: The treatment of asthma exacerbations with theophylline is not supported or recommended by current clinical practice guidelines (GINA 2018; NAEPP 2007).
COPD treatment: The treatment of acute COPD with theophylline IV is not supported or recommended by current clinical practice guidelines due to significant side effects (GOLD 2018).
Patients who have not received theophylline in the previous 24 hours: 4.6 mg/kg/dose IV (preferred route) or 5 mg/kg orally (immediate release only [oral solution]). Note: Loading dose intended to achieve a serum level of ~10 mcg/mL (range: 5 to 16 mcg/mL). On the average, for every 1 mg/kg theophylline given, blood levels will rise 2 mcg/mL. Obtain theophylline serum concentration 30 minutes (IV) or 24 hours (oral) after loading dose (when distribution is complete) to assess the need for and size of subsequent loading doses (and for guidance of continuing therapy).
Patients who have received theophylline in the previous 24 hours: A loading dose should not be given before obtaining a serum theophylline concentration. The loading dose should be calculated as follows:
Dose = (desired serum theophylline concentration - measured serum theophylline concentration) (Vd)
Maintenance: Continuous IV infusion: Note: Dosing presented is to achieve a target concentration of 10 mcg/mL unless otherwise noted. Lower initial doses may be required in patients with reduced theophylline clearance. Dosage should be adjusted according to serum level measurements during the first 12- to 24-hour period.
Adults ≤60 years: 0.4 mg/kg/hour; maximum: 900 mg/day unless serum levels indicate need for larger dose.
Adults >60 years: 0.3 mg/kg/hour; maximum: 400 mg/day unless serum levels indicate need for larger dose.
Cardiac decompensation, cor pulmonale, sepsis with multiorgan failure, or shock: 0.2 mg/kg/hour; maximum: 400 mg/day, unless serum levels indicate need for larger dose.
Reversible airflow obstruction, chronic conditions: Oral: Note: Increase dose only if tolerated and if needed. Consider lowering dose or using a slower titration if caffeine-like adverse events occur. May use smaller doses more frequently in patients requiring higher than average doses prevent breakthrough symptoms. If at risk for impaired theophylline clearance or not feasible to monitor serum theophylline concentrations, do not exceed maximum dose of 400 mg/day.
Immediate release (oral solution) (without risk factors for impaired clearance): Initial: 300 mg/day in divided doses every 6 to 8 hours; if tolerated, after 3 days increase to 400 mg/day divided every 6 to 8 hours; if tolerated, after 3 more days increase to 600 mg/day divided every 6 to 8 hours.
Extended release (without risk factors for impaired clearance):
12-hour formulation (tablets): Initial: 300 mg/day in divided doses every 12 hours; if tolerated, after 3 days increase to 400 mg/day in divided doses every 12 hours; if tolerated, after 3 days, increase to 600 mg/day in divided doses every 12 hours
24-hour formulation (capsules and tablets): Initial: 300 to 400 mg once daily; if tolerated after 3 days increase to 400 to 600 mg once daily; if doses >600 mg are needed, titrate according to serum level measurement.
Reversal of dipyridamole- or regadenoson-induced adverse reactions (eg, angina, hypotension) during nuclear cardiac stress testing (alternative agent) (off-label use): IV: 50 mg over 1 minute; may repeat dose if necessary (Johnson 2011; Singleton 2018).
Dosage adjustment based on serum theophylline concentrations: IV, Oral:
<9.9 mcg/mL: If symptoms not controlled and current dosage tolerated, increase dose or infusion rate by ~25%; recheck serum concentration after 24 hours (IV) or 3 days (oral) for further dosage adjustment.
10 to 14.9 mcg/mL: If symptoms controlled and current dose tolerated, maintain dose and recheck serum concentrations at 24-hour intervals (IV) or 6- to 12-month intervals (oral); if symptoms are not controlled and current dose is tolerated, consider adding additional medications.
15 to 19.9 mcg/mL: Consider 10% decrease in dose or infusion rate even if current dosage is tolerated.
20 to 24.9 mcg/mL: Decrease dose or infusion rate by 25% even if no adverse effect present; recheck serum concentrations after 24 hours (IV) or 3 days (oral) to guide further dosage adjustment.
25 to 30 mcg/mL: Stop infusion for 24 hours or skip next oral dose; decrease subsequent doses or infusion rate at least 25% even if no adverse effects present; recheck serum concentrations after 24 hours (IV) or 3 days (oral) to guide further dosage adjustments; if symptomatic, discontinue infusion and consider if overdose treatment is needed.
>30 mcg/mL: Discontinue infusion and treat overdose as indicated; if theophylline is resumed, decrease dose or infusion rate by at least 50% and recheck serum concentrations after 24 hours (IV) or 3 days (oral) to guide further dosage adjustment.
Dosing: Geriatric
Reversible airflow obstruction, acute symptoms:
Loading dose: Oral (immediate release oral solution), IV: Refer to adult dosing.
Maintenance dose: IV: 0.3 mg/kg/hour; maximum: 400 mg/day unless serum levels indicate need for larger dose.
Reversible airflow obstruction, chronic conditions: Oral: Refer to adult dosing. Maximum dose: 400 mg/day (unless symptomatic and the peak steady-state serum theophylline concentration is <10 mcg/mL)
Cardiac decompensation, cor pulmonale, sepsis with multiorgan failure, shock: Refer to adult dosing.
Dosing: Pediatric
Doses should be individualized based on steady-state serum concentrations; theophylline pharmacokinetics have age-dependent factors which may alter required doses particularly in pediatric patients. For obese patients, ideal body weight should be used for dosage calculation.
Acute symptoms; asthma or other chronic lung conditions: Note: Not recommended for the treatment of asthma exacerbations (NAEPP 2007).
Loading dose: Note: Doses presented intended to achieve a serum level of approximately 10 mcg/mL; loading doses should be given intravenously (preferred) or with a rapidly absorbed oral product (not an extended release product). On the average, for every 1 mg/kg theophylline given, blood concentrations will rise 2 mcg/mL.
Patients not currently receiving methylxanthines:
IV: 4.6 mg/kg/dose
Oral: Immediate release product: 5 mg/kg
Patients currently receiving methylxanthines: A loading dose is not recommended without first obtaining a serum theophylline concentration in patients who have received aminophylline or theophylline within the past 24 hours. The loading dose should be calculated as follows:
Dose = (C desired – C measured) (Vd)
C desired = desired serum theophylline concentration
C measured = measured serum theophylline concentration
Maintenance dose: Continuous IV infusion: Note: Dosing presented is to achieve a target concentration of 10 mcg/mL. Lower initial doses may be required in patients with reduced theophylline clearance. Dosage should be adjusted according to serum concentration measurements during the first 12- to 24-hour period.
Infants 4 to 6 weeks: 1.5 mg/kg/dose every 12 hours
Infants 6 to 52 weeks: Dose (mg/kg/hour) = (0.008 X age in weeks) + 0.21
Children 1 to <9 years: 0.8 mg/kg/hour
Children 9 to <12 years: 0.7 mg/kg/hour
Adolescents 12 to <16 years (otherwise healthy, nonsmokers): 0.5 mg/kg/hour; maximum daily dose: 900 mg/day unless serum concentrations indicate need for larger dose
Adolescents 12 to <16 years (cigarette or marijuana smokers): 0.7 mg/kg/hour
Adolescents 16 to 18 years (otherwise healthy, nonsmokers): 0.4 mg/kg/hour; maximum dose: 900 mg/day unless serum concentrations indicate need for larger dose
Cardiac decompensation, cor pulmonale, hepatic dysfunction, sepsis with multiorgan failure, shock: Initial: 0.2 mg/kg/hour; maximum dose: 400 mg/day unless serum concentrations indicate need for larger dose
Chronic conditions, asthma or other chronic lung conditions: Note: Increase dose only if tolerated. Consider lowering dose or using a slower titration if caffeine-like adverse events occur. Smaller doses given more frequently may be used in patients with a more rapid metabolism to prevent breakthrough symptoms which could occur due to low trough concentration prior to the next dose.
Immediate release formulation: Oral: Note: If at risk for impaired clearance or not feasible to monitor serum theophylline concentrations then do not exceed 16 mg/kg/day; maximum daily dose: 400 mg/day
Manufacturer's labeling: Frequency based upon age.
Infants: Total daily dose (mg/day) = [(0.2 x age in weeks) + 5] x (weight in kg); frequency is based on age
Dosing interval:
≤26 weeks: Divide in 3 equal doses and administer every 8 hours
>26 weeks: Divide in 4 equal doses and administer every 6 hours
Children and Adolescents 1 to 15 years and ≤45 kg:
Initial:
Days 1 to 3: 12 to 14 mg/kg/day in divided doses every 4 to 6 hours; maximum daily dose: 300 mg/day
Days 4 to 6: 16 mg/kg/day in divided doses every 4 to 6 hours; maximum daily dose: 400 mg/day
Maintenance: 20 mg/kg/day in divided doses every 4 to 6 hours; maximum daily dose: 600 mg/day
Children and Adolescents >45 kg or Adolescents ≥16 years:
Initial:
Days 1 to 3: 300 mg/day in divided doses every 6 to 8 hours
Days 4 to 6: 400 mg/day in divided doses every 6 to 8 hours
Maintenance: 600 mg/day in divided doses every 6 to 8 hours
Alternate dosing; age-directed (Kliegman 2007):
Children 1 to <9 years: 20 to 24 mg/kg/day; maximum daily dose: 600 mg/day
Children 9 to 12 years: 16 mg/kg/day; maximum daily dose: 600 mg/day
Children and Adolescents >12 to 16 years (nonsmokers): 13 mg/kg/day; maximum daily dose: 600 mg/day
Children >12 years and Adolescents (smokers): 16 mg/kg/day; maximum daily dose: 600 mg/day
Adolescents >16 years (nonsmokers): 10 mg/kg/day; maximum daily dose: 600 mg/day
Extended release formulations: Oral: Note: If at risk for impaired clearance or not feasible to monitor serum theophylline concentrations then do not exceed 16 mg/kg/day; maximum daily dose: 400 mg/day
Manufacturer's labeling:
Children ≥6 years and Adolescents <16 years, weighing ≤45 kg:
Initial:
Days 1 to 3: 12 to 14 mg/kg/day; maximum daily dose: 300 mg/day
Days 4 to 6: 16 mg/kg/day; maximum daily dose: 400 mg/day
Maintenance: 20 mg/kg/day; maximum daily dose: 600 mg/day
Dosing interval (product specific):
12-hour extended release tablets: Children ≥6 years and Adolescents: Divide in 2 equal doses and administer every 12 hours
24-hour extended release tablets: Children ≥12 years and Adolescents: Administer every 24 hours
Children ≥6 years and Adolescents, weighing >45 kg or Adolescents ≥16 years:
12-hour extended release tablets: Children ≥6 years and Adolescents, weighing >45 kg or Adolescents ≥16 years:
Initial:
Days 1 to 3: 300 mg/day in divided doses every 12 hours
Days 4 to 6: 400 mg/day in divided doses every 12 hours
Maintenance: 600 mg/day in divided doses every 12 hours
24-hour extended release tablets: Children ≥12 years and Adolescents, weighing >45 kg or Adolescents ≥16 years:
Initial:
Days 1 to 3: 300 to 400 mg once daily
Days 4 to 6: 400 to 600 mg once daily
Maintenance: Titrate according to serum concentrations
Alternate dosing; age-directed (Kliegman 2007):
Children 6 to <9 years: 20 to 24 mg/kg/day; maximum daily dose: 600 mg/day
Children 9 to 12 years: 16 mg/kg/day; maximum daily dose: 600 mg/day
Children and Adolescents >12 to 16 years (nonsmokers): 13 mg/kg/day; maximum daily dose: 600 mg/day
Children >12 years and Adolescents (smokers): 16 mg/kg/day; maximum daily dose: 600 mg/day
Adolescents >16 years (nonsmokers): 10 mg/kg/day; maximum daily dose: 600 mg/day
Chronic conditions: Oral: Note: Increase dose only if tolerated. Consider lowering dose or using a slower titration if caffeine-like adverse events occur. Smaller doses given more frequently may be used in patients with a more rapid metabolism to prevent breakthrough symptoms which could occur due to low trough concentration prior to the next dose.
Immediate release oral solution: Initial dose: 300 mg/day administered in divided doses every 6 to 8 hours; maintenance: 400 to 600 mg/day (maximum daily dose: 600 mg/day)
Extended release formulations: Initial dose: 300 to 400 mg once daily; maintenance: 400 to 600 mg once daily (maximum daily dose: 600 mg/day)
Dosage adjustment based on serum theophylline concentrations: Infants, Children, and Adolescents: Note: Recheck serum theophylline concentrations after 3 days when using oral dosing, or after 12 hours (children) or 24 hours (adults) when dosing intravenously. Patients maintained with oral therapy should be reassessed at 6- to 12-month intervals, when clinically indicated or if concomitant medication is added which may affect theophylline serum concentration.
<9.9 mcg/mL: If tolerated, but symptoms remain, increase dose by ~25%. Recheck serum theophylline concentrations.
10 to 14.9 mcg/mL: Maintain dosage if tolerated. Recheck serum concentrations at 24-hour intervals (for acute IV dosing) or at 6- to 12-month intervals (for oral dosing).
15 to 19.9 mcg/mL: Consider 10% dose reduction to improve safety margin even if dose is tolerated.
20 to 24.9 mcg/mL: Decrease dose by ~25%. Recheck serum concentrations.
25 to 30 mcg/mL: Skip next dose (oral) or stop infusion for 12 hours (children) or 24 hours (adults) and decrease subsequent doses by at least 25%. Recheck serum concentrations.
>30 mcg/mL: Stop dosing and treat overdose; if resumed, decrease subsequent doses by at least 50%. Recheck serum concentrations.
Extemporaneously Prepared
Note: An alcohol-containing commercial oral solution is available (80 mg/15 mL).
A 5 mg/mL oral suspension may be made with tablets. Crush one 300 mg extended release tablet in a mortar and reduce to a fine powder. Add small portions of a 1:1 mixture of Ora-Sweet® and Ora-Plus® and mix to a uniform paste; mix while adding the vehicle in equal proportions to almost 60 mL; transfer to a calibrated bottle, rinse mortar with vehicle, and add sufficient quantity of vehicle to make 60 mL. Label "shake well". Stable for 90 days at room temperature.
Johnson CE, VanDeKoppel S, and Myers E, "Stability of Anhydrous Theophylline in Extemporaneously Prepared Alcohol-Free Oral Suspensions," Am J Health-Syst Pharm, 2005, 62(23):2518-20.16303910
Administration
IV: Administer loading dose over 30 minutes; follow with a continuous infusion as appropriate. For patients with cor pulmonale, cardiac decompensation, hepatic impairment, the elderly or patients taking drugs that reduce theophylline clearance, the maximum infusion rate should not exceed 17 mg/hour unless patient continues to be symptomatic, steady state serum concentrations is <10 mcg/mL, and serum concentrations can be monitored at 24-hour intervals. Do not administer solutions containing dextrose simultaneously through the same administration set as blood, as this may result in pseudoagglutination or hemolysis.
Oral: Extended release: Administer consistently with or without food (to maintain a consistent drug level); do not chew or crush tablets; may split tablet if scored. An intact matrix tablet may pass in stool.
12-hour formulation: May be administered as once daily dosing in non-smokers (with appropriate total body clearance) and patients with low dosage requirements; consider only after titrated to therapeutic levels. Base once-daily dosing on the twice daily dosing and initiate at the end of the last every 12-hour dosing interval. Once-daily dosing should not be administered at night (after the evening meal).
24-hour formulation: Administer each morning at approximately the same time; avoid administration at night (after the evening meal). Patients who require a high dose (ie, ≥900 mg or 13 mg/kg, whichever is less), should take medication less than 1 hour before a high-fat meal (significant increase in peak serum level and absorption may occur). Patients should consistently take theophylline with food or in fasting state. Twice daily dosing may be considered in patients who metabolize theophylline rapidly (eg, younger patients, smokers, and some nonsmoking adults) and who have symptoms at the end of a dosing interval; administer one dose in the morning and the second dose 10 to 12 hours later (but before the evening meal); avoid administration at night (after the evening meal).
Dietary Considerations
Premixed injection may contain corn-derived dextrose and its use is contraindicated in patients with allergy to corn-related products.
Storage
Capsule: Store below 25°C (77°F).
Elixir, oral solution Store at 25°C (77°F); excursions permitted to 15°C to 30°C (59°F to 86°F); avoid exposure to excessive heat.
Injection: Store at 25°C (77°F). Avoid excessive heat. Brief exposure up to 40°C (104°F) or up to 2 weeks to ultraviolet or fluorescent light does not adversely affect the product. Protect from freezing.
Tablet: Store at 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F).
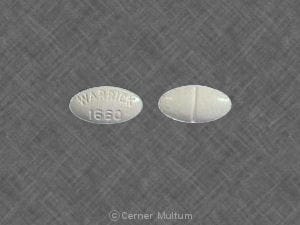
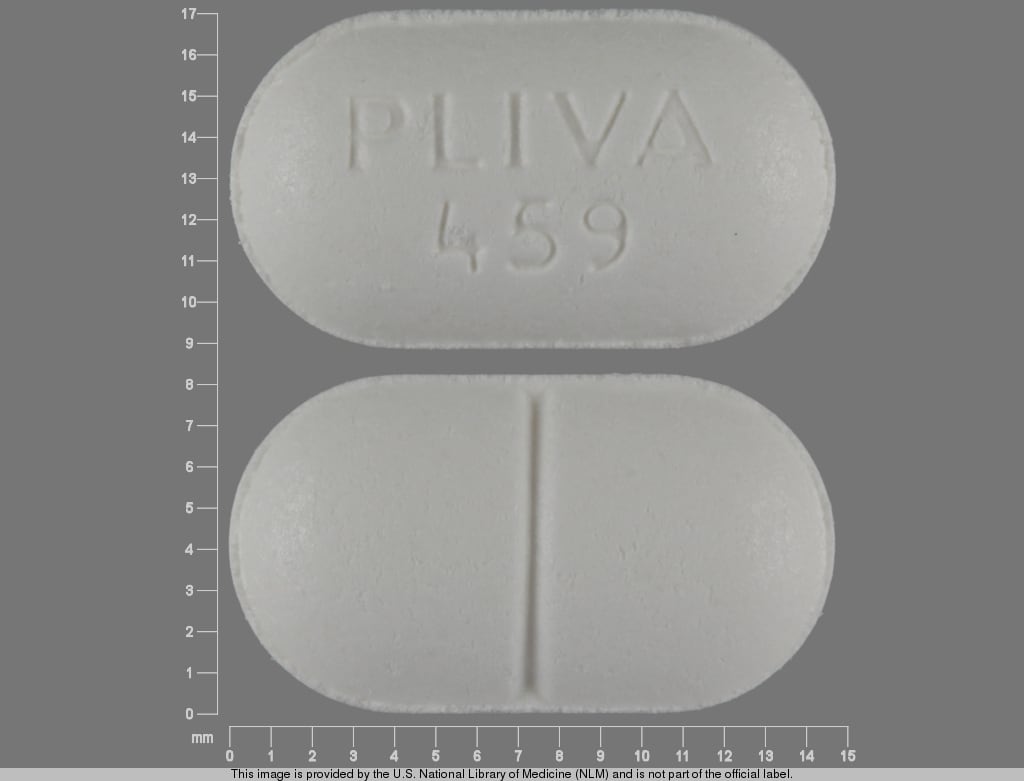
Theophylline Images
Drug Interactions
Acebrophylline: May enhance the stimulatory effect of Theophylline Derivatives. Avoid combination
Adalimumab: May decrease the serum concentration of Theophylline Derivatives. Monitor therapy
Adenosine: Theophylline Derivatives may diminish the therapeutic effect of Adenosine. Consider therapy modification
Alcohol (Ethyl): May increase the serum concentration of Theophylline. Monitor therapy
Allopurinol: May increase the serum concentration of Theophylline Derivatives. Monitor therapy
Amifampridine: Agents With Seizure Threshold Lowering Potential may enhance the neuroexcitatory and/or seizure-potentiating effect of Amifampridine. Monitor therapy
Antithyroid Agents: May increase the serum concentration of Theophylline Derivatives. Monitor therapy
AtoMOXetine: May enhance the hypertensive effect of Sympathomimetics. AtoMOXetine may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Barbiturates: May decrease the serum concentration of Theophylline Derivatives. Monitor therapy
Benzodiazepines: Theophylline Derivatives may diminish the therapeutic effect of Benzodiazepines. Consider therapy modification
Beta-Blockers (Beta1 Selective): May diminish the bronchodilatory effect of Theophylline Derivatives. Management: Monitor for reduced theophylline efficacy during concomitant use with any beta-blocker. Beta-1 selective agents are less likely to antagonize theophylline than nonselective agents, but selectivity may be lost at higher doses. Monitor therapy
Beta-Blockers (Nonselective): May diminish the bronchodilatory effect of Theophylline Derivatives. Monitor therapy
Broccoli: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
BuPROPion: May enhance the neuroexcitatory and/or seizure-potentiating effect of Agents With Seizure Threshold Lowering Potential. Monitor therapy
Cambendazole: May increase the serum concentration of Theophylline Derivatives. Monitor therapy
Cannabinoid-Containing Products: May enhance the tachycardic effect of Sympathomimetics. Exceptions: Cannabidiol. Monitor therapy
Cannabis: May decrease the serum concentration of CYP1A2 Substrates (High risk with Inducers). Monitor therapy
CarBAMazepine: May decrease the serum concentration of Theophylline Derivatives. Theophylline Derivatives may decrease the serum concentration of CarBAMazepine. Management: Seek alternatives to this combination when possible. If these agents are used together, monitor closely for decreased serum concentrations/therapeutic effects of both medications. Consider therapy modification
Cocaine (Topical): May enhance the hypertensive effect of Sympathomimetics. Management: Consider alternatives to use of this combination when possible. Monitor closely for substantially increased blood pressure or heart rate and for any evidence of myocardial ischemia with concurrent use. Consider therapy modification
CYP1A2 Inducers (Moderate): May decrease the serum concentration of Theophylline Derivatives. Monitor therapy
CYP1A2 Inhibitors (Moderate): May increase the serum concentration of Theophylline Derivatives. Management: Consider avoidance of this combination. If coadministration is necessary, monitor for increased theophylline serum concentrations and toxicities when combined. Theophylline dose reductions will likely be required. Consider therapy modification
CYP1A2 Inhibitors (Strong): May increase the serum concentration of Theophylline Derivatives. Management: Consider avoidance of this combination. If coadministration is necessary, consider an empiric theophylline dose reduction to one-third of the original theophylline dose. Monitor for increased theophylline serum concentrations and toxicities when combined. Consider therapy modification
CYP1A2 Inhibitors (Weak): May increase the serum concentration of Theophylline Derivatives. Monitor therapy
Dichlorphenamide: Theophylline may enhance the hypokalemic effect of Dichlorphenamide. Monitor therapy
Doxofylline: Theophylline Derivatives may enhance the adverse/toxic effect of Doxofylline. Avoid combination
Febuxostat: May increase serum concentrations of the active metabolite(s) of Theophylline Derivatives. Specifically, concentrations of 1-methylxanthine, a metabolite of unknown clinical importance, may become elevated. Monitor therapy
Fluconazole: May increase the serum concentration of Theophylline Derivatives. Monitor therapy
Formoterol: Theophylline Derivatives may enhance the adverse/toxic effect of Formoterol. Theophylline Derivatives may enhance the hypokalemic effect of Formoterol. Monitor therapy
Fosphenytoin: May decrease the serum concentration of Theophylline Derivatives. Theophylline Derivatives may decrease the serum concentration of Fosphenytoin. Management: Seek alternatives when possible. If used together, monitor for decreased concentrations/effects of phenytoin or theophylline if the other agent is initiated/dose increased, or increased concentrations/effects if the other is discontinued/dose decreased. Consider therapy modification
Guanethidine: May enhance the arrhythmogenic effect of Sympathomimetics. Guanethidine may enhance the hypertensive effect of Sympathomimetics. Monitor therapy
Indacaterol: Theophylline Derivatives may enhance the adverse/toxic effect of Indacaterol. Theophylline Derivatives may enhance the hypokalemic effect of Indacaterol. Monitor therapy
Iohexol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iohexol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iohexol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iomeprol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iomeprol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iomeprol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Iopamidol: Agents With Seizure Threshold Lowering Potential may enhance the adverse/toxic effect of Iopamidol. Specifically, the risk for seizures may be increased. Management: Discontinue agents that may lower the seizure threshold 48 hours prior to intrathecal use of iopamidol. Wait at least 24 hours after the procedure to resume such agents. In nonelective procedures, consider use of prophylactic anticonvulsants. Consider therapy modification
Isoniazid: May increase the serum concentration of Theophylline Derivatives. Monitor therapy
Isoproterenol: May decrease the serum concentration of Theophylline Derivatives. Monitor therapy
Linezolid: May enhance the hypertensive effect of Sympathomimetics. Management: Reduce initial doses of sympathomimetic agents, and closely monitor for enhanced pressor response, in patients receiving linezolid. Specific dose adjustment recommendations are not presently available. Consider therapy modification
Lithium: Theophylline Derivatives may decrease the serum concentration of Lithium. Monitor therapy
Macrolide Antibiotics: May decrease the metabolism of Theophylline Derivatives. Exceptions: Azithromycin (Systemic); Fidaxomicin; Roxithromycin; Spiramycin; Telithromycin. Consider therapy modification
Methacholine: Theophylline may diminish the therapeutic effect of Methacholine. Management: Hold theophylline for 12 to 48 hours before methacholine use. Consider therapy modification
Methotrexate: May increase the serum concentration of Theophylline Derivatives. Monitor therapy
Metreleptin: May decrease the serum concentration of Theophylline. Metreleptin may increase the serum concentration of Theophylline. Monitor therapy
Olodaterol: Theophylline Derivatives may enhance the adverse/toxic effect of Olodaterol. Theophylline Derivatives may enhance the hypokalemic effect of Olodaterol. Monitor therapy
Pancuronium: Theophylline Derivatives may enhance the adverse/toxic effect of Pancuronium. Theophylline Derivatives may diminish the neuromuscular-blocking effect of Pancuronium. Management: Pancuronium dosage adjustment may be necessary to induce paralysis in patients receiving concomitant theophylline derivatives. Monitor closely for adverse effects (e.g., cardiac effects) with concomitant use of these agents. Consider therapy modification
Pentoxifylline: May increase the serum concentration of Theophylline Derivatives. Monitor therapy
Phenytoin: May decrease the serum concentration of Theophylline Derivatives. Theophylline Derivatives may decrease the serum concentration of Phenytoin. Management: Seek alternatives when possible. If used together, monitor for decreased concentrations/effects of phenytoin or theophylline if the other agent is initiated/dose increased, or increased concentrations/effects if the other is discontinued/dose decreased. Consider therapy modification
QuiNINE: May increase the serum concentration of Theophylline Derivatives. Monitor therapy
Quinolones: May decrease the metabolism of Theophylline Derivatives. Ciprofloxacin and enoxacin are of greatest concern. Theophylline/quinolone therapy might augment the seizure-producing potential of each of the individual agents. Exceptions: Delafloxacin; Gemifloxacin; LevoFLOXacin (Systemic); Lomefloxacin; Moxifloxacin (Systemic); Nalidixic Acid; Pefloxacin; Sparfloxacin. Consider therapy modification
Regadenoson: Theophylline may diminish the vasodilatory effect of Regadenoson. Consider therapy modification
Riociguat: Theophylline Derivatives may enhance the hypotensive effect of Riociguat. Avoid combination
Ritonavir: May decrease the serum concentration of Theophylline Derivatives. Monitor therapy
Solriamfetol: Sympathomimetics may enhance the hypertensive effect of Solriamfetol. Monitor therapy
Sulfinpyrazone: May decrease the serum concentration of Theophylline Derivatives. Monitor therapy
Sympathomimetics: May enhance the adverse/toxic effect of other Sympathomimetics. Monitor therapy
Tedizolid: May enhance the hypertensive effect of Sympathomimetics. Tedizolid may enhance the tachycardic effect of Sympathomimetics. Monitor therapy
Thyroid Products: May increase the metabolism of Theophylline Derivatives. Monitor therapy
Tobacco (Smoked): May decrease the serum concentration of Theophylline Derivatives. Monitor therapy
Verapamil: May increase the serum concentration of Theophylline Derivatives. Monitor therapy
Zafirlukast: Theophylline Derivatives may decrease the serum concentration of Zafirlukast. Zafirlukast may increase the serum concentration of Theophylline Derivatives. Monitor therapy
Test Interactions
Plasma glucose, uric acid, free fatty acids, total cholesterol, HDL, HDL/LDL ratio, and urinary free cortisol excretion may be increased by theophylline. Theophylline may decrease triiodothyronine.
Adverse Reactions
Frequency not defined. Adverse events observed at therapeutic serum levels.
Cardiovascular: Cardiac flutter, tachycardia
Central nervous system: Headache, hyperactivity (children), insomnia, restlessness, seizure, status epilepticus (nonconvulsive)
Endocrine & metabolic: Hypercalcemia (with concomitant hyperthyroid disease)
Gastrointestinal: Gastroesophageal reflux (aggravation), gastrointestinal ulcer (aggravation), nausea, vomiting
Genitourinary: Difficulty in micturition (elderly males with prostatism), diuresis (transient)
Neuromuscular & skeletal: Tremor
Warnings/Precautions
Concerns related to adverse effects:
- Theophylline toxicity: Severe and potentially fatal theophylline toxicity may occur if reduced theophylline clearance occurs. Theophylline clearance may be decreased in patients with acute pulmonary edema, heart failure, cor pulmonale, fever (≥102°F for ≥24 hours or lesser temperature elevations for longer periods), hepatic disease, acute hepatitis, cirrhosis, hypothyroidism, sepsis with multiorgan failure, shock, neonates (term and premature), infants <3 months of age with decreased renal function, infants <1 year of age, elderly >60 years of age, and patients following cessation of smoking. Consider benefits versus risks and the need for more intensive monitoring in these patients; reduced infusion rate required. If a patient develops signs and symptoms of theophylline toxicity (eg, nausea or persistent, repetitive vomiting), a serum theophylline level should be measured immediately and subsequent doses withheld.
Disease-related concerns:
- Cardiovascular disease: Use with caution in patients with cardiac arrhythmias (excluding bradyarrhythmias); use may exacerbate arrhythmias.
- Cystic fibrosis: Use with caution in patients with cystic fibrosis; increased theophylline clearance may occur.
- Hepatic impairment: Use with caution in patients with hepatic impairment (eg, cirrhosis, acute hepatitis, cholestasis); risk of severe and potentially fatal theophylline toxicity is increased; theophylline clearance is decreased ≥50% in these patients. Dose reduction and frequent monitoring of serum theophylline concentration are required.
- Hyperthyroidism: Use with caution in patients with hyperthyroidism; increased theophylline clearance may occur.
- Peptic ulcer disease: Use with caution in patients with active peptic ulcer disease; use may exacerbate peptic ulcer.
- Seizure disorder: Use with caution in patients with seizure disorders; use may exacerbate seizure disorder.
Concurrent drug therapy issues:
- Drug-drug interactions: Potentially significant interactions may exist, requiring dose or frequency adjustment, additional monitoring, and/or selection of alternative therapy. Consult drug interactions database for more detailed information.
Special populations:
- Elderly: Use extreme caution in the elderly; these patients are at greater risk of serious theophylline toxicity.
- Pediatric: Select dose with caution and with frequent monitoring of concentrations (especially <1 year); rate of clearance is highly variable in these patients.
Dosage form specific issues:
- Propylene glycol: Some dosage forms may contain propylene glycol; large amounts are potentially toxic and have been associated hyperosmolality, lactic acidosis, seizures, and respiratory depression; use caution (AAP 1997; Zar 2007).
Other warnings/precautions:
- Appropriate use: Do not increase dose in response to acute exacerbation of symptoms unless steady state serum theophylline concentration is <10 mcg/mL. As the rate of theophylline clearance may be dose-dependent, an increase in dose based upon a subtherapeutic serum concentration measurement should be limited to ~25% increase of the previous infusion rate or daily dose.
Monitoring Parameters
Heart rate, CNS effects (insomnia, irritability); respiratory rate (COPD patients often have resting controlled respiratory rates in low 20s); arterial or capillary blood gases (if applicable); fluid balance, electrolyte concentrations, and acid-base balance during prolonged IV therapy.
Theophylline levels: Serum theophylline levels should be monitored after initiation of therapy, prior to making dose increases; in the presence of signs or symptoms of toxicity; or when a new illness, worsening of a present illness, or change in patient's treatment regimen occur that may alter theophylline clearance (eg, fever >102°F or sustained for 24 hours or more, hepatitis, or drugs that are added or discontinued).
Oral: Monitor serum concentrations at 6 month intervals for rapidly growing children and at yearly intervals for all others (if symptoms are well controlled).
IV:
Loading dose: Measure serum concentrations 30 minutes after the end of an IV loading dose in patients who have received no theophylline in the previous 24 hours to determine the need for an additional loading (serum concentration <10 mcg/mL) or to delay starting the constant IV infusion (serum concentration >20 mcg/mL).
Infusion: Measure serum concentrations one expected half-life (eg, ~4 hours in children 1 to 9 years of age or 8 hours in nonsmoking, otherwise healthy adults) after starting a continuous infusion, then every 12 to 24 hours to determine if further adjustments are necessary, and then at 24 hour intervals for duration of infusion.
Pregnancy
Pregnancy Risk Factor
C
Pregnancy Considerations
Adverse effects have been observed in animal reproduction studies. Theophylline crosses the placenta; adverse effects may be seen in the newborn. Use is generally safe when used at the recommended doses (serum concentrations 5 to 12 mcg/mL) however maternal adverse events may be increased and efficacy may be decreased in pregnant women. Theophylline metabolism may change during pregnancy; the half-life is similar to that observed in otherwise healthy, nonsmoking adults with asthma during the first and second trimesters (~8.7 hours), but may increase to 13 hours (range: 8 to 18 hours) during the third trimester. The volume of distribution is also increased during the third trimester. Monitor serum levels. The recommendations for the use of theophylline in pregnant women with asthma are similar to those used in nonpregnant adults (National Heart, Lung, and Blood Institute Guidelines 2004).
Patient Education
What is this drug used for?
- It is used to treat breathing problems.
- This drug is not to be used to treat intense flare-ups of shortness of breath. Use a rescue inhaler. Talk with the doctor.
Frequently reported side effects of this drug
- Agitation
- Diarrhea
- Tablet shell in stool
- Passing a lot of urine
Other side effects of this drug: Talk with your doctor right away if you have any of these signs of:
- Low potassium like muscle pain or weakness, muscle cramps, or an abnormal heartbeat.
- High blood sugar like confusion, fatigue, increased thirst, increased hunger, passing a lot of urine, flushing, fast breathing, or breath that smells like fruit.
- Acidosis like confusion, fast breathing, fast heartbeat, abnormal heartbeat, severe abdominal pain, nausea, vomiting, fatigue, shortness of breath, or loss of strength and energy.
- Nausea
- Vomiting
- Fast heartbeat
- Abnormal heartbeat
- Severe dizziness
- Passing out
- Severe anxiety
- Tremors
- Severe headache
- Confusion
- Trouble sleeping
- Seizures
- Behavioral changes
- Irritability
- Muscle spasm
- Signs of a significant reaction like wheezing; chest tightness; fever; itching; bad cough; blue skin color; seizures; or swelling of face, lips, tongue, or throat.
Note: This is not a comprehensive list of all side effects. Talk to your doctor if you have questions.
Consumer Information Use and Disclaimer: This information should not be used to decide whether or not to take this medicine or any other medicine. Only the healthcare provider has the knowledge and training to decide which medicines are right for a specific patient. This information does not endorse any medicine as safe, effective, or approved for treating any patient or health condition. This is only a brief summary of general information about this medicine. It does NOT include all information about the possible uses, directions, warnings, precautions, interactions, adverse effects, or risks that may apply to this medicine. This information is not specific medical advice and does not replace information you receive from the healthcare provider. You must talk with the healthcare provider for complete information about the risks and benefits of using this medicine.